Insulin Bolus in Diabetic Ketoacidosis
Received: 01-Mar-2024 / Manuscript No. jdce-24-130721 / Editor assigned: 04-Mar-2024 / PreQC No. jdce-24-130721 (PQ) / Reviewed: 18-Mar-2024 / QC No. jdce-24-130721 / Revised: 22-Mar-2024 / Manuscript No. jdce-24-130721 (R) / Published Date: 29-Mar-2024 DOI: 0.4172/jdce.1000242
Abstract
Idiopathic hypoglycemia, characterized by recurrent episodes of low blood sugar without an apparent underlying cause, remains a perplexing and challenging medical condition. Despite extensive research in the field of endocrinology and metabolism, the etiology and mechanisms driving this enigmatic disorder continue to elude comprehensive understanding. This review aims to provide an updated overview of idiopathic hypoglycemia, shedding light on its clinical manifestations, diagnostic challenges, and potential pathophysiological mechanisms.
Keywords
Diabetic ketoacidosis (DKA); Insulin bolus; Insulin infusion; Priming dose; Hyper/Hypo/Normoglycemia.
Background
DKA is one of the common presentations in the emergency and is
managed well by ED, critical care and acute care physicians. There are
lot of controversies regarding its plan of management. One of the big
controversies is that of bolus of insulin vs infusion. There is ongoing
controversy about the use of an initial bolus of 0.1 U/kg IV followed
by an infusion. However, others disagree and say it carries risks when
compared to an insulin infusion alone. There is always significant
difference on this issue within my hospital as well. As one physician
might administer a bolus initially, but the patient may be followed by
another physician who might have a different thought process and
belief. This is the reason for selection of this topic as it interests me and
I intend to workup and appraise the literature.
Introduction
Diabetes mellitus is one of the challenging medical problems around the world and is being given a lot of attention by the governments around the world. In this regard sometimes, the diabetic patients can face an emergency related to this condition known as Diabetic Ketoacidosis (DKA). Diabetic ketoacidosis (DKA) is one of the common endocrinological emergencies presenting to the Emergency department. It presents a huge challenge for emergency physicians and to the critical care physicians in treating these patients. It presents as a combination of hyperglycaemia, ketosis, and metabolic acidosis [1]. The pathology in this condition is relative or absolute deficiency of insulin and also an excess of counter-regulatory hormones including glucagon, cortisol, catecholamines, and growth hormones which can lead to triad of hyperglycaemia, glycosuria, dehydration, and hyperosmolarity [2]. Glycosuria can also cause an osmotic diuresis, which can result in dehydration and also lead to imbalance of electrolytes including sodium, potassium, calcium, magnesium, chloride, and phosphate. This condition can lead to hypertonicity and also cause a shifting of water from the intracellular space to the hypertonic extracellular space. This will cause a potassium efflux from the intracellular space, and can be aggravated by acidosis, lack of effective insulin action, and also breakdown of intracellular proteins [3].
Despite the new ways of treating this condition, there are lot of increasing number of hospital admissions for this endocrine medical emergency DKA and hyperosmolar hyperglycaemic state (HHS) [4,5]. It can also have high mortality rates like as high as 5–9% in the elderly and especially in patients with multiple comorbidities [6]. Diabetic ketoacidosis can also lead to multiple other associated medical conditions because it can cause Hyper coagulable state. It can be a threat to the patient by making him/her highly hypercoagulable because of which patient can suffer from the worse medical life-threatening complications like Cerebrovascular accident (CVA), Acute coronary syndrome, Pulmonary embolism, Deep vein thrombosis (DVT) and also Disseminated intravascular coagulation [7].
As discussed earlier, there is a significant controversy among the treating physicians like Emergency and critical care physicians in the initial management which is either we should use insulin bolus followed by infusion or we should use infusion alone. Which is the best or both are same, it has been always a matter of controversy and can lead to multiple change in treatments when treated by different physicians. We do not have any very good data supporting the initial insulin bolus prior to the initiation of insulin infusions. We always as treating physicians bank on thought that the logical basis for using a bolus insulin is to overcome the relative insulin deficiency which is seen in DKA to cause suppression of lipolysis and hepatic gluconeogenesis and which can limit further worsening of acidosis. However, we may find that insulin boluses may lead to more harm which includes causing hypoglycaemia, hypokalaemia, and if we bring glucose levels down too rapidly, it will lead to another complication to the patient like cerebral oedema particularly in the younger patients. We still find big differences in different guidelines. The American diabetes association has incorporated bolus in their guidelines released by them in 2009 but on the contrary we do not see any bolus in NICE [8,9].
Historically from the 1980, Insulin bolus was considered a choice before infusion because one study which showed in a paediatric patient using a dosing regimen of 0.1U/kg/hr. without using a loading dose that resulted in a total plasma insulin level of 50-60μU/ml [10]. This level was found not enough to suppress gluconeogenesis, lipolysis and also acidosis.
The effectiveness of low dose insulin without using a bolus insulin has not been established in a prospective randomized study.
Objective
The objective of this CTR is to answer a question. The best way to formulate a clinical question is to prepare a 3- or 4-part question. This is based on format of population involved, intervention and comparison and lastly the outcome.
The 3-part question is as follows:
In [adult patients with diabetic ketoacidosis], does [an initial bolus of insulin result in faster, safer restoration of normoglycemia and pH] which effect mortality when compared [with no bolus prior to commencing continuous insulin infusion]?
P- Population - adult patients with diabetic ketoacidosis
I-Intervention - an initial bolus of insulin
C-Comparison - No bolus prior to commencing continuous insulin infusion i.e. only infusion of insulin
O-Outcome - Primary: Mortality within 14 days of hospital admission; Secondary: Morbidity (measured by length of stay in hospital, occurrence of hypoglycaemia and electrolyte abnormalities, length of stay in the hospital
Literature Search
The literature search was done on 12th January 2023 and repeated several times before the final submission.
Inclusion criteria
• Adult patients with DKA
• Treatment with insulin bolus and or infusion
• Articles in English
Exclusion criteria
• Case reports
• Case series
• Subcutaneous insulin regimes (Table 1)
| Recent queries in PubMed | |||
|---|---|---|---|
| Search | Query | Items found | Time |
| #7 | Search ((((Diabetic ketoacidosis) OR DKA) AND insulin bolus) OR priming dose) OR priming bolus Filters: Clinical Trial; Humans Sort by: [pubsolr12] | 657 | 03:23:03 |
| #6 | Search ((((Diabetic ketoacidosis) OR DKA) AND insulin bolus) OR priming dose) OR priming bolus Filters: Clinical Trial; Humans | 652 | 02:55:01 |
| #5 | Search ((((Diabetic ketoacidosis) OR DKA) AND insulin bolus) OR priming dose) OR priming bolus Filters: Clinical Trial | 667 | 02:54:54 |
| #4 | Search ((((Diabetic ketoacidosis) OR DKA) AND insulin bolus) OR priming dose) OR priming bolus | 4659 | 02:54:45 |
Table 1: Search strings.
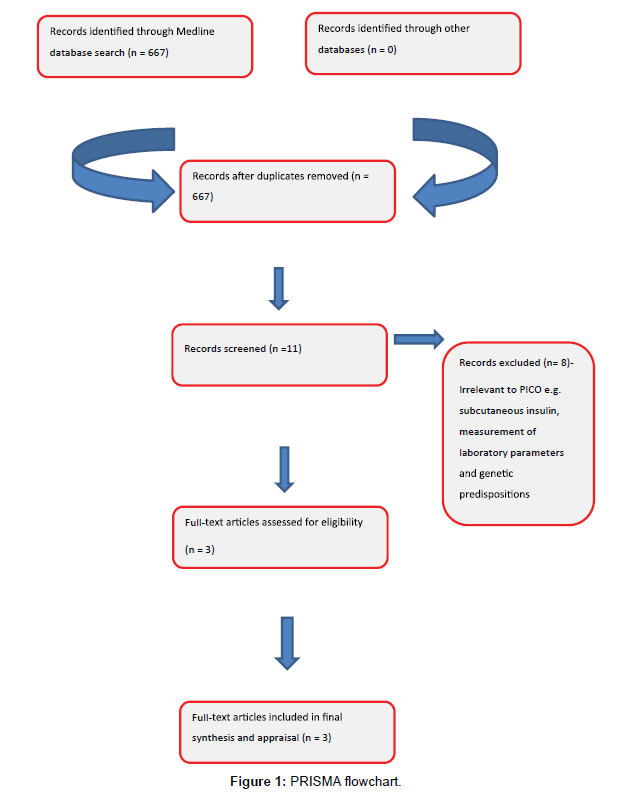
667 articles were screened for their title and only 3 were included in the final appraisal as they best matched the 3-part question. Indirect evidence and review articles were not appraised. Reasons for exclusion were:
• Different doses of insulin used
• Human insulin tested against analogs
• Oral medications used along with insulin
• IV tested against subcutaneous
The 3 articles included in the final appraisal were;
• Is a Priming Dose of Insulin Necessary in a Low-Dose Insulin Protocol for the treatment of Diabetic Ketoacidosis? [11] Abbas E. Kitabchi, PHD, MD.
• Insulin therapy for DKA – Bolus vs infusion. Eryn K Butkiewicz, BA.
• Goyal et al [12]
Other portals were searched and the results are as follows;
• GOOGLE SCHOLAR: None
• Manual search of journals: None
• BESTBETS.ORG: None
• Bibliographies of the relevant articles and review articles:
None (Figure 1)
Appraisal of Literature
Butkiewicz et al.
This study was published in Journal of Diabetes care of American Diabetes association in 1995. It was a Retrospective cohort study. This study was done in a big tertiary care centre. The study was done retrospectively and the researchers reviewed and randomized the complete medical records of all patients of diabetes among Rochester, Minnesota, local residents from the year 1950 to 1989. They went through past patients records with a discharge diagnosis of DKA. Every past data which was taken out were randomized to either bolus insulin infusion group (BII) or continuous insulin infusion group (CII). The researchers found among the diabetes patients that there were 59 cases with confirmed first episodes of DKA between the years 1950-1992. Among the 30 patients 29 were treated with BII and these all cases were treated before 1970. In the 29 patients of DKA who were treated with CII were admitted between year 1976 and 1992.
In detail the basic characteristics like demographics and age at the presentation of DKA among these patients were totally similar for the two groups included in the study. When compared, the proportion of obese individuals was higher in continuous infusion group along with proportion of DKA, this represents the temporal trend observed in Rochester population cohort. The BII cases were treated before 1970 and the CII were admitted between 1976 and 1992 and the number of more obese patients were in CII and this was because obesity has increased over time. It implies that increase in the obesity in US population over the period and the association of obesity with DKA. Studies have proven that obese patients have poor glucose control which can result in higher incidences of DKA [13].
When comparing the mean quantity of insulin administered it was higher in the BII group as compared to the centre CII group (179 ± 140 and 99 ± 70 U, P< 0.006). One of the problems was that the episodes of hypoglycaemia occurred more frequently in the BII group than in the CII group (BII = 8/30, CII = 1/29; P = 0.03). The P value was significant in terms of event of hypoglycaemia. But when comparing the rest of variables like hypokalaemia, neurological deficit, myocardial arrhythmia, or mortality, it did not differ significantly between groups.
It was indeed the first study of this kind which involved studying directly bolus versus infusion of insulin in the management of DKA.
But it had definitely number of limitations like the number of participants which was limited when considering the time duration of this study. Such a study is limited because of its selection bias. Selection of medical records was retrospective which makes subjectivity come into play.
Another limitation was that it was from a single centre, retrospective with a small cohort of patients. The outcomes did not measure what is truly clinically relevant to an ED physician as they measured surrogate markers.
Because of limitations associated with this study including retrospective nature, small sample size, selection bias and surrogate markers. So, in terms of its generalizability and applicability to larger population especially the one here in our hospital it cannot be effectively applied.
However, the positive aspect of this study is that it retrospectively confirmed that using of continuous insulin infusion is associated with less episodes of hypoglycaemia (Table 2).
| Study | Type | Patient Cohort | Outcomes/Results | Comments | Oxford level of evidence |
|---|---|---|---|---|---|
| Butkiewicz et al | Retrospective Randomized | Bolus group (BII)-30 | Higher glucose values (BII=24.9±8.5 mmol/l; P=0.002) | Novel | 2C |
| Retrospective and single centre | |||||
| Continuous infusion (CII)-29 | Hypoglycemia (BII=8/30, CII-1/29; P=0.03) | 90% of subjects that received bolus were before 1970 which shows a trend which is changing | |||
| Infusion group had fewer episodes of hypoglycemia |
Kitabchi et al.
Table 2: Study Characteristics (Butkiewicz et al).
This is an RCT conducted in 2007 in the Emergency department of a single centre in US and published in 2008. This study was a prospective study fully randomized, single centre trial which was having 38 patients with DKA. The patients who were diagnosed as DKA in ED department were shifted to research centre. Total of 38 patients were randomized after they were transferred from the ED to the research centre. In terms of management every group received the same therapy apart from the interventions which was being studied. In terms of design the participants were then assigned to either of the group. There were three groups one was Load group another was No Load group and the third one was Twice no-load group. The participants were then assigned to one of the groups as:
• 12 patients were put in the Load group who received a loading dose of insulin at 0.07U/kg of Body weight and then followed by an infusion of 0.07U/kg Body wt./hr.
• The group which was a No-Load group had 12 patients, who received only an intravenous infusion of insulin at a dose of 0.07U/kg Body weight/h without any loading dose.
• Among the Twice No-Load group an infusion of insulin in 13 patients at a dose of 0.14U/kg /h of insulin without a bolus dose was started and given.
The total response of the patient to the therapy was ultimately based on the time to achieve a glucose level of ≤ 250 mg/dL, bicarbonate of >15mEq/L and pH ≥ 7.3.
The blood tests sent to the laboratory for investigations included the following: complete blood count, venous blood glucose level and routine blood chemistries which were measured by standard assay in the clinical chemistry laboratory in the centre. The other tests which were measured were the plasma free insulin, C-peptide, beta hydroxybutyrate (βOHB), acetoacetate, pyruvate, lactate, cortisol, and free fatty acids. The Glucose was checked and measured by a glucose oxidase method using a Beckman Glucose Analyzer. Plasma free insulin along with C-peptide were both measured following polyethylene glycol precipitation by a double antibody radioimmunoassay method.
In terms of population in all these groups, the majority of patients belonged to African American population. There was no genetic or gender predominance and these differences do not represent the true cohort of DKA patients.
While going through the details of the results it did not show any significant differences in when it comes to outcomes of any groups apart from some biochemical assays which actually are not part of my study question and doesn’t seem to impact at all patient oriented outcome.
In terms of Limitations in the study following were the flaws which I will be discussing next although it is one of the only three studies addressing my question.
First were methodological concerns. Although it was randomized, there is no clear mention of concealment which is very important and what was the type of randomization and no mention of blinding.
It was a single centre trial and had higher male population with small cohort of patients. There was also no mention of about risk of bias assessment. In terms of application of results in my institution, the articles results cannot be generalizable due to above reasons and more methodologically sound study needs to be carried out to answer the question.
But what important about this study can be said is that bolus dose of insulin doesn’t seem to add any advantage in patient-oriented outcomes (Table 3).
| Study | Type | Patient Cohort | Outcomes/Results | Comments | Oxford level of evidence |
|---|---|---|---|---|---|
| Kitabchi et al., 2008 | Randomized control trial | Load group-12 | Time to achieve glucose level of ≤250 mg/Dl, bicarbonate of >15mEq/L and pH ≥ 7.3 | No mention of concealment, type of randomization and binding | 2B |
| No Load group-12 | It’s a small cohort of patients (all are African American) | ||||
| Laboratory values analyzed | A single center | ||||
| Double load group-13 | No mention of risk of bias assessment | ||||
| No differences in outcomes | Outcomes were biochemical assays which don’t reflect clinical practice and are not applicable |
Table 3: Study Characteristics (Kitabchi et al., 2008).
Goyal et al.
Nikhil Goyal and his colleagues had published this study in 2007 in the Journal of emergency medicine. It was non-concurrent, prospective, observational cohort study. This study was done by including the electronic charts of the patients who were labelled a diagnosis of DKA, Ketoacidosis or metabolic acidosis upon admission from the Emergency department (ED). The parameters which the investigators looked in to the electronic chart were glucose level via the central laboratory or bed side point-of-care testing, anion gap determination, insulin administration, D50 administration and how much intravenous fluid was administered. The investigators did the chart review and it was limited to the emergency department time course and along with that laboratory tests checked within 2 h of departure from the ED. Regarding the baseline data which includes prior history of diabetes mellitus, insulin or oral hypoglycaemic agent usage by patient before arrival to ED and the type of diabetes patient was suffering were extracted from prior medical records.
This study was approved by Institutional review board after taking their Prior approval.
Many steps were undertaken to makes this study powerful like one of that was equivalence testing which was done to make results more clinically relevant.
In this study the most important primary outcome of interest was the incidence of hypoglycaemia. There were other end points which included like:
• Any need for IV fluid change
• what was the rate of decrease in serum glucose and anion gap levels
• Total length of stay in the Emergency department and in the hospital.
This study was having two groups named bolus group and infusion group and in them 78 charts were included in the bolus group and 79 were included in the infusion group.
It was observed in this study that more charts in the bolus group had developed hypoglycaemia which was five patients which amounted to 6% as when compared to the control group which was one patient which was only 1%. Exact time period of the bolus administration and hypoglycaemic episode were not mentioned.
When it comes to the statistical difference, it was not found to be having any significant difference as the p value of the comparison was 0.12.
In terms of the relative risk of hypoglycaemia in the bolus group which was 5.06
(95% CI 0.61-42.36). Although 5.06 apparently seems significant however the wide confidential interval contradicts it.
This study had limitations. First this study was a prospective nonrandomized study which is a limitation and regarding the option of bolus of insulin which was alone at the discretion of the emergency physician may have led to intervention bias.
This explains that there was set protocol followed and the risk of bias comes into play. When it comes to similarity between the two groups, they were similar in terms of other treatment modalities and baseline characteristics.
The detailed chart review was done only from the emergency department perspective however it would had been more meaningful if the investigators would have looked them in relation to length of hospital stay, mortality and complications.
From the point of view of my institution applicability length of stay in ED would have been interesting outcome (Table 4).
| Study | Type | Patient Cohort | Outcomes/Results | Comments | Oxford level of evidence |
|---|---|---|---|---|---|
| Goyal et al., 2007 | Prospective observational study | 78 bolus group | Glucose levels, anion gap determination, insulin administration, D50 administration | High risk of bias | 2C |
| 79 infusion group | Hypoglycemia (p-value of the comparison was 0.12). RR 5.06 (95% CI 0.61-42.36) | Patient relevant outcomes weren’t measured like mortality and length of stay | |||
| Protocol was applied as per physician discretion. |
Table 4: Study characteristics (Goyal et al., 2007)
Discussion
Only three studies addressed my search question. The use of Bolus insulin has been controversial. The logical basis behind the use of bolus insulin in treatment of DKA is not clear. Since the invention of insulin in 1922, it has rapidly become the treatment of choice for management Study Type Patient Cohort Outcomes/Results Comments Oxford level of evidence
Table 4: Study characteristics (Goyal et al., 2007). of DKA [14]. It has been found by the later research studies that larger doses of insulin were more effective. In 1970 some studies proposed that the more “physiologic” 0.1units/kg/h dose was very effective in the management of DKA. In the after years some randomized controlled studies proved that by using the same dose of insulin will be having lesser incidence of hypoglycaemia and also with similar rates of resolution of hyperglycaemia and ketosis. Thus, being safer way of treating DKA patients. In 1977 a revolutionary randomized trial looked at three pathways of insulin administration that is IV, SC, and intramuscular (IM) administration of insulin utilizing a bolus “primer” dose followed by an infusion. It has always been a big question that whether bolus dose of insulin really provides any extra benefit when the real priority is fluid and electrolyte management in DKA [15].
There has been a paediatric literature which seems to recognize this and now with American diabetes association and the European society for paediatric endocrinology guidelines also recommending that an Intravenous infusion of insulin without the bolus dose of insulin is the better way of managing DKA.
On the contrary the American diabetes association guidelines is still recommending the use of bolus insulin dose before starting insulin infusion for treating adult patients with DKA with no obvious justification and merely based on expert opinion [16].
From the three articles that were appraised above, it is still unclear if insulin bolus before an infusion is of any benefit.One of them only is a prospectively randomized study which shows no differences in outcomes. It is certainly studied on a small cohort of patients and has methodological flaws. The aim is to give insulin in a way that leads to near physiological circulating levels of around 150 – 200 microunits/ ml in the form of a plateau. A bolus does lead to a high peak insulin level but with a low plateau. With an infusion rate of around 0.14 units/ kg, the patient will reach a steady plateau state that is near the normal circulating level.
More relevantly, Goyal et al found no difference in glucose change or anion gap change in the patients who received a bolus of insulin followed by an infusion. There was some difference in hypoglycaemia episode favouring CII however it was not statistically significant [17].
Conclusion
From the literature search and appraisal of best available articles the effectiveness and risks associated with a bolus of regular intravenous insulin is lacking. At this point of time, we don’t have enough evidence to favour or dismiss the use of bolus insulin in DKA patients. There was a concern regarding the episodes of hypoglycaemia with bolus insulin but it was statistically insignificant. Further research is needed to be carried in future to look for effectiveness of bolus insulin.
Recommendation
The American diabetes association guidelines is still recommending the use of bolus insulin dose before starting insulin infusion for treating adult patients with DKA. In my EBCTR I have not found the strong evidence favouring against use of bolus insulin infusion. So, I would like to recommend it as an option till further evidence is available either supporting or not favouring it. Larger scale randomized controlled trials are to be conducted to answer the question.
References
- Malik, WA (2016) Audit on biacrbonate use in DKA. Doha: yet to be published.
- Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN (2009) Hyperglycemic crises in adult patients with diabetes. Diabetes care 32:1335-1343.
- Nyenwe EA, Kitabchi AE (2016) The evolution of diabetic ketoacidosis: an update of its etiology, pathogenesis and management. Metabolism 65:507-521.
- Blumer C, Prescott V, Senes S, Australian Institute of H, Welfare (2012) Diabetes among young Australians. Canberra: Australian Institute of Health and Welfare.
- Dhatariya K, Savage M (2013) The management of diabetic ketoacidosis in adults. UK: Joint British Diabetes Society
- Azevedo LC, Choi H, Simmonds K, Davidow J, Bagshaw SM, et al. (2014) Incidence and long-term outcomes of critically ill adult patients with moderate-to-severe diabetic ketoacidosis: retrospective matched cohort study. Journal of critical care 29:971-977.
- Carr ME (2001) Diabetes mellitus: a hypercoagulable state. Journal of Diabetes and its Complications 15:44-54.
- National Clinical Guideline Centre for A, Chronic C, National Institute for H, Care E (2015) Type 1 diabetes in adults: diagnosis and management.
- Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, et al. (2001) Management of hyperglycaemic crises in patients with diabetes. Diabetes care 24:131-153.
- Burghen GA, Etteldorf JN, Fisher JN, Kitabchi AQ (1980) Comparison of high-dose and low-dose insulin by continuous intravenous infusion in the treatment of diabetic ketoacidosis in children. Diabetes care 3:15-20.
- Kitabchi AE, Murphy MB, Spencer J, Matteri R, Karas J, et al. (2008) Is a priming dose of insulin necessary in a low dose insulin protocol for the treatment of diabetic ketoacidosis? Diabetes care.
- Goyal N, Miller JB, Sankey SS, Mossallam U (2010) Utility of initial bolus insulin in the treatment of diabetic ketoacidosis. The Journal of emergency medicine 38:422-427.
- Drenick EJ, Johnson D (1975) Evolution of diabetic ketoacidosis in gross obesity .The American Journal of Clinical Nutrition 28:264–272.
- Foster NB (1923) The treatment of diabetic coma with insulin. The American Journal of the Medical Sciences 166:699.
- Root HF (1945) The Use of Insulin and The Abuse of Glucose: In the Treatment Of Diabetic Coma. Journal of the American Medical Association 127:557-564.
- Soler N, Wright A, Fitzgerald M, Malins J (1975) Comparative study of different insulin regimens in management of diabetic ketoacidosis. The Lancet 306:1221-1224.
- Sacks HS, Shahshahani M, Kitabchi AE, Fisher JN, Young RT, et al. (1979) Similar responsiveness of diabetic ketoacidosis to low-dose insulin by intramuscular injection and albumin-free infusion. Annals of internal medicine 90:36-42.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, CrossRef
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Waseem AM, Sameena W, Shoukat RD, Baha K, Qureshi RS, et al. (2024) Insulin Bolus in Diabetic Ketoacidosis. J Diabetes Clin Prac 7: 223. DOI: 0.4172/jdce.1000242
Copyright: © 2024 Waseem AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 635
- [From(publication date): 0-2024 - Mar 26, 2025]
- Breakdown by view type
- HTML page views: 493
- PDF downloads: 142