Insecticide Treated Net, Possession, Spatial Distribution, Utilization and Associated Factors among Households of Jawi District, Northwest Ethiopia
Received: 13-Nov-2018 / Accepted Date: 05-Dec-2018 / Published Date: 07-Dec-2018 DOI: 10.4172/2161-0711.1000635
Abstract
Introduction: In malaria endemic areas, use of Insecticide Treated Nets (ITNs) for protecting mosquito bite during sleeping is highly effective. Though ITN distribution has full coverage in Jawi District, northwest Ethiopia, the malaria transmission remains high. Hence, assessing the ITN utilization and associated factors are important for further interventions.
Objective: The aim of the study was to investigate utilization of ITN and associated factors among households in Jawi-district, northwest Ethiopia.
Methods: A community based cross-sectional study was conducted among households at Jawi District from February to March, 2016. A stratified simple random sampling technique was applied. Data were collected using pretested and structured questionnaire and observation check list easy used. A total of 410 households were included in the study. A Global Positioning System (GPS) was used to gather geographical data. Bivariate and multivariate logistic regression model was fitted to identify factors associated with ITN utilization among respondents. An adjusted odds ratio with 95% confidence interval was computed to determine the level of significance.
Result: The overall utilization of ITNs among households was 201(49.0%) (95% CI: 44.16, 53.9) with full coverage and possession of 2.4 individuals per ITN. Living in urban (AOR=3.0; 95% CI: 1.5, 6.0), having good knowledge (AOR=2.1; 95% CI: 1.1-4.0), two beds (AOR=2.4; 95%CI: 1.1-5.3) and being rich (AOR=2; 95% CI: 1.1-3.7) were predictors for ITN utilization. During dry season, ITN utilization among households reduced by 89% (AOR=0.11; 95% CI: 0.06, 0.17).
Conclusion: In this study, ITN utilization and possession was below the Universal standard. The full coverage of ITN, awareness and having knowledge merely doesn’t guarantee ITN utilization. Hence, mobilizing households on sustained use of ITNs in order to optimize their role as a malaria control tool on rural and resettled villages in all seasons are supreme important.
Keywords: ITN utilization; Households; Northwest Ethiopia
Abbreviations
AOR: Adjusted Odds Ratio; BCC: Behavioral Change Communication; CI: Confidence I Interval; EPINFO: Epidemiological Information; FMOH: Federal Ministry of Health; GPS: Global Positioning System; HAD: Health Development Army; HH: Household; HLM: Health Learning Materials; IEC: Information Education Communication; ITN: Insecticide Treated Net; LLIN: Long- Lasting Insecticide Net; OR: Odds Ratio; RBM: Roll Back Malaria; SPSS: Statistical Package for Social Science; SSA: Sub-Saharan Africa; STATA: Statistics/Data Analysis; WHO: World Health Organization
Introduction
Malaria is a vector born disease [1] and poses a tremendous public health problem across the globe [2]. Malaria is endemic within most tropical and subtropical regions of the world, over 90 percent of all malaria deaths currently occur in sub-Saharan Africa (SSA) [3]. In Ethiopia, malaria transmission patterns and intensity vary greatly due to the large diversity in altitude, rainfall, and population movement [4]. Malaria is the leading cause of morbidity and mortality in endemic areas of Afar, some parts of Oromia and Amhara regions with the prevalence of more than 12.4% and 17%-23% in some specific endemic sites [5,6]. The disease causes 70,000 deaths, 17% of outpatient visits to health institutions, 15% of admissions and 29% of inpatient deaths each year [7].
Utilization of ITNs is one of the strategies of Roll Back Malaria (RBM) initiatives to reduce malaria burden in Sub Sahara Africa [8]. It is estimated to reduce malaria mortality rates by 55% in children under 5 years of age in sub-Saharan Africa [1]. Almost half of the population at risk in SSA (49%, range 44%–54%) had access to an Insecticide Treated Mosquito Net (ITN) in their household as vector control interventions [1]. But an estimated 44% (39%–48%) of the population at risk in SSA were sleeping under an ITN [1]. It is also not more than 60% in other studies of Africa [9], in Southwest Ethiopia, 58% [10] and in East Gojjam Zone, 59.1% [11].
RBM sets three new indicators; proportion of households with at least one ITN for every two people, proportion of population with access to an ITN in their household and proportion of population who slept under an ITN in the previous night [2]. ITNs used for protection against mosquito bites have proven to be a practical, highly effective, and cost-effective intervention against malaria [12] and promotion of use of ITNs has emerged as a key intervention for malaria control [13]. According to a study on many African countries consistent use of ITNs can reduce malaria transmission by up to 90% [14,15]. However, according to world malaria report 2014, only 44% of population at risk in SSA were sleeping under ITN [1].
In Nigeria and Kenya, heat and dry season [16,17] and in Ethiopia, poor condition of ITN [15] were reasons for non-utilization despite possession of ITN. In Zambia and some parts of Ethiopia, incorrectly hanging of ITN and used for other purposes had a negative impact on its utilization [15]. On the other hand perceived malaria preventive action of ITN and sustainable use of ITN [18] were significant factors for ITN utilization in Ethiopia.
In Jawi district, malaria transmission is highly endemic and the annual malaria report of the district shows that 31%-43% cases of malaria. It accounts 39%-43% admission rate [19]. These are a remarkable problem of the area and need to be put under consideration. Though ITN distribution is full coverage in the district [19], the problem remains high. Hence, assessing the ITN utilization and associated factors are very important for further interventions.
Methods
Study design and setting
A community based cross sectional study was conducted among selected households in malaria endemic district, Jawi from February to April 2016. Jawi district is located 558 km from Addis Ababa (capital of the country) in northwest Ethiopia and 157 km to southwest from Bahir Dar city.
Sample size
A single population proportion formula was used with an assumptions of 0.05 level of significance, 95% confidence interval and 0.05 margin of error, 59% estimated population proportion [11] and contingency for non-response rate of 10%. Hence, the total sample size was 410.
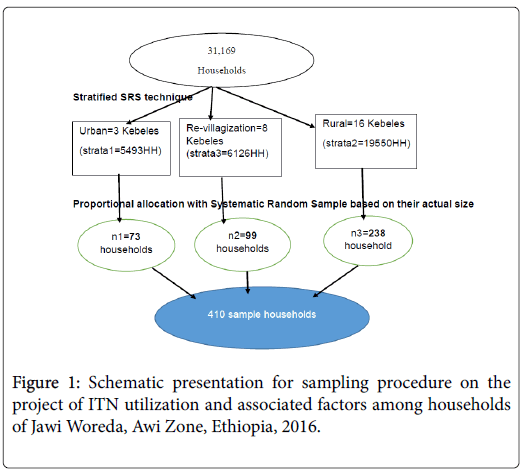
Sampling flow chart
Schematic presentation for sampling procedure on the project of ITN utilization and associated factors among households of Jawi Woreda, Awi Zone, Ethiopia, 2016 was shown as a flow chart in Figure 1.
Data collection tool and procedure
Data were collected using structured interviewer administered questionnaire, which was developed by reviewing different literatures and observation checklist about ITN utilization indicators in the night before the survey and early morning interview.
Concerning on the reliability and validity of the questionnaire a predesigned and pre-test of questionnaire were done at Pawi Woreda by taking 5% of the total sample size and necessary correction were taken after the pre-test in order to make consistency and clarity of statement and close supervision was conducted during data collection time. The reliability test of Cronbach’s alpha (ά=0.714) test were performed for the questionnaire. The collected format was checked for completeness and consistency by supervisors and PI daily and amendments were made before the next data collection. Data clean up and cross-checking was done before analysis.
Data processing and analysis
The collected data were entered and edited using Epi-Info version 3.5.3 software and then transferred to State version 12 for further analysis. After checking the correlation of independent variables, significance was determined using crude and adjusted odds ratios with 95% confidence intervals. To determine the association between the different predictor variables with the dependent variable, first bivariable analysis between each independent variable and outcome variable was investigated using a binary logistic regression model and then all variables having an association with cutoff point at pvalue< 0.2 in the bi-variable analysis were analyzed for multi-variable logistic regression.
P value<0.05 with a 95% confidence interval were regarded as significant determinant factors and the strength of the association between the variables were classified based on their value of Odds Ratio (OR). The Hosmer-Lemeshow goodness of fit test (0.841) was checked on the logistic model for appropriateness, to assess how good the model is fit (P-value>0.05).
Results
A total of 410 households (73 were urban, 238 were rural and 99 were re-villagization) were included in the study. Most, 333 (81.2%) of heads of the household were males. The median age of the participants was 37.5 with ranges 18-75, whereas the mean of family size of the households was 4.9 ± 1.9 (Table 1).
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Residence | ||
| Urban | 73 | 17.8 |
| Rural | 238 | 58.05 |
| Re-villagization | 99 | 24.15 |
| Sex | ||
| Male | 333 | 81.22 |
| Female | 77 | 18.78 |
| Marital status | ||
| Married | 312 | 7.32 |
| Single | 30 | 76.1 |
| Divorced | 40 | 9.76 |
| Widowed& In relation-ship | 28 | 6.83 |
| Educational status | ||
| An able to read and write | 223 | 54.39 |
| Read and write | 103 | 25.12 |
| Primary education (4-8) | 59 | 14.39 |
| Secondary education and above | 25 | 8.1 |
| Position in the family | ||
| House head | 372 | 90.73 |
| House wife and care giver | 38 | 9.27 |
| Occupation | ||
| Farmer | 295 | 71.95 |
| Housewife | 20 | 4.88 |
| Government employed | 10 | 2.44 |
| Private employed | 7 | 1.71 |
| Trader | 55 | 13.41 |
| Has no job and over age | 23 | 5.61 |
| Family size | ||
| ≤ 4 | 178 | 43.41 |
| >4 | 232 | 56.59 |
| Malaria risk population | ||
| Under five children | 215 | 12.5 |
| Pregnant women | 47 | 2.3 |
| 1717 | 85.2 | |
| Wealth index | ||
| Poor | 136 | 33.17 |
| 137 | 33.41 | |
| Rich | 137 | 33.41 |
Table 1: Socio demographic and economic characteristics of household heads of Jawi District, Northwest Ethiopia, 2016.
Knowledge and ITN utilization
Of the households, 328 (80%) had good knowledge about malaria. Of households, 354 (86.3%) were aware about ITN and obtained from health institution. Of these, 192 (54.27%) of them used ITN (Table 2).
| Variables | Frequency | Percentage |
|---|---|---|
| Is malaria a health problem | ||
| Yes | 373 | 90.99 |
| NO | 37 | 9.02 |
| Is malaria transmissible disease | ||
| Yes | 259 | 63.17 |
| NO | 151 | 36.83 |
| When do mosquitoes mostly bite | ||
| Day time | 17 | 4.1 |
| Night | 356 | 86.8 |
| I don’t know | 37 | 9 |
| Is malaria preventable | ||
| Yes | 385 | 93.9 |
| No | 25 | 6.1 |
| Overall knowledge | ||
| Good knowledge | 328 | 80 |
| Poor knowledge | 82 | 20 |
| Does HI give you any information on ITN? | ||
| Yes | 354 | 86.34 |
| No | 56 | 13.66 |
| Frequency of receiving the information (n=354) | ||
| Everyday | 3 | 0.85 |
| At least once a week | 41 | 11.58 |
| 1-3 times a month | 141 | 39.83 |
| In the time Longer than a month | 169 | 47.74 |
| Was ITN distributed by Health institute | ||
| Yes | 405 | 98.78 |
| No | 5 | 1.22 |
| Frequency of house visit by health workers | ||
| Once a week | 23 | 5.61 |
| Two times a month | 119 | 29.02 |
| Once a month | 156 | 38.05 |
| In the time Longer than a month | 112 | 27.32 |
Table 2: Knowledge and Health service related characteristics of household heads, Jawi District, Northwest Ethiopia, 2016.
Environmental and behavioral related characteristics of households
There were about 843 sleeping spaces (sleeping bed+sleeping mat). Of these, 504 (59.8%) were sleeping beds. Of the households which didn’t use ITN, 188 (89.9%) were not using ITNs due to dry season where they thought malaria transmission was not happening (Table 3).
| Variables | Frequency | Percentage |
|---|---|---|
| Hanged ITN over the sleeping places | ||
| Yes | 296 | 72.2 |
| No | 114 | 27.8 |
| Was there observed miss-use of ITN | ||
| Yes | 62 | 15.1 |
| No | 348 | 84.9 |
| Observed miss-use | ||
| Cover of seedlings | 20 | 32.3 |
| holding different crops | 21 | 33.9 |
| For robbing | 11 | 17.7 |
| For house equipment | 10 | 16.1 |
| Do windows and doors have screening | ||
| Yes | 92 | 22.4 |
| No | 318 | 77.6 |
Table 3: Observed behaviors of household among households of Jawi District, Northwest Ethiopia, 2016.
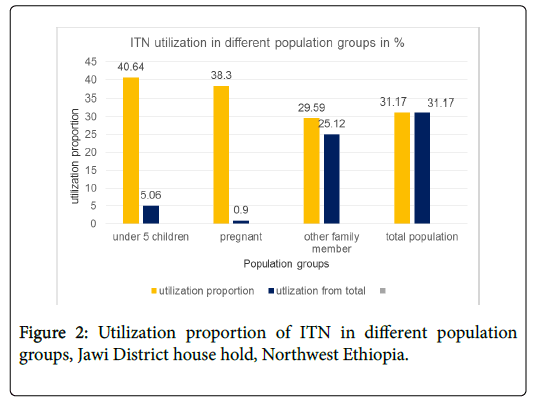
ITN Utilization proportion by residence coverage, possession and proportion
In this study, 201 (49.01%) (95% CI 44.16, 53.88) households utilized ITN. Of these, 100 (49.75%) were from rural, 51 (25.37%) were from urban and 50 (24.88%) were from re-villagization sites (Figure 2).
Associated factors for ITN utilization among households
Multi-variable logistic regression analysis; constructed by including the factors found to be significant in the bi-variable analysis showed that, were significant predictors of ITN utilization.Table 4
| Variables | ITN utilization Yes (%) | COR (95% CI) | AOR (95% CI) |
|---|---|---|---|
| Residence | |||
| Rural | 100 (42.0) | 1 | 1 |
| Urban | 51 (69.86) | 3.20 (1.82, 5.61) | 3.03 (1.52, 6.02) |
| Re-villagization | 50 (50.50) | 1.4 (0.88, 2.25) | 1.24 (0.69, 2.22) |
| Knowledge | |||
| Non-knowledgeable | 23 (28.05) | 1 | 1 |
| Knowledgeable | 178 (54.27) | 3.04 (1.79, 5.16) | 2.09 (1.09, 4) |
| Wealth index | |||
| Poor | 54 (39.71) | 1 | 1 |
| Medium | 72 (52.55) | 1.68 (1.04, 2.72) | 1.74 (0.96, 3.16) |
| Rich | 75 (54.74) | 1.84 (1.14, 2.97) | 2 (1.09, 3.69) |
| Have ITN information from HIs | |||
| Yes | 181 (51.13) | 1.88 (1.05, 3.38) | 1.48 (0.73, 3.02) |
| No | 20 (35.71) | 1 | 1 |
| Reasons affect ITN use | |||
| Not being malaria season (season) | 42 (22.46) | 0.12 (0.07, 0.18) | 0.11 (0.06, 0.17) |
| Other than season | 16 (72.7) | 1 | 1 |
| Individuals Sleep on bed being | |||
| Zero (all in mat) | 9 (34.62) | 0.82 (0.33, 2.03) | 52946 (0, -) |
| With one | 7 (36.84) | 0.9 (0.32, 2.50) | 0.47 (0.14, 1.59) |
| With two | 35 (39.33) | 1 | 1 |
| With three | 63 (50.81) | 1.59 (0.92, 2.76) | 1.07 (0.54, 2.11) |
| With four | 48 (64) | 2.74 (1.45, 5.17) | 1.56 (0.64, 3.79) |
| With five | 14 (45.16) | 1.27 (0.56, 2.90) | 0.54 (0.16, 1.85) |
| With six | 25 (54.35) | 1.83 (0.89, 3.77) | 1.37 (0.38, 4.94) |
| No. sleeping bed | |||
| Zero (no bed in HH) but only in mat | 9 (33.33) | 0.6 (0.26, 1.39) | 0.000013 (0) |
| One | 113 (45.38) | 1 | 1 |
| Two | 71 (62.28) | 1.98 (1.26, 3.13) | 2.38 (1.07, 5.32) |
| Three and above | 8 (40) | 0.84 (0.31, 2.28) | 0.69 (0.14, 3.32) |
Table 4: among households of Jawi District, Northwest Ethiopia, 2016.
Multi-variable logistic regression analysis; constructed by including the factors households who lived in urban were 3.0 times more likely to use ITN than those who lived in rural (Table 4).
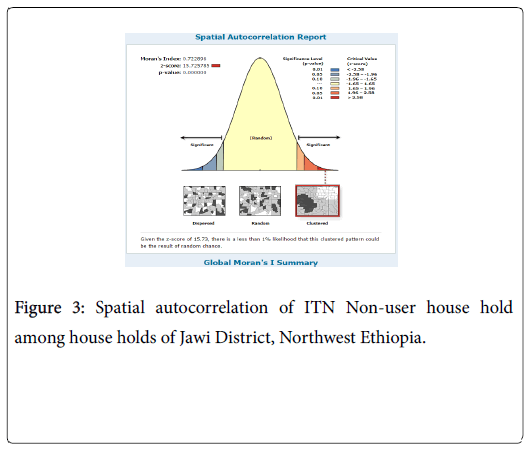
Spatial autocorrelation and distribution of ITN utilization
The spatial distribution of ITN non-user households was found to be non-random at the study period. The Global Moran’s I: 0.72 (pvalue: 0) revealed that there was statistically significant clustered pattern of households did not utilized ITN (Figure 3).
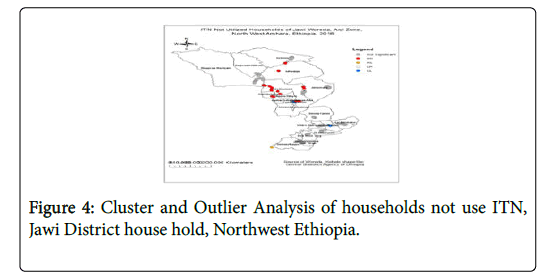
Spatial distribution for ITN non-user households
Majority of ITN non users were found in southern and middle west of the study area. As we goes to these direction especially middle west, the weather condition is too hot and households were influenced to sleep in mats rather than beds and the probability of using ITN in sleeping mat is lower as shown in the cluster analysis (Figure 4).
(HH-high value surrounded by high value (hotspot); HL-high value surrounded by low values; LH-low value surrounded by high value; and LL-low value surrounded by low value (cold spot). HL and LH are outliers. The hot spots (red colors), cold spots (blue colors), and outliers (the brown and white colors) have been identified. Others were not significant.)
Discussion
In this study, the overall household utilization of ITNs was low. There was a full ITN coverage and possession of 2.4 individuals per ITN. Dry season, too hot to sleep with ITN, ITNs causes a source of bed bug were reasons that the household did not use ITNs. Living in urban, having good knowledge about malaria prevention and transmission and being rich family are significant predictors of ITN utilization.
The result of current study revealed that, utilization of ITNs among households were low (49.01%) with a full coverage of ITNs, even though the possession is under achievement comparing to Roll Back Malaria 2013 recommendation (ITN utilization, coverage and possession to be 90%, 100% and 2 individuals per ITN respectively for effective malaria prevention by the end of 2015 [19]. The reason for this low possession may be due to that at a time of ITN distribution i.e. when one ITN per two individuals were distributed the population may not be similar with the current population [20,21].
These is also much lower than the findings, in Zambia (90%) with half coverage in 2012, in SNNP of regional state (60.6%) in 2012 [22], in Southwest Ethiopia (58%) 2013 and East Gojjam Ethiopia (59.1%) in 2014 [10]. The main reason for this variation might be season. Since the studies in Zambia and Southwest Ethiopia were conducted in pick malaria transmission seasons and studies in SNNP and East Gojjam Ethiopia were in minor malaria transmission seasons, whereas the time of current study was dry season and utilization is mostly seasonal.
But it is larger than a finding in Eastern Ethiopia (21.5%) in 2012 with 62.4% of coverage [23]. These variations might be due to the study settings. Since the study in Eastern Ethiopia was only in rural residence with altitude of 1200-2950 m. But the setting of current study was urban, rural and re-villagization with altitude of 800-1800 m above sea level.
Based on the residence, urban contributes the greatest (69.8%) proportion, re-villagization 50.5% and rural were 42% of their households. This finding is much lower than the findings in East Gojjam Ethiopia 2014 (82.2% in urban and 44.3% in rural) [11], even if urban was the dominant in both studies. Since stratification of residence were two in the previous study and three in the current study and rural might not get information and different accesses as of urbans.
Even though big variation was there, similar to world malaria report 2014 (44%)[1], studies conducted in Equatorial Guinea 2011 (49%) [23], Switzerland and Kenya 2009 (39.2% [24], Eastern Ethiopia 2012 (29.4%)[20], malaria risk groups (under five children and pregnant women) were dominant users (40.27%) among other population groups. That is why more emphasis is always for more risk groups across the world.
Like different studies conducted in Ghana, Nigeria [25] and East Gojjam Ethiopia 2014 [10], urban residence was significant predictor for ITN utilization on this study. On the other hand, similar with studies in Nigeria 2014, a two years study in Amhara and Oromia regional states [15] and findings in Eastern Ethiopia 2012 knowledge on malaria transmission and prevention, ITN use and household level malaria prevention activity was significant predictor in this study.
Among the potential predictors explored regarding utilization of ITNs in the households of Jawi District, not being a malaria season (dry season) was the one having inversely association predictor. These result is comparable with the findings in Nigeria, Kenya and Amhara and Oromia regional states of Ethiopia [26-27].
Even though ITNs were distributed freely in the households through the support of WHO and carter center, being rich family based on their wealth index was significant predictor. This might be due to housing character having bed in the house hold and this is suitable for hanging ITNs. On the other hand paying for ITN rather than receiving free in Amhara and Oromia regional states and southern Ethiopia 2011 [28] were predictors for ITN utilization.
Unlike studies in Eastern Ethiopia 2012, Southwest Ethiopia 2013 and West Gojjam; family size=<4, being farmer and being currently married were not significant predictors in current study. These might be due to that ITNs were distributed based on family size (ITN per two individuals) and marital status and occupation are not that much variability in the study.
On the other hand like studies in Serbo town, Ethiopia, sleeping space (households having two sleeping bed) was significant predictor (AOR=2.38, 95% CI; 1.07, 5.32) in this study [29,30]. Since the area is hot, and they prefer to sleep on mat rather than bed and this is not suitable for hanging and using ITNs, that is why many of them sleep on mat and sleeping on bed makes variability in the households. These might be reason that number of sleeping bed was significant predictor.
Comparable with the studies in Kenya 2011 and in SNNP of Ethiopia 2012 season, the need of saving ITNs for future, being hotness of the environment and assuming (considering) ITNs as a source of bug were challenges for not using ITNs in the study area. Also comparable proportion of miss-use of ITNs were observed as East Gojjam study in 2014 in the study.
Even though the procedure is correct with assumptions of heterogeneity the sample size was somewhat lower as compared to general population for generalization. On the other hand the study included households those registered in the family folder card and those not registered were not included. The use of nets during the high transmission season could not be assessed because it was not malaria transmission season at the time of data collection. And this study did not use the qualitative method.
Limitations
• Utilization of nets during high malaria transmission season could not be assessed because it was not malaria transmission season at the time of data collection.
• Hose holds that were not registered in the family folder card were not included in the study.
Declaration
Ethics approval and consent to participate
The ethical clearance was obtained from Institutional Review Board (IRB) of University of Gondar. A formal letters from Amhara Regional Health Bureau, Awi zone Health Department, Jawi District Administrative and Health Office were obtained. Written informed consent was obtained from the participants and were informed about the purpose, the risk and benefit of the study. Personal identifiers were not used to maintain confidentiality.
Availability of Data and Materials
The datasets generated and/or analyzed during the current study are available at University of Gondar, College of medicine and Health Science, Institute of Public Health and Amhara national regional state health bureau research and technology transfer core process in hard and soft copy repository [www.UoG.edu.et/CMHS]. In addition the data are available from the authors upon reasonable request and with permission of the principal investigators (Tiruneh Getenet).
Funding
Amhara regional Health Bureau
Authors’ Contributions
TG designed the study, participated in the data collection, performed analysis and interpretation of data and drafted the paper and revised the manuscript. KA and AN assisted with the design, approved the proposal, and revised drafts of the paper and prepared and revised the manuscript. All authors read and approved the final manuscript.
Acknowledgement
We would like to forward our heartfelt gratitude to the University of Gondar College of Medicine and Health Sciences Institute of Public Health for assigning adivisorship to do this practical research. We would like to express our thanks to Amhara Regional Health Bureau for financial support.
Finally we would like to acknowledge study participants, selected committees of HDAs, data collectors and super visors for their time and contribution of this work.
References
- Centers for Disease Control and Prevention (2014) President’s Malaria Initiative.
- FDREMOH (2008) Ethiopia national malaria indicator survey 2007: Technical Summary.
- Deressa W, Fentie G, Girma S, Reithinger R (2011) Ownership and use of insecticide-treated nets in Oromia And Amhara regional states of Ethiopia two years after a nationwide campaign. Tropical Med Int Health 16: 1552-1561.
- Adugna A (2005) Malaria in Ethiopia. Ethiopian demography and health survey, Lesson 14.
- Esimai OA, Aluko OO (2014) Determinants of use of insecticide treated bednets among caregivers of under five children in an urban local government area of Osun State, South-Western Nigeria. Global J Health sci.
- Singh M, Brown G, Rogerson SJ (2013) Ownership and use of insecticide-treated nets during pregnancy in Sub-Saharan Africa: A review. Malar J 12: 268.
- Sena LD, Deressa WA, Ali AA (2013) Predictors of long-lasting insecticide-treated bed net ownership and Utilization: Evidence from community-based cross-sectional comparative study, Southwest Ethiopia. Malar J 12: 406.
- Kassie A, Wale M, Fekensa T (2014) Assessment of insectiside treated bed net possession, proper Utilization and the prevalence of malaria in Dejen woreda, East Gojam Zone, Ethiopia. J Parasitol Vector Biolog.
- Lengeler C (2004) Insecticide-treated nets for malaria control: Real gains. Bull World Health Organ 82: 84.
- Ndwiga T, Kei RM, Dancan OW (2014) Utilization of insecticide treated bed nets among mothers attending MCH/FP in webuye district hospital bungoma county Kenya. Prevent Med 4 :470-480.
- Baume CA, Marin MC (2008) Gains in awareness, ownership and use of insecticide-treated nets in Nigeria, Senegal, Uganda and Zambia. Malar J 7: 153.
- Baume CA, Reithinger R, Woldehanna S (2009) Factors associated with use and non-use of mosquito nets owned in Oromia and Amhara regional states, Ethiopia. Malar J 8: 264.
- Idowu OA, Sam-Wobo SO, Oluwole AS, Adediran AS (2011) Awareness, possession and use of Insecticide-treated nets for prevention of malaria in children under five in Abeokuta, Nigeria J Paediatr Child Health 47: 117-121.
- Atieli HE, Zhou G, Afrane Y, Lee M-C, Mwanzo I, et al. (2011) Insecticide-treated net (ITN) Ownership, usage, and malaria transmission in the highlands of western Kenya. Parasit Vectors 4: 113.
- Amoran OE, Senbanjo IO, Asagwara CE (2011) Determinants of insecticide treated nets use among youth Corp members in Edo State, Nigeria. BMC Public Health 11: 728.
- Centers for Disease Control and Prevention (2014) State Indicator Report.
- Innovation and Networks Executive Agency (2015) Annual Activity Report Programe.
- Biadgilign S, Reda A, Kedir H (2012) Determinants of ownership and utilization of insecticide-treated bed nets formalaria control in eastern Ethiopia. J Tropic Med.
- Berie Y (2013) Insecticide treated nets utilization and associated factors among people living with HIV/AIDS in three associations in Bahir dar city administration, northwest Ethiopia.
- Batisso E, Habte T, Tesfaye G, Getachew D, Tekalegne A, et al. (2012) A stitch in time: A cross Sectional survey looking at long lasting insecticide-treated bed net ownership, utilization and Attrition in SNNPR, Ethiopia. Malar J 11: 183.
- Garcia-Basteiro AL, Schwabe C, Aragon C, Baltazar G, Rehman AM, et al. (2011) Determinants of bed net use in children under five and household bed net ownership on Bioko Island, Equatorial Guinea. Malar J 10: 179.
- Noor AM, Kirui VC, Brooker SJ, Snow RW (2009) The use of insecticide treated nets by age: Implications for universal coverage in Africa. BMC Public Health 9: 369.
- Macintyre K, Littrell M, Keating J, Hamainza B, Miller J, et al. (2012) Determinants of hanging and use of itns in the context of near universal coverage in Zambia. Health Policy Plan 27: 316-325.
- Ankomah A, Adebayo SB, Arogundade ED, Anyanti J, Nwokolo E, et al. (2012) Determinants of Insecticide-treated net ownership and utilization among pregnant women in Nigeria. BMC Public Health 12: 105.
- Amoran OE, Ariba AA, Iyaniwura CA (2012) Determinants of intermittent preventive treatment of malaria During pregnancy (iptp) utilization in a rural town in Western Nigeria. Reprod Health J 9: 12.
- Gebresilassie FE, Mariam DH (2011) Factors influencing people's willingness-to-buy insecticide-treated Bednets in Arbaminch Zuria District, southern Ethiopia. Journal of Health, Population, and Nutrition 29: 200-206.
- Siraw D (2014) Assessment of ownership and factors affecting utilization of insecticide treated bed nets in dembecha woreda, west gojjam zone, Ethiopia from September 2013 to June 2014. Addis Ababa University, Ethiopia.
- Getachew S (2005) Assessment of use of insecticide treated mosquito nets and factors affecting it in Serbo town: Addis Ababa University.
Citation: Genet T, Alemu K, Nigusie A (2018) Insecticide Treated Net, Possession, Spatial Distribution, Utilization and Associated Factors among Households of Jawi District, Northwest Ethiopia. J Community Med Health Educ 8: 635. DOI: 10.4172/2161-0711.1000635
Copyright: © 2018 Genet T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3819
- [From(publication date): 0-2018 - Apr 25, 2025]
- Breakdown by view type
- HTML page views: 2985
- PDF downloads: 834