Research Article Open Access
Inpatient Palliative Care Consultation for Women with Gynecologic Malignancies
Nicole S Nevadunsky1*, Zahava Brodt1, SerifeEti2, Peter A Selwyn3, Ann Van Arsdale1, Bruce Rapkin4 and Gary L Goldberg11Department of Obstetrics & Gynecology and Women’s Health, Division of Gynecologic Oncology, Albert Einstein Cancer Center, Albert Einstein College of Medicine, Montefiore Medical Center, NY, USA
2Department of Palliative medicine, Albert Einstein College of Medicine, Beth Israel Medical Center, New York, NY, USA
3Department of Family and Social Medicine, Department of Psychiatry and Behavioral Sciences, Department of Epidemiology & Population Health, Department of Medicine, Albert Einstein College of Medicine Department of Family and Social Medicine, Montefiore Medical Center, NY, USA
4Department of Epidemiology & Population Health, Albert Einstein College of Medicine Department of Family and Social Medicine, Montefiore Medical Center, NY, USA
- *Corresponding Author:
- Nicole S Nevadunsky
Department of Obstetrics
Gynecology and Women’s Health
Albert Einstein College of Medicine
Montefiore Medical Center
3332 Rochambeau Ave Bronx
New York 10467, USA
Tel: 718-920-4794
Fax: 718-920-6313
E-mail: nnevadun@montefiore.org
Received date: August 24, 2013; Accepted date: September 23, 2013; Published date: September 27, 2013
Citation: Nevadunsky NS, Brodt Z, SerifeEti, Selwyn PA, Arsdale AV, et al. (2013) Inpatient Palliative Care Consultation for Women with Gynecologic Malignancies. J Palliat Care Med 3:160. doi:10.4172/2165-7386.1000160
Copyright: © 2013 Nevadunsky NS et al., This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Objective: Recommendations to improve end-of-life cancer care include integration of palliative care into standard cancer care. There is limited information regarding palliative care for ethnic and racial minority women with gynecologic malignancies. The purpose of this study was to determine the impact of clinical, socio-demographic, and provider factors on palliative medicineconsultation.
Methods: After IRB approval, patients with gynecologic malignancies who received a palliative medicine consultation from January 1, 2008 until June 1, 2010 were identified. Abstracted data included demographics, reason/s for consultation, and outcomes. Results were described and comparison made using Fisher’s Exact Test, Student’s T analysis, and Kaplan-Meier time to event analysis with SPSS software.
Results: 84 patients were referred for palliative medicine consultation. Ethnic/racial distribution was Black (37%), White (39%), and Hispanic (16%). The reason/s for consultation included pain (45%), goals of care (46%), and bowel obstruction (4%), dyspnea (4%). Median number of days from the initial consultation until death by Kaplan-Meier time to event analysis, which is a proxy metric for timely consultation was 35 days [Range 0-1005 days].Younger patients (<60) were less likely to be DNR (p=0.03, 60% verses 79.5%) or referred to hospice (p=0.02, 9% versus 33%). “Goals of care” was the consultation reason in 61% of patients of medical sub-specialists vs. 26% of Gynecologic Oncologists (p=0.003). 28% of patients from medical sub-specialists died in the hospital verses 8% of gynecologic oncologist referred patients (p=0.02).
Conclusions: These data suggest that there may be barriers to the implementation of palliative medicine for women with gynecologic malignancies. Providers may be influenced by patient age as well as their own specialty background. Reasons for the barriers to access in these women need to be further explored.
Keywords
Palliative medicine; Gynecologic malignancies; Consultation models
Introduction
Recent attention has focused on innovations to improve end-of life care for patients with incurable solid tumors while addressing the exponentially increasing costs for cancer and end of life care [1]. It has been predicted that annual direct costs from cancer care will rise from the 2006 cost of $104 billion to $173 billion in 2020 [2]. Integration of palliative care into routine oncology care is one suggested change in attitudes and practices for health care providers managing patients with cancer [3]. In 2012 the American Society of Clinical Oncology put forth a consensus statement that suggested that “combined standard oncology care and palliative care should be considered early in the course of illness for any patient with metastatic cancer and/or high symptom burden” [4]. The consensus opinion cited seven randomized controlled trials (RCT) demonstrating improvement in symptoms, quality-of-life, patient satisfaction, reduced caregiver burden, more appropriate referral and use of hospice, reduced use of futile intensive care and other invasive care and improved survival [5-11]. Additionally there are retrospective reports that timely consultation by palliative medicine experts results in decreased metrics associated with poor end-of-life care, as well as decreased cost [12,13].
Concerns of changing attitudes and practices are real as we do not know how patients, physicians or payers may be affected by these changes. Additionally, negative attitudes and misunderstanding of the role and place of palliative medicine have arisen secondary to references to “death panels” during debate regarding health care legislation. Despite these concerns, no studies to date have described patient/caregiver harm or excessive cost from early palliative care involvement and management [4]. While the evidence from RCTs integrating standard oncology practice and palliative care are promising, the applicability of these trials to general oncology practice is yet to be tested, reproduced or proven. Additionally, the optimal method of integration of palliative medicine into standard oncology care is unknown, and at the present time, less than 1% of National Institute of Health funding is directed at research in palliative medicine [12].
In reviewing the end-of-life care in the last decade in the United States, a significant number of cancer patients who died from cancer received new chemotherapy regimens, had multiple emergency department visits, and hospitalizations including intensive care admissions at the end-of-life [14,15]. Conversely, hospice care and palliative medicine services were under-utilized, with less than 28% of patients under hospice care at the time of death [14]. An obstacle to the implementation of concurrent care is that little is known regarding clinical care guidelines for consultation with palliative medicine for women with gynecologic malignancies. The Society of Gynecologic Oncology (SGO), the parent organization for Gynecologic Oncologists in the US, has recently organized a Palliative Medicine Network to provide resources and educational programs to SGO members in recognition of this void. However, much remains to be learned regarding the optimal treatment planning and protocols of care for these cancer patients at the end-of-life.
In studies limited to gynecologic malignancies, enrollment in hospice is associated with decreased resource utilization without appreciable change in survival. Despite these reports resonating themes include that approximately 30% of patient die while awaiting initiation of hospice care at home or in an inpatient unit, patients receive aggressive interventions up to the time of death and that resource utilization for non-hospice patients is much greater without an appreciable improvement in outcomes. Keyser et al. described 81 patients, of which 52 were enrolled in hospice and found significantly greater incidence of invasive procedures performed within 4 weeks of death including chemotherapy (55% versus 33%) for women not enrolled in hospice compared to women enrolled in hospice [16]. Lewin et al. found a cost difference of $15,164 for women enrolled in hospice versus $59,319 for women with gynecologic malignancies not enrolled in hospice [17]. Despite this report Fauci et al. reported utilization of palliative care/hospice at the end of life for women with gynecologic malignancies, and found that median time between hospice enrollment and death was short, 22 days [18]. In an evaluation of trends for hospice use from 1992-1997, Dalrymple et al. described that while clinicians were placing DNR orders earlier, outcomes remained unchanged and that 30% of patients died while awaiting discharge to home with hospice or transfer to inpatient hospice care [19]. There is also evidence that discussion of comfort care and in the outpatient setting is associated with fewer hospitalizations and days of hospitalization [20,21]. Most studies of end of life care in gynecologic malignancies have focused on hospice referral or poorly defined discussions of comfort care by the primary treating gynecologic oncologist. To date no studies have described the characteristics of formal palliative medicine consultation for women with gynecologic malignancies.
Montefiore Medical Center is the largest hospital center in the Bronx, which has about 1.4 million persons, and is the poorest urban county in the United States. It is a 1,062 bed, urban community academic medical center. Over 27% of Bronx residents have incomes below the poverty level and 32% of the Bronx population is foreign born. Montefiore Medical Center provides medical care to a highly diverse population: 48% of its patients are identified as Latino/Hispanic, 31% as African American. English is the second language for more than half of all the inhabitants of the Bronx. Providing culturally sensitive end of life care is an important health care issue in these urban underserved communities such as the Bronx where the prevalence rates for many poverty related illnesses such as late stage presentation with cancer, or HIV is above the national average.
The Palliative Care Service (PCS) was established in 2000 and currently provides care to nearly 40% of the adult patients who die at Montefiore Medical Center each year. This compares with the national norm of 13% [14]. On average there were 800 new in-patient consultations during the study period, more than 600 in-patient unit admissions and 2000 outpatient clinic visits to the palliative care service each year. Palliative medicine at Montefiore Medical Center has developed an integrated model of care with Critical Care Medicine and Emergency Medicine [1,22-24]. The primary role of the PCS is consultative services and is available upon request by the patients attending of record. Patients with gynecologic malignancies were admitted by primary gynecologic oncologists or medical subspecialists including internists, medical oncologists, general surgeons, neurologists, neurosurgeons, and critical care specialists. At the time of data collection the PCS consisted of three palliative care physicians, two specialist nurse practitioners, two social workers and a pastoral care worker. To date there has been no standardized assessment of the palliative care and hospice needs of women with any type of cancer in the Bronx. This study is designed to describe the utilization of palliative medicine services in patients with advanced gynecologic malignancies at our institution. In particular, we were interested in referral characteristics as related to patient demographics and problems as well as characteristics of referring physicians.
Methods
After IRB approval, all patients with gynecologic malignancies who were referred for a palliative medicine consultation from January 1, 2008 until June 1, 2010 were identified from a comprehensive clinical database of all patients at Montefiore Medical Center who were referred to inpatient palliative medicine consultation. This database consisted of archived consultation requests from referring physicians as well as history, physical, assessment and plan from consultants’ first interaction with patients. Each archived consultation request was evaluated for site of disease, which was verified by review of pathology, radiography, and patient encounter records available in the electronic medical record. Only patients with confirmed gynecologic malignancies (uterine, cervical, ovarian, primary peritoneal, vulvar or vaginal) were included. Consultation reason was abstracted from record of referring teams request. Consultation charts were reviewed and the pathology was verified utilizing central pathology documentation. Abstracted data included patient demographics, disease status, reason/s for the palliative care consultation, clinical status and findings, interventions and outcomes. Symptom burden was abstracted from consultation narrative including assessment and plan. Data regarding the patient’s date of death was abstracted from the electronic medical record as well as the on-line social security database records. Results were described and comparisons between the groups were made using Fisher’s Exact, Student’s T analysis and Kaplan-Meier time to event anlaysis with SPSS software.
Results
At the time of this analysis, 75 of the 84 patients (89%) had died. The mean age of patients was 64 years (range 22-96 years) (Table 1). Primary cancer sites were: uterus 37 (44%), ovary/fallopian tube 26 (31%), cervix 15 (18%), and vulva/vagina 6 (7%). All patients had metastatic, recurrent, or progressive disease at time of consultation request and stage distribution at time of initial staging was 22% Stage I, 16% Stage II, 30% Stage 3, and 32% Stage IV Self-described ethnic/ racial distribution was, Black 31 (37%), White 33 (39%), Hispanic 13 (16%) and ”Other” 7 (8%). Relationship status was 23 (27%) married, 37 (36%) single, 16 widowed (19%), divorced 13 (16%) and unknown 2 (2.4%). Patients had an average of 1.8 (range 0-7) major medical problems, including diabetes, hypertension, and coronary artery disease. Fourteen (17%) of patients had a diagnosis of a mental health disorder including depression, anxiety, dementia and schizophrenia.
| Characteristics | N=84 (%) |
|---|---|
| Age | |
| Mean | 63 |
| Range | (22-96) |
| Race/Ethnicity | |
| Black | 31 (36.9) |
| Hispanic | 13 (15.5) |
| White | 33 (39.3) |
| Other | 7 (8.3) |
| Disease Site | |
| Uterus | 37 (44.0) |
| Ovary | 24 (28.6) |
| Cervix | 15 (17.9) |
| Vulva | 5 (6.0) |
| Other | 3 (3.5) |
| Psychiatric Co-Morbidities | 14 (16.7) |
| Medical Co-Morbidities | |
| Mean | 1.8 |
| Range | 0-7 |
| Patient Delirious | 6 (7.1) |
Table 1: Patient demographics
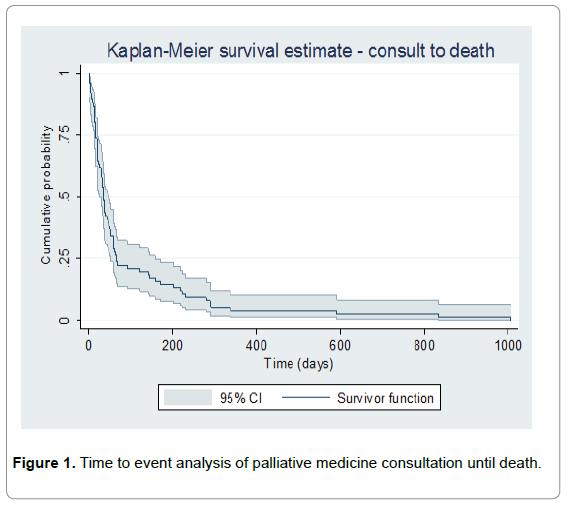
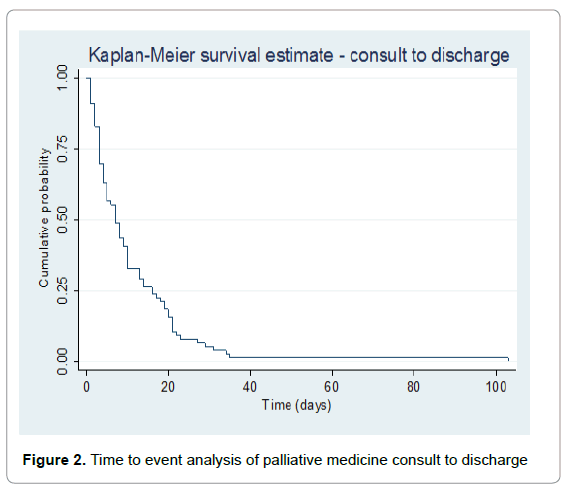
The primary reasons for the palliative care consultation included pain (45%), bowel obstruction (4%), dyspnea (4%), and nausea/ vomiting (1%) (Table 2). In 46% of the consultations, the palliative care team were asked to address the overall “goals of care”, which includes establishment of a health care proxy, do-not-resuscitate/dono- intubate orders (DNR/DNI), hospice enrollment, and discussion regarding avoidance of non-meaningful and /or futile invasive interventions. Median number of days from the initial consultation until deathby Kaplan-Meier time to event analysis, which is a proxy metric for timely consultation was 35 days [Range 0-1005 days, 95% CI of medians, 25-49 days] (Figure 1). Median time from consult to discharge was 7 days [Range 0-103 days] (Figure 2).
| Days Consult Until Death | |
|---|---|
| Median | 31 |
| Range | 0-591 |
| Reason for Consultation | |
| Pain | 38 (45.2) |
| Goals of Care | 39 (46.4) |
| Bowel Obstruction | 3 (3.6) |
| Dyspnea | 3 (3.6) |
| Nausea/Vomiting | 2 (1.2) |
| Patients on opioids at time of consult | 67 (79.7) |
| Pain well controlled | 46 (54.7) |
| Pharmacologic intervention advised | 68 (80.9) |
| Hospice resident at time of consult | 5 (5.9) |
| Hospice referral at time of consult | 19 (22.6) |
| DNR/DNI before admission | 22 (26.2) |
| DNR/DNI after admission | 60 (71.4) |
Table 2: Characteristics of Consultation
Hospice referral was made on the first day of consultation for 19 (23%) patients and five patients (6%) were current hospice residents that had been admitted to the hospital. Twenty-two patients (26%) had DNR/DNI consent at the time of admission. During the index hospitalization 60 (71%) of patients were transitioned to DNR/DNI code status. Palliative care consultants recommended medication changes, including addition, removal, change of dose, for 68 (81%) of patients. Pain was reported as uncontrolled by 46 (55%) of the patients, although 67 (80%) of the patients were using opioid narcotics at the time of the initial consultation. Five patients (6%) were noted to be delirious by consultants at the time of the initial consult interview. There was no difference in the consultation rate between older and younger patients (<60 years). However, younger patients were less likely to be DNR (p=0.03, 60% versus 80%) and referred to hospice (p=0.02, 9% versus 33%).
There were differences in consultation reasons and dispositions depending on who referred the patient: gynecologic oncologists or medical sub-specialists (Table 3). Thirty-eight (45%) patients were referred by medical sub-specialists and forty-six (55%) were referred by gynecologic oncologists. “Goals of care” was identified as the initial reason or indication for consultation in 61% of patients from medical sub-specialists (medical oncology and other) vs. 26% from gynecologic oncologists (p=0.003). Twenty-eight percent of the palliative care patients referred from medical sub-specialists died in hospital in compared to 8% of patients of referred by gynecologic oncologists (p=0.02).
| Gynecologic Oncologists n=38 (%) | Medical Subspecialists n=46 (%) | P | |
|---|---|---|---|
| Consult Reason | 0.001 | ||
| Pain | 27 (71.1) | 12 (26.1) | |
| Goals of care | 10 (26.3) | 28 (60.9) | |
| Nausea/Vomiting | 0 (0) | 1 (2.2) | |
| Dyspnea | 1 (2.6) | 2 (4.3) | |
| Bowel Obstruction | 0 (0) | 3 (6.5) | |
| On opioid | 34 (89.4) | 33 (71.7) | |
| Pain controlled | 16 (42.1) | 22 (47.8) | |
| Pharmacologic intervention | 34 (89.4) | 34 (73.9) | |
| DNR/DNI | 26 (68.4) | 34 (73.9) | |
| Referred to hospice | 8 (2.1) | 11 (2.4) | |
| Died in hospital | 3 (7.9) | 13 (28.3) | 0.02 |
Table 3: Comparison of Consultations between Gynecologic Oncologists and Medical Subspecialists
Discussion
In this study we have described the current practice of palliative medicine consultation at our institution and for our ethnically/racially diverse patient population. While organizations such as ASCO issue recommendations for earlier initiation and integration of palliative medicine with standard oncology care, there is a paucity of data on which to base guidelines for these referrals. Of note, time from consultation until death in our patient population was about 31 days (0-591). If we consider that hospice care in the United States is available to patients for the last six months of life, thirty one days between consultation and death appears to be an inadequate length of time for patients to be provided the benefit of palliative medicine resources. From the perspective of the ASCO recommendation for concurrent care at time of diagnosis of metastatic cancer and/or high symptom burden, patients may have benefitted for a period of time even longer than 6 months. Additionally, the median of 31 days is shorter than 1.4 months (interquartile range 0.5-4.2 months) between time of consultation to death reported by Hui et al. in a study of access to palliative care at MD Anderson Cancer Center [25]. Several studies recommend early palliative care consultation improves quality of life, including Temel et al. who defined early palliative medicine intervention as being within eight weeks of the diagnosis of metastatic non-small cell lung cancer [11].
Palliative care consultants often made recommendations for pharmacologic intervention and identified deficiencies in pain and symptom control. Several studies have addressed deficiencies in the basic healthcare professional training and utilization of pain and symptom management as an integral part of end-of-life care. These differences are even more pronounced in low socio-economic, ethnic minority patients with cancer [26]. For a variety of reasons, the symptom burden is often under-recognized or unrecognized and often under or -untreated. In a study of physicians and nurses perceptions, 75% of providers underestimated the incidence of delayed nausea and vomiting in patients receiving emetogenic chemotherapies [27]. Similarly, in a study of approximately 60,000 patients with breast, colorectal, lung or prostate cancer, long –acting opiate prescription was made in only 10% of these patients, despite data that up to 75% of the cancer patients experience significant pain at the end-of-life [28]. In our study group only 4% had consultation specifically for bowel obstruction. Possible explanations for this low rate of complaint prompting referral include overlap with patients referred for pain and goals of care, manifestation pattern of advanced cancer in our disease population (44% uterine), and comfort level of the primary team in managing bowel obstruction independent of consultation service.
There is no adequate explanation for the decreased number of DNR/ DNI code status and hospice referrals for patients under the age of 60. It is possible that consultants felt less comfortable in prognosticating survival for these younger cancer patients. Alternatively, these younger cancer patients may have refused DNR/DNI code status. It is of interest that gynecologic oncologists were more likely to request assistance with pain control, and medical sub-specialists were more inclined to ask for assistance in establishing goals of care. This finding may reflect the longer standing relationships that gynecologic oncologists have with their patients and their perception that they do not need assistance in establishing goals of care. Alternatively, the need for gynecologic oncologists to request assistance with pain control may reflect deficiencies in their training and knowledge base regarding utilization of pain medications. It is also unclear why there were fewer hospital deaths for patients referred by gynecologic oncologists than the medical sub-specialists.
Our study presented data on a racially/ethnically diverse population, with approximately 61%, self-identified as non-white. It was beyond the scope of this study to identify specific barriers to palliative medicine consultation associated with race. Within this population there were no differences in time from consultation until death associated with race, pharmacologic interventions, DNR/DNI, or referral to hospice. In comparison to Fauci et al. (77% identified as Caucasian), there was a higher prevalence of late stage disease, 32% versus 18% Stage IV, and uterine cancer (44% versus 19%) in our study population [18]. The majority of data regarding palliative care for women with gynecologic malignancies has to this point in time focused on ovarian cancer and there may be different symptom burdens associated with aggressive uterine disease, which is associated with non-white race. Additionally, it is unclear whether race is associated with later stage at palliative medicine intervention and this may warrant further study related to resource availability and patient preferences.
Limitations of our study include the retrospective data abstraction from chart review. In addition, our study population was taken from a single institution. These data were exploratory in nature and limited by small sample size, lack of symptom assessments and lack of outcomes data. Outpatient consultation utilization was also beyond the scope of this study and may have influenced rates of hospital death. Findings of this study may not be applicable to other institutions or populations, as our palliative medicine service has been operating a high volume consultation service for a decade. The training of all health care providers in palliative medicine and end of life care needs to be assessed and addressed to impact this important patient care and quality of life issue.
There is a significant need for the prospective assessment of the outcomes of interventions recommended by palliative care consultants as well as the effects on the patient and the family especially regarding general satisfaction and quality-of-life assessments after palliative medicine consultation.
References
- Smith TJ, Hillner BE (2011) Bending the cost curve in cancer care. N Engl J Med 364: 2060-2065.
- Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML (2011) Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst 103: 117-128.
- Brody H (2010) Medicine's ethical responsibility for health care reform--the Top Five list. N Engl J Med 362: 283-285.
- Smith TJ, Temin S, Alesi ER, Abernethy AP, Balboni TA, et al. (2012) American Society of Clinical Oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol 30: 880-887.
- Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, et al. (2009) Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 302: 741-749.
- Brumley R, Enguidanos S, Jamison P, Seitz R, Morgenstern N, et al. (2007) Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc 55: 993-1000.
- Gade, G, Venohr, I, conner, D, McGrady K, Beane J, et al. (2008) Impact of an inpatient palliative care team: A Randomized trial of in-home palliative care. J Palliat Med 11: 180-190.
- Meyers FJ, Carducci M, Loscalzo MJ, Linder J, Greasby T, et al. (2011) Effects of a problem-solving intervention (COPE) on quality of life for patients with advanced cancer on clinical trials and their caregivers: simultaneous care educational intervention (SCEI): linking palliation and clinical trials. J Palliat Med 14: 465-473.
- Pantilat SZ, O'Riordan DL, Dibble SL, Landefeld CS (2010) Hospital-based palliative medicine consultation: a randomized controlled trial. Arch Intern Med 170: 2038-2040.
- Rabow MW, Dibble SL, Pantilat SZ, McPhee SJ (2004) The comprehensive care team: a controlled trial of outpatient palliative medicine consultation. Arch Intern Med 164: 83-91.
- Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, et al. (2010) Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363: 733-742.
- Morrison RS, Dietrich J, Ladwig S, Quill T, Sacco J, et al. (2011) Palliative care consultation teams cut hospital costs for medicaid beneficiaries. Health Aff 30: 454-463.
- Gonsalves WI, Tashi T, Krishnamurthy J, Davies T, Ortman S, et al. (2011) Effect of palliative care services on the aggressiveness of end-of-life care in the Veteran's Affairs cancer population. J Palliat Med 14: 1231-1235.
- Earle CC, Neville BA, Landrum MB, Ayanian JZ, Block SD, et al. (2004) Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol 22: 315-321.
- Lunney JR, Foley KM, Smith TJ, Gelband H (2003) Describing Death in America: What We Need to Know. National Academy of Press, Washington, DC.
- Keyser EA, Reed BG, Lowery WJ, Sundborg MJ, Winter WE 3rd, et al. (2010) Hospice enrollment for terminally ill patients with gynecologic malignancies: impact on outcomes and interventions. Gynecol Oncol 118: 274-277.
- Lewin SN, Buttin BM, Powell MA, Gibb RK, Rader JS, et al. (2005) Resource utilization for ovarian cancer patients at the end of life: how much is too much? Gynecol Oncol 99: 261-266.
- Fauci J, Schneider K, Walters C, Boone J, Whitworth J, et al. (2012) The utilization of palliative care in gynecologic oncology patients near the end of life. Gynecol Oncol 127: 175-179.
- Dalrymple JL, Levenback C, Wolf JK, Bodurka DC, Garcia M, et al. (2002) Trends among gynecologic oncology inpatient deaths: is end-of-life care improving? Gynecol Oncol 85: 356-361.
- Acevedo M, Havrilesky L, Abernethy A, Kamal A, Broadwater G, et al. (2013) Addressing comfort-care int eh ambulatory setting is associated with improved end0of-life quality measures among women with ovarian cancer. Gynecoloncol 130: 152-155.
- Doll KM, Stine JE, Van Le L, Moore DT, Bae-Jump V, et al. (2013) Outpatient end of life discussions shorten hospital admissions in gynecologic oncology patients. Gynecol Oncol 130: 152-155.
- Twaddle ML, Maxwell TL, Cassel JB, Liao S, Coyne PJ, et al. (2007) Palliative care benchmarks from academic medical centers. J Palliat Med 10: 86-98.
- O'Mahony S, McHugh M, Zallman L, Selwyn P (2003) Ventilator withdrawal: procedures and outcomes. Report of a collaboration between a critical care division and a palliative care service. J Pain Symptom Manage 26: 954-961.
- Mahony SO, Blank A, Simpson J, Persaud J, Huvane B, et al. (2008) Preliminary report of a palliative care and case management project in an emergency department for chronically ill elderly patients. J Urban Health 85: 443-451.
- Hui D, Kim SH, Kwon JH, Tanco KC, Zhang T, et al. (2012) Access to palliative care among patients treated at a comprehensive cancer center. Oncologist 17: 1574-1580.
- Welch LC, Teno JM, Mor V (2005) End-of-life care in black and white: race matters for medical care of dying patients and their families. J Am Geriatr Soc 53: 1145-1153.
- Herrstedt J (2002) Nausea and emesis: still an unsolved problem in cancer patients? Support Care Cancer 10: 85-87.
- Setoguchi S, Earle CC, Glynn R, Stedman M, Polinski JM, et al. (2008) Comparison of prospective and retrospective indicators of the quality of end-of-life cancer care. J Clin Oncol 26: 5671-5678.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 14187
- [From(publication date):
October-2013 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 9654
- PDF downloads : 4533