Innovative Dental Implant Technologies
Received: 30-Jun-2022 / Manuscript No. johh-22-70220 / Editor assigned: 02-Jul-2022 / PreQC No. johh-22-70220(PQ) / Reviewed: 16-Jul-2022 / QC No. johh-22-70220 / Revised: 21-Jul-2022 / Manuscript No. johh-22-70220(R) / Accepted Date: 25-Jul-2022 / Published Date: 28-Jul-2022 DOI: 10.4172/2332-0702.1000326
Abstract
A frequent remedy for tooth loss is dental implants. This study provides an overview of the state-of-the-art regarding implant surfaces, instantaneous versus conventional loading, short implants, sinus lifts, and three-dimensional printed custom implants. The majority of implant surface alterations had successful Osseo integration outcomes. Positive outcomes were seen in animal trials involving the recently created and analysed bimolecular coatings. Because immediate loading has the benefit of shortening treatment periods and delivering function and aesthetics sooner than conventional loading, it can be employed as a successful treatment. Comparing short implants to conventional implants, similar clinical results were obtained. It is possible to use a range of sinus augmentation methods, grafting materials, and alternative methods such tilted implants, zygotic implants, and short implants. Customized implants can be utilised as an alternative to conventional implant designs thanks to the development of new technologies in three dimensions and computer-aided design/computer-aided manufacture (CAD/CAM). However, there are restrictions because there aren’t any clinical or long-term trials. A more predictive analysis and a lengthy clinical trial are required.
Keywords: Dental implants; Sinus floor augmentation; Immediate dental implant loading; Osseo integration; Computer-aided design
Keywords
Dental implants; Sinus floor augmentation; Immediate dental implant loading; Osseo integration; Computer-aided design
Introduction
Periodontitis is the most frequent reason for tooth loss; but additional reasons include dental caries; trauma; birth defects; and hereditary conditions [1]. In the past 30 years; there has been an upsurge in the use of dental implants to replace missing teeth [2]. Prior to dental implants; dentures and bridges were utilised; but because of the procedure’s high success rate; predictability; and relative lack of problems; dental implants have become a very popular alternative [1- 3].
There have been several researches published and on-going about dental implants. The present state of dental implant research is summarised in each section of this study (implant surface; immediate loading versus conventional loading; short implant; sinus lifting; and custom implant using three-dimensional printing) [4].
A dental surgeon places artificial components called dental implants into a patient’s jawbone. If one or more teeth have been lost; a person may require an implant.
What exactly are dental implants?
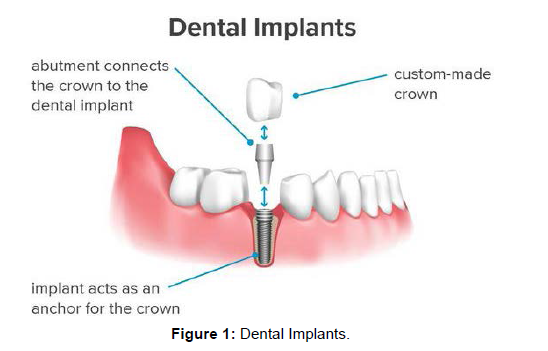
(Figure 1) A dental implant is a structure that acts as a tooth replacement. The surgeon places an implant into the jawbone using tools that resemble screws; the implant serves as the anchor for a crown; which is a type of artificial tooth [5].
The dental implant and the prosthetic tooth are joined by a component known as an abutment.
The crown is designed specifically for the individual to fit their mouth and complement their tooth colour. Crowns have a natural appearance; feel; and performance [6].
Compared to detachable artificial teeth known as dentures; implants have a number of benefits. Implants:
• Are more comfortable and natural-looking;
• Have a higher success rate;
• enhance chewing ability;
• Lower the risk of cavities forming in teeth nearby;
• Better preserve the bone at the site of the lost tooth;
• Lessen the sensitivity of teeth nearby;
• Don’t need to be taken out and cleaned every night.
Dental implants; however; are not appropriate for everyone. Before having implant surgery; a person’s bones must be in good shape since the implanting devices need to form a bond with the jawbone [7].
Types
Endosteal and sub periosteal dental implants are the two types available.
The most typical kind of implants is Endosteal. Each one can accommodate one or more false teeth and is implanted into the jawbone by a surgeon [8].
A sub periosteal implant is attached to the jawbone by a surgeon.
For patients with low jawbone height; dental surgeons recommend this method.
Stability
Around 3 million Americans have dental implants; and this number rises by roughly 500000 per year; according to the American Academy of Implant Dentistry [9].
When a trained and experienced surgeon or dentist completes the procedure; dental implant surgery is safe. Additionally; it is the only method of dental restoration that promotes the growth and preservation of the jawbone.
Threats
There are some persons who cannot receive dental implants. Dental surgeons should avoid performing procedures on patients who have:
• Acute illness
• Metabolic disorder that is uncontrollable
• Infection or sickness of the bones or soft tissues
A person can get the operation if these problems are fixed. Dentists may decline to treat patients who have any of the following conditions:
• Heavy cigarette smoking;
• Para functional behaviours like clenching or grinding teeth;
• Behavioural or mental health issues;
• HIV;
• Diabetes;
• Osteoporosis;
• AIDS are just a few examples.
There is an increased risk of the implant failing in those who have any of the aforementioned conditions and undergo dental implant surgery [10]. Due to an increased risk of implant issues; dental surgeons may also elect to avoid performing procedures on patients receiving the following treatments:
• Radiation therapy for the head or neck;
• Chemotherapy;
• Bisphosphonate medication treatment for bone loss illnesses;
Risks associated with implant surgery
Complication during or after this treatment could occur in patients [11]. The issues may include:
• A surgical incision opening following surgery;
• Implant movement;
• Implant exposure above the gum line;
• Nerve injury causing altered sensation in the surgical area;
• An implant infection
In order to enhance the condition of the bone and gums; remove or replace the implant; or both; those who experience movement or exposure of the implant may need to undergo further treatments [12].
Some warning signs and symptoms indicating an implant placement was failed include:
• Fast; progressive bone loss;
• Excessive implant mobility;
• Discharge of pus or other fluids from the location;
• Pain when tapping the implant
Methods
Each patient’s experience with dental implant surgery is likely to be unique [12]. The following variables could have an impact on this:
• The quantity and quality of bone at the implant site;
• The number of teeth that need to be replaced;
• The position of the implants inside the jaw;
• The underlying oral and general health of the patient.
These variables may warrant the need for extra procedures. These may consist of:
Sinus augmentation/ Sinus lifting
Intensification or elevation of the sinuses: Due to the location of the sinuses; implant placement in the upper jawbone is typically challenging. A sinus augmentation technique; in which the sinuses’ floors are raised to encourage the growth of additional bone; may be required by the surgeon in order to ensure the success of the implantation [13].
Sinus augmentation technique: The term “sinus augmentation;” sometimes known as “sinus lifting;” was first used to refer to a surgical procedure that involved making a bone window in the vestibular wall of the sinus. Next; a gap was made for bone grafting by gently raising the sinus epithelium. In the vicinity of the iliac crest; bone was harvested and then positioned in the ready location [14]. Prior to implantation; the healing process lasted roughly 6 months. It was suggested that bone grafting during sinus augmentation use autogenous bone; allograft; and alloplast material. There was also a demonstration of the one-stage technique; which combines sinus augmentation and implantation in a single procedure as opposed to the two-stage approach; which delayed the implantation for a number of months [15]. Due to its consistent efficacy; the aforementioned technique-also known as sinus lifting with the lateral window—is still frequently employed in contemporary implant dentistry.
One-stage osteotome sinus floor elevation was a less intrusive method. This method used a crestal approach to gain access to the sinus epithelium. With increasing diameter; the osteotomes’ tips elevate the sinus epithelium by pushing a mass of bone above the initial sinus floor to the necessary elevation [16]. After performing sinus enlargement and any necessary bone grafting; the implants were then put in place without needing to be drilled. However; it was asserted that main stability required a minimum of 6-mm alveolar bone height.
Perforation of the sinus epithelium was one of the most frequent side effects of sinus augmentation. This condition could be brought on by sinusitis; severe bleeding; or a slow rate of recovery [17]. In order to prevent complications from sinus augmentation; numerous modified surgical methods and tools were developed. To lessen the possibility of rupturing the sinus membrane; a crystal approach utilising a nontraumatic drill was recommended. Long implants (13 mm and 15 mm) were placed in 265 instances during a retrospective analysis. There were numerous options for bone grafting.
Either a bone replacement or bone from the osteotomy site might be used to replace the missing bone. Implants may be placed by skilled surgeons without the need for grafting; and the tips of the implants could support the sinus membrane. Similar to the crystal approach technique; primary stability is attained if there is at least 3 mm of accessible alveolar bone height [18].
Additionally; using absorbable collagen membranes in perforated sinuses for sinus elevation and implant implantation yielded positive outcomes. In another method; implants were first inserted in the ulna to treat the posterior edentulous maxilla. A sinus region with a 3 to 4 mm protrusion was transplanted with bone blocks containing implants after 6 weeks. After that; the implants were given six weeks to recover [19]. Patients who received particulate bone grafts (an autogenous bone graft from the symphysis; tibia; or iliac crest) served as controls to compare the effectiveness of this therapy technique. In the control group; grafts had been allowed to heal for six months before being implanted. Regarding implant stability; there were no differences between the two groups. At 6 and 12 months; there was a considerable improvement in implant stability in both groups. In extreme cases of bone atrophy; an ulna implant block in conjunction with sinus grafting may be an efficient way to increase the vertical bone height [20].
Ridge transformation
Some people’s jawbone abnormalities hinder the development of enough bone for an implant. A ridge alteration may be required in such circumstances by the surgeon.
In order to see the area of the malformed bone; you must lift the gum. The surgeon will next rebuild the damaged area using bone or a bone substitute. In order to prepare for dental implant surgery; this enhances the jawbone’s quality [21, 22].
Restoration
Following dental implant surgery; a patient must continue to maintain good oral hygiene habits; including regular brushing and flossing. The same maintenance is needed for artificial teeth as for natural teeth.
To check on the implants and make sure the teeth and gums are in good condition; the surgeon or dentist will also arrange follow-up appointments [23]. For thorough cleanings every six months; it’s vital to visit the dentist again.
Expense
The following elements may affect the price of dental implant surgery:
• Whether further treatments are required to prepare the mouth for surgery;
• The quantity and types of implants that are required;
• Where the implants are located within the jaw.
The price of dental implant surgery can be estimated by a dentist or other oral health expert during a preliminary exam [24].
Some dental insurance plans offer greater expense coverage. Bridges are one alternative to dentures that may be less expensive. Bridges; on the other hand; are more difficult to keep clean and frequently need replacement and repair; which raises the overall cost. If dental implants are taken care of properly; they might have longer-term advantages [25, 26].
Discussion
Dental implants serve as bone-anchored fixtures to replace lost teeth. Long-term advantages can be obtained through implants; which have a high success rate.
To prepare their mouth for dental implants; some people require extra operations. These will raise the overall price. Costs may also increase depending on the type and quantity of implants needed. Asking their dentist if dental implant surgery is right for them is advised for anybody considering it.
Conclusion
Recent advancements in implant success rates include sinus lifts; rapid loading; short implants; surface changes; and bespoke implants. The absence of long-term or clinical trials has; however; resulted in restrictions. We require a more predictive analysis and a lengthy clinical trial.
Acknowledgement
None
Conflict of Interest
None
References
- Jenny G, Jauernik J, Bierbaum S, Bigler M, Gratz KW, et al. (2016) A systematic review and meta-analysis on the influence of biological implant surface coatings on periimplant bone formation. J Biomed Mater Res A 104: 2898–2910.
- Smeets R, Stadlinger B, Schwarz F, Beck-Broichsitter B, Jung O, et al. (2016) Impact of dental implant surface modifications on osseointegration. Biomed Res Int 2016: 6285620
- Von Wilmowsky C, Moest T, Nkenke E, Stelzle F, Schlegel KA (2014) Implants in bone: part I. A current overview about tissue response, surface modifications and future perspectives. Oral Maxillofac Surg 18: 243–257.
- Li LH, Kong YM, Kim HW, Kim YW, Kim HE, et al. (2004) Improved biological performance of Ti implants due to surface modification by micro-arc oxidation. Biomaterials 25: 2867–2875.
- Buser D, Janner SF, Wittneben JG, Bragger U, Ramseier CA, et al. (2012) 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res 14: 839–851.
- Degidi M, Nardi D, Piattelli A (2012) 10-year follow-up of immediately loaded implants with TiUnite porous anodized surface. Clin Implant Dent Relat Res 14: 828–838.
- Binahmed A, Stoykewych A, Hussain A, Love B, Pruthi V (2007) Long-term follow-up of hydroxyapatite-coated dental implants-a clinical trial. Int J Oral Maxillofac Implants 22: 963–968.
- Calvo-Guirado JL, Satorres-Nieto M, Aguilar-Salvatierra A, Delgado-Ruiz RA, Mate-Sanches De Val JE, et al. (2015) Influence of surface treatment on osseointegration of dental implants: histological, histomorphometric and radiological analysis in vivo. Clin Oral Investig 19: 509–517.
- Roberts WE, Smith RK, Zilberman Y, Mozsary PG, Smith RS (1984) Osseous adaptation to continuous loading of rigid endosseous implants. Am J Orthod 86: 95–111.
- Becker W, Becker BE, Israelson H, Lucchini JP, Handelsman M, et al. (1997) One-step surgical placement of Branemark implants: a prospective multicenter clinical study. Int J Oral Maxillofac Implants 12: 454–462.
- Goiato MC, Bannwart LC, Pesqueira AA, Santos DM, Haddad MF, et al. (2014) Immediate loading of overdentures: systematic review. Oral Maxillofac Surg 18: 259–264.
- Penarrocha M, Boronat A, Garcia B (2009) Immediate loading of immediate mandibular implants with a full-arch fixed prosthesis: a preliminary study. J Oral Maxillofac Surg 67: 1286–1293.
- Busenlechner D, Mailath-Pokorny G, Haas R, Furhauser R, Eder C, et al. (2016) Graftless full-arch implant rehabilitation with interantral implants and immediate or delayed loading-part II: transition from the failing maxillary dentition. Int J Oral Maxillofac Implants 31: 1150–1155.
- Zhang S, Wang S, Song Y (2017) Immediate loading for implant restoration compared with early or conventional loading: a meta-analysis. J Craniomaxillofac Surg 45: 793–803.
- Yildiz P, Zortuk M, Kilic E, Dincel M, Albayrak H (2016) Clinical outcomes after immediate and late implant loading for a single missing tooth in the anterior maxilla. Implant Dent 25: 504–509.
- Mundt T, Passia N, Att W, Heydecke G, Freitag-Wolf S, et al. (2017) Pain and discomfort following immediate and delayed loading by overdentures in the single mandibular implant study (SMIS). Clin Oral Investig 21: 635–642.
- Al-Hashedi AA, Taiyeb Ali TB, Yunus N (2014) Short dental implants: an emerging concept in implant treatment. Quintessence Int 45: 499–514.
- Mezzomo LA, Miller R, Triches D, Alonso F, Shinkai RS (2014) Meta-analysis of single crowns supported by short (<10 mm) implants in the posterior region. J Clin Periodontol 41: 191–213.
- Srinivasan M, Vazquez L, Rieder P, Moraguez O, Bernard JP, et al. (2012) Efficacy and predictability of short dental implants (< 8 mm): a critical appraisal of the recent literature. Int J Oral Maxillofac Implants 27: 1429–1437.
- Romeo E, Storelli S, Casano G, Scanferla M, Botticelli D (2014) Six-mm versus 10-mm long implants in the rehabilitation of posterior edentulous jaws: a 5-year follow-up of a randomised controlled trial. Eur J Oral Implantol 7: 371–381.
- Gulje F, Abrahamsson I, Chen S, Stanford C, Zadeh H, et al. (. 2013) Implants of 6 mm vs. 11 mm lengths in the posterior maxilla and mandible: a 1-year multicenter randomized controlled trial. Clin Oral Implants Res 24:1325–1331.
- Boyne PJ, James RA (1980) Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg 38: 613–616.
- Cosci F, Luccioli M (2000) A new sinus lift technique in conjunction with placement of 265 implants: a 6-year retrospective study. Implant Dent 9: 363–368.
- Palmer P, Palmer R (1999) Dental implants. 8. Implant surgery to overcome anatomical difficulties. Br Dent J 187: 532–540.
- Raghoebar GM, Schortinghuis J, Liem RS, Ruben JL, Van Der Wal JE, et al. (2005) Does platelet-rich plasma promote remodeling of autologous bone grafts used for augmentation of the maxillary sinus floor? Clin Oral Implants Res 16: 349–356.
- Duret F, Blouin JL, Duret B (1988) CAD-CAM in dentistry. J Am Dent Assoc 117: 715–720.
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Citation: Anderson H (2022) Innovative Dental Implant Technologies. J Oral Hyg Health 10: 326. DOI: 10.4172/2332-0702.1000326
Copyright: © 2022 Anderson H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2149
- [From(publication date): 0-2022 - Apr 08, 2025]
- Breakdown by view type
- HTML page views: 1681
- PDF downloads: 468