Initial Long-Term Findings from a Multimodal Treatment Program for Child Sexual Abuse Victims Demonstrate Reduction of PTSD Frequency and Symptoms
Received: 02-May-2016 / Accepted Date: 30-May-2016 / Published Date: 03-Jun-2016 DOI: 10.4172/2375-4494.1000297
Abstract
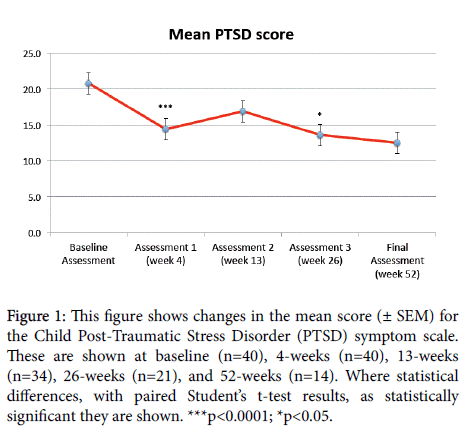
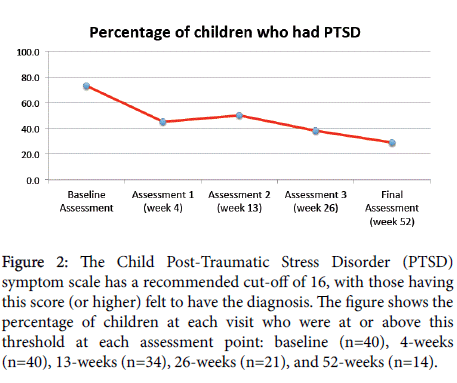
It is well recognized that sexually abused children frequently experience long-term negative outcomes including Posttraumatic Stress Disorder (PTSD). To assist victims, a long-term, multimodal approach was developed at the “Be Brave Ranch” (BBR), a treatment facility specifically designed for this program. This paper reports on the initial long-term (1-year) findings from the first 40 children to attend BBR, aged 8-12 (mean age 10.0), of whom 27 were female and 13 were male. While the program remains in progress, here we report here on the results of those who have completed Baseline visits and Assessment #2 at the end of 4-weeks (n=40), those who have completed Assessment #3 at 13-weeks (n=34), those who have completed Assessment #4 at 26-weeks (n=21), and those who have completed Assessment #5, final visit, at 52-weeks (n=14). Of the 40 children who entered the BBR program, two have dropped out, one between Assessment #2 and Assessment #3 and the other between Assessment #3 and Assessment #4. The findings from data collected as part of the standard program demonstrate highly statistically significant reductions in Child Posttraumatic Stress Disorder Symptom Scale (CPSS) scores, which decreased from a mean score at baseline of 20.8 ± 1.4 to a mean of 12.5 ± 2.3 at 52-weeks. There was also a marked reduction in the percentage of children whose scores were above threshold for the diagnosis of PTSD, decreasing from 73% at baseline to 29% at 52-weeks. It should be noted that while much of the reduction in mean CPSS scores occurred in the first 4-weeks, the percentage reduction in those who met criteria for PTSD continued over time. These initial longer-term findings support the utility of this program, but further research is required to determine the potential role of each of the elements of this multimodal program.
Keywords: PTSD; Child; Sexual abuse; CSA; Residential; Therapy; Multimodal; Intensive
218650Introduction
Incidents of child sexual abuse (CSA) are a common occurrence in our society, particularly for female children [1-6], with most CSA never being reported to the authorities [2]. Victims of CSA routinely experience long-term negative outcomes [7-10] including multiple psychological issues [9-14], often linked to feelings of shame [15-17]. Posttraumatic Stress Disorder (PTSD) is consistently found in this population and is associated with poorer long-term outcomes [18-21]. There is some evidence to suggest that these negative outcomes are the result of underlying neurobiological changes that occur following CSA [22-24]. More recently, evidence has emerged supporting the efficacy of brief intensive interventions for PTSD [25,26]. Thus, CSA is common, severe, and can have major negative long-term impacts on the lives of the victims. Despite this, the most effective treatment approaches remain uncertain, although several studies suggest that trauma-focused cognitive behavioural therapy (TF-CBT) can be effective for many children [7,27,28]. TF-CBT consists of (1) skillsbuilding components to enhance children’s affective, behavioural, biological, and cognitive self-regulation; gradual exposure to the child’s trauma reminders is included throughout these components; (2) trauma narrative (TN) during which children describe and cognitively process their personal trauma experiences; and (3) treatment closure including conjoint caregiver–child sessions and safety planning [29]. Typically, one third of TF-CBT treatment is dedicated to each of these modules, and its benefits have been shown to be continued over extended periods in children who have been victims of CSA [29].
Other treatment modalities that have been found to be effective, but in a more limited range of studies, including eye movement desensitization and reprocessing (EMDR), animal-assisted therapy, art-therapy, and play therapy [7,30-34]. Recent review have determined that both individual and group therapy can be helpful, but multiple questions remain about what is the best form of therapy for an individual child or youth, and how this may vary depending upon their age, gender, and type of CSA [7,34]. Additionally, many of the therapies used in the treatment of CSA were proposed over 30 years ago, but the research on the effectiveness for many of these is poor. Other key issues also remain about the length of treatment and how this could be standardized [8,35,36]. Provision of treatment is also difficult, with significant access issues for children and youth who have experienced CSA [37,38]. In terms of treatment modalities for interventions no single therapy (such as TF-CBT) has proved effective for all individuals [29], and it is possible that a combined approach may be more useful [7,34]. If so, it is uncertain which are key components, and whether such a complex multimodal intervention could be of benefit.
Given this large unmet need for effective treatments, and uncertainty about the most appropriate form (or combinations) of therapy, there is a need for novel approaches in addition to those available at this time. Currently, many treatment approaches for victims of CSA are based on out-patient programs offering 12-20 sessions occurring once-per-week. However, co-location of treatments with an integrated model “is considered the gold standard” of treatment by some [34]. For these reasons, and in collaboration with the University of Alberta, a novel program was designed to include multiple therapies, all of which had some evidence of efficacy. Based on recent evidence the program was also designed to provide brief, but more intensive, interventions as these appear to be effective in treating PTSD. The novel program was implemented at the Be Brave Ranch in 2014 for children aged 8-12 who have been victims of CSA. It is currently a 1-year treatment program involving visits to a “camp-like” facility called the “Be Brave Ranch” (BBR). Because of the age-group involved, it was felt important that any program at BBR also involved components of play and artistic activities, and so these were incorporated into the program. The goal of the program was to provide support to both child victims of CSA and their families, and to also try and reduce symptoms typical of PTSD. Should the overall program be efficacious, then research is planned to help determine which aspects of the program are most important in terms of producing longer-term benefits.
The present publication is an interim report of the longer-term outcomes from those children who have attended the BBR facility to date, with the data being analyzed having been collected as part of the standard program. It should be clearly noted, however, that at this time no formal clinical research study has taken place, although these may occur in the future. For this reason, it is not possible at this time to identify the possible importance of any of the individual components, and future research will be necessary to determine how important each of the various components of this complex intervention is in terms of overall outcomes (such as the role of TF-CBT alone and how important physical activity is). To determine these matters, appropriate future clinical research studies will need to be carried out, ideally working with other groups to enhance generalizability.
Methods
The program involves a 4-week initial stay at BBR, where intensive therapeutic interventions are employed for 8-10 hours from Monday to Friday. Weekends are dedicated to a variety of community-based recreational activities. Children return to the BBR for further interventions, followed by additional reassessment at 13-weeks, 26- weeks, and 52-weeks. Assessments of progress take place before starting at the BBR (“Baseline”) at the end of the initial 4-week stay (“Assessment #2”), at the end of the 13-week stay (“Assessment #3”), at the end of the 26-week stay (“Assessment #4”), and at the end of the final 52-week visit (“Assessment #5”).
Additional interventions occur during 2-week periods to facilitate multiple therapeutic modules being used. BBR is a 130-acre “camplike” facility with fully equipped communal lodges located in rural Alberta, Canada. All children at BBR have secure, private bedrooms of their own. Parents who live within driving distance frequently visit their children at BBR, staying in the “parent’s house” located in the same facility. Out-of town parents typically have telephone calls or Skype sessions with their child on a daily basis. Due to the complex, intensive nature of the program, BBR maintains a high staff ratio of one adult to every four children. The facility has ongoing inspections to ensure its compliance with all safety and regulatory guidelines, and the site is secured by a surrounding fence, multiple camera, and dedicated security personnel.
Central to the program is the daily TF-CBT group, which comprises 100 hours of group therapy across 12 months. Treatment fidelity is ensured through the use of a detailed program guide as well as daily clinical consultations and weekly team meetings. As noted, and consistent with previous evidence, the TF-CBT component of the BBR program focuses on: (1) developing self-regulation skills; (2) supportive discussions about the child’s CSA experience; (3) processing the child’s trauma narrative; and (4) conjoint caregiver–child sessions, as well as safety planning to facilitate appropriate closure [29]. During each of their visits to BBR, children repeat the sharing of their trauma narrative. This approach is consistent with a study of adolescent CSA victims where it was found that repeated exposure to the trauma was more efficacious than supportive therapy alone [39].
In conjunction with TF-CBT, BBR’s multimodal program involves a number of other interventions including daily cardiovascular exercise, yoga, music, art, EMDR, individual counselling, and interactions with animals, most of which have some level of evidence supporting efficacy in the treatment of CSA [7].
Each of these activities were also closely defined and manualized, and appropriately supervised. The manual included detailed clarification of specific games, art, and other activities carried out each day to help support the specific daily objectives of the TF-CBT program at that time. For example, after pilot work, it was determined that during the 4-week stay there would be 4-days in which there was therapeutic role playing, with the staff and children dressing up and spending the day in full costume playing therapeutically beneficial characters. Children were usually entered into the program in cohorts of 4 or 5 who would progress through the program at the same time, and share accommodation with their own room in a specific lodge.
Criteria for attendance at the be brave ranch (BBR)
The program is currently for children aged 8-12 who have experienced childhood sexual abuse. They had to be developmentally developed enough to be in an on-site “camp-like” facility, had to be able to perform skills of daily living for self-care, and in stable physical health. All children had to be voluntary attendees, and specifically agree to attend the program in a 1:1 interview with a staff member (which was be carried out either in person or via electronic means). They also had to have written parental/guardian support to attend. Those children who had severe mental health or behavioural issues were not felt to be appropriate for the BBR. To make parents and children who may be interested in attending the BBR aware of the program, a wide social media campaign was launched. It should also be noted that all costs for the program to date have been met by donations from charitable sources, and so there has been no cost for children or their relatives to attend the program to date. All consecutive children who met these criteria were invited to attend the BBR program, and form the basis of this report. However, it is important to recognize that this group may (or may not) be typical of the wider group of children aged 8-12 who have experienced CSA. This is for many reasons, including the fact that at least 95% of CSA is not reported to authorities [2], that those who responded to the information on social media may not be typical of the wider group of CSA survivors of this age group, and that several potential children who would like to have come to the BBR had significant pre-existing mental health or behavioural issues that precluded this (approximately as many children were unable to attend for these reasons as did attend). Lastly, the requirement that children attend a residential program also likely limited the potential group of applicants. Therefore, is it not possible for any findings from the current research to be considered generalizable.
Measurement
As a standard part of the program, all children completed baseline measurements of PTSD symptoms, as measured by the Child Post- Traumatic Stress Disorder symptom scale (CPSS) which was designed to be used in children aged 8-18 [40-42]. All children then repeated this at the end of each time they had attended the BBR, again as part of the standard clinical determination of progress. This scale has a total of 24 items and includes two parts; the first has 17-items and measures the type and frequency of PTSD symptoms (mapping directly on to DSM-IV criteria), each of which is can be scored on a scale of 0, 1, 2, and 3. The questions ask about how much each problem has bothered the individual during the previous 2 weeks. The CPSS can be thus be used as a continuous measure of symptom severity (summation of items 1–17 with possible scores ranging from 0 to 51). Several studies of the psychometric properties of the CPSS suggest that a score of 16 or more is highly likely to indicate clinically significant PTSD [40-42]. This scale also includes an additional second part which has 7 items, and measures the degree of functional impairment these symptoms cause, but we did not utilize this second part in our program. Improvements in PTSD symptoms would lead to a decrease in score.
The clinical team met daily to discuss progress. However, to be able to compare the effectiveness of the present program with other such programs, here we present the data collected on PTSD scores.
This program adhered to all appropriate laws and regulations regarding confidentiality of data. However, it is important to note that while all information was confidential, there were two specific legal issues regarding confidentiality that were made clear to all participating children and their parents/guardians.
• Child Abuse: if a disclosure was made about abuse (physical, emotional, sexual, neglect) of a child, it was reported it to Alberta Child and Family Services and/or any other appropriate authorities.
• Harm to self or others: if a disclosure was made about immediate or risk of self-harm, or harm to another client, staff would act appropriately including (as necessary) calling emergency services, the individual’s family, or taking the child to a place of safety.
We used a paired design, in which each child who completed baseline ratings and follow-up ratings was their own control. We have analyzed the data using two separate methods, since some individuals have not yet completed the program and therefore there is some missing data points. We firstly utilized a repeated-measure analysis of variance (RM-ANOVA) utilizing a last-observation carried forward (LOCF) to account for missing data points. We then performed a posthoc Tukey-Kramer multiple comparison test comparing Baseline data to each of the subsequent visits. In all cases we utilized p<0.05 as the criteria for statistical significance. In addition, we also separately carried out a statistical analysis using paired Student’s t-tests between Baseline and each subsequent group, but on the existing data only, not with LOCF. Again, statistical significance was determined as p<0.05. All data is reported as mean ± standard error of the mean (SEM).
Results
A total of 40 children entered the program in the time period September 2014 – January 2016, and these form the basis of this interim report. Of these children, 27 were female and 13 were male, with a mean age of 10.0 ± 0.5 years overall. Since the program is in progress, the results report on those who have completed Baseline assessment followed by the first 4-weeks (40 children) at Asssement #2, those who have completed 13-weeks (34 children) at Assessment #3, those who have completed 26-weeks (21 children) at Assessment #4, and those who have completed 52-weeks (14 children) at Assessment #5. Of those who entered the program there were 2 children who have dropped out, one between the 4-week and 13-week assessments, and one other between the 13-week and 26-week assessments.
It is important to note that once trust had been established, several children made significant additional disclosures to BBR staff, all of which were reported to parents and law enforcement. While there were no significant episodes of self-harm (requiring any medical intervention), several children engaged in periodic self-harming behaviour including banging heads against walls, scratching/picking behaviour, squashing themselves into tights spaces etc. All such instances were treated as therapeutic opportunities and clinical staff worked with the children to teach them more appropriate coping strategies. Parental and/or guardian participation varied. In several instances children would travel from long distances, sometimes by airplane, in which case they were met at the airport and didn’t usually have parental and/or guardian visits. Relatively few parents participated on a daily basis, either in person or on the telephone, but were continuously encouraged to do so.
In terms of CPSS scores, at Baseline the mean scores were 20.8 ± 1.4, with 29 (73%) of the children having scores of at least 16. At 4-weeks the mean scores were 14.4 ± 1.4, with 18 (45%) of the children having scores of at least 16. At 13-weeks the mean scores were 16.9 ± 1.8, with 17 (50%) of the children having scores of at least 16. At 26-weeks the mean scores were 13.6 ± 1.9, with 8 (38%) of the children having scores of at least 16. At 52-weeks the mean scores were 12.5 ± 2.3, with 4 (29%) of the children having scores of at least 16.
Utilizing a RM-ANOVA with LOCF then F=8.65, p<0.0001, suggesting a highly statistically significant outcome. Utilizing post-hoc Tukey-Kramer testing, then with the current data a “q” score greater than 3.91 gives p<0.05. The results showed that the post-hoc test was significant at each time point: Baseline vs. Visit #2, mean difference=6.38, q=6.73, p<0.001; Baseline vs. Visit #3, mean difference=4.45, q=4.70, p<0.05; Baseline vs. Visit #4, mean difference=5.95, q=6.28, p<0.001; Baseline vs. Visit #5 (final visit), mean difference=6.83, q=7.21, p<0.01.
Utilizing Students t-test for paired data the differences between the mean scores were highly statistically significant at the 4-week assessment (p<0.0001, t=4.50, df=39) and statistically significant at the 26-week assessment (p<0.01, t=2.84, df=20). At 13-weeks they did not quite meet standards for statistical significance (p=0.056, t=1.98, df=33). These data are shown in Figures 1 and 2 respectively.
Figure 1:This figure shows changes in the mean score (± SEM) for the Child Post-Traumatic Stress Disorder (PTSD) symptom scale. These are shown at baseline (n=40), 4-weeks (n=40), 13-weeks (n=34), 26-weeks (n=21), and 52-weeks (n=14). Where statistical differences, with paired Student’s t-test results, as statistically significant they are shown. ***p<0.0001; *p<0.05.
Figure 2:The Child Post-Traumatic Stress Disorder (PTSD) symptom scale has a recommended cut-off of 16, with those having this score (or higher) felt to have the diagnosis. The figure shows the percentage of children at each visit who were at or above this threshold at each assessment point: baseline (n=40), 4-weeks (n=40), 13-weeks (n=34), 26-weeks (n=21), and 52-weeks (n=14).
Discussion
The present results are supportive of the anecdotal experiences of the treatment staff that the comprehensive program leads to a clinically meaningful improvement in the symptoms of PTSD. This would support suggestions that such an intensive approach could be more widely utilized. A potential advantage to children aged 8-12 of the current program is that it occurs in a residential facility, as many of them otherwise have no access to appropriate therapy (for geographical and other reasons). Given the fact that there is a lack of clinical treatment programs that demonstrate similar levels of improvement in PTSD symptoms, at least in this age group of CSA survivors, this may be a valuable addition to the treatment options available.
However, because several activities occurred during the program, the clinical and PTSD scale score improvements cannot be tied to a single isolated part of the program. In future, it would be helpful to carry out clinical research studies to determine the relative importance of the TF-CBT program alone. Such a study could conceivably be done by utilizing the same TF-CBT program, but administered on an outpatient basis only. Unfortunately, this may be difficult to administer because of lack of access in many remote areas, but in urban settings it may be possible to perform such a research study. It is also not possible to exclude any therapeutic benefits that derived from the “camp-like” environment and extra activities that this involved, including the physical exercise. It is conceivable that this may have contributed to the clinical improvements, but again comparison with an appropriate outpatient approach would help clarify this. In this regard, consideration should be given to a recent intensive outpatient intervention, which gave 14 – 21 hours of exposure therapy to adolescent female rape victims over 3 months, and which reported significant reductions in CPSS scale scores [39]. Interestingly, this specific therapeutic intervention was much more effective than supportive counseling. This would suggest that the therapeutic intervention itself was the primary reason for the reduction in CPSS scores, and that non-specific interventions or activities may be less effective. In the future, it would also be potentially useful to determine if the present BBR program is effective in helping PTSD symptoms in older children, and also if it is effective for children who have experienced different kinds of trauma.
One of the key issues that needs to be addressed is how to minimize future CSA. While the present program addresses a treatment approach, clearly prevention is to be far preferred. One approach we are actively working on is to design a novel program for adults to increase their knowledge about CSA and to change their behaviours to help them recognize it (and prevent it). This program involves educating adults in positions of trust and authority and determining if through both individual, and organization, changes CSA can be prevented. Clearly, a combination of prevention and effective treatment are required to address this complex and challenging issue that can lead to very long-term problems for victims [7-21].
In conclusion, the present paper presents results from a novel comprehensive residential program for child survivors of sexual abuse. It is currently being used in those aged 8-12, which is often prior to the onset of many possible self-destructive behaviours, such as self-harm and addiction issues. The interim data presented from the first 40 children to take part suggests that this program significantly decreases the symptoms of PTSD. Whle it is not clear at present what components of the program may be most effective, this complex intervention does seem to have both short-term and longer-term impacts. The availability of a program with clinically meaningful improvements is a useful additional treatment option, and can potentially be implemented more widely. Clinical research on the various components is warranted in the future, as is comparison to out-patient programs.
Acknowledgement
We wish to thank the following individuals who were instrumental in program implementation: Fern Ashton, Yona McGinnis, Megan Ivancic, Danielle Fiddler, and Janine Groeneveld.
References
- Fang X, Fry DA, Brown DS, Mercy JA, Dunne MP, et al. (2015) The burden of child maltreatment in the East Asia and Pacific region. Child Abuse Negl 42: 146-162.
- Martin EK, Silverstone PH (2013) How Much Child Sexual Abuse is "Below the Surface," and Can We Help Adults Identify it Early? Front Psychiatry 4: 58.
- Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, et al. (2009) Burden and consequences of child maltreatment in high-income countries. Lancet 373: 68-81.
- Finkelhor D (1994) Current information on the scope and nature of child sexual abuse. Future Child 4: 31-53.
- Pereda N, Guilera G, Forns M, Gómez-Benito J (2009) The international epidemiology of child sexual abuse: a continuation of Finkelhor (1994). Child Abuse Negl 33: 331-342.
- Chiu GR, Lutfey KE, Litman HJ, Link CL, Hall SA, et al. (2013) Prevalence and overlap of childhood and adult physical, sexual, and emotional abuse: a descriptive analysis of results from the Boston Area Community Health (BACH) survey. Violence Vict 28: 381-402.
- Greenspan F, Moretzsohn AG, Silverstone PH (2013) What treatments are available for childhood sexual abuse, and how do they compare? International Journal of Advances in Psychology 2: 232-241.
- Finkelhor D, Berliner L (1995) Research on the treatment of sexually abused children: a review and recommendations. J Am Acad Child Adolesc Psychiatry 34: 1408-1423.
- Chen LP, Murad MH, Paras ML, Colbenson KM, Sattler AL, et al. (2010) Sexual abuse and lifetime diagnosis of psychiatric disorders: systematic review and meta-analysis. Mayo Clin Proc 85: 618-629.
- Maniglio R (2009) The impact of child sexual abuse on health: a systematic review of reviews. Clin Psychol Rev 29: 647-657.
- Vloet A, Simons M, Vloet TD, Sander M, Herpertz-Dahlmann B, et al. (2014) Long-term symptoms and posttraumatic growth in traumatised adolescents: findings from a specialised outpatient clinic. J Trauma Stress 27: 622-625.
- Kajeepeta S, Gelaye B, Jackson CL, Williams MA2 (2015) Adverse childhood experiences are associated with adult sleep disorders: a systematic review. Sleep Med 16: 320-330.
- Wosu AC, Gelaye B, Williams MA (2015) History of childhood sexual abuse and risk of prenatal and postpartum depression or depressive symptoms: an epidemiologic review. Arch WomensMent Health 18: 659-671.
- O'Brien BS, Sher L (2013) Child sexual abuse and the pathophysiology of suicide in adolescents and adults. Int J Adolesc Med Health 25: 201-205.
- Kendall-Tackett KA, Williams LM, Finkelhor D (1993) Impact of sexual abuse on children: a review and synthesis of recent empirical studies. Psychol Bull 113: 164-180.
- Pettersen KT (2013) A study of shame from sexual abuse within the context of a Norwegian incest center. J Child Sex Abus 22: 677-694.
- Feiring C, Simon VA, Cleland CM, Barrett EP (2013) Potential pathways from stigmatization and externalizing behavior to anger and dating aggression in sexually abused youth. J Clin Child AdolescPsychol 42: 309-322.
- Schönbucher V, Maier T, Mohler-Kuo M, Schnyder U, Landolt MA (2012) Disclosure of child sexual abuse by adolescents: a qualitative in-depth study. J Interpers Violence 27: 3486-3513.
- Cort NA, Gamble SA, Smith PN, Chaudron LH, Lu N, et al. (2012) Predictors of treatment outcomes among depressed women with childhood sexual abuse histories. Depress Anxiety 29: 479-486.
- Aydin B, Akbas S, Turla A, Dundar C, Yuce M, et al. (2015) Child sexual abuse in Turkey: an analysis of 1002 cases. J Forensic Sci 60: 61-65.
- Gospodarevskaya E1 (2013) Post-traumatic stress disorder and quality of life in sexually abused Australian children. J Child Sex Abus 22: 277-296.
- Ehlert U (2013) Enduring psychobiological effects of childhood adversity. Psychoneuroendocrinology 38: 1850-1857.
- De Bellis MD, Spratt EG, Hooper SR (2011) Neurodevelopmental biology associated with childhood sexual abuse. J Child Sex Abus 20: 548-587.
- Enlow MB, Egeland B, Blood EA, Wright RO, Wright RJ (2012) Interpersonal trauma exposure and cognitive development in children to age 8 years: a longitudinal study. J Epidemiol Community Health 66: 1005-1010.
- Ehlers A, Hackmann A, Grey N, Wild J, Liness S, et al. (2014) A randomized controlled study of 7-day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. Am J Psychiatry 171: 294-304.
- Cloitre M (2014) Alternative Intensive Therapy for PTSD. Am J Psychiatry 171: 249-251.
- Mannarino AP, Cohen JA, Deblinger E, Runyon MK, et al. (2012) Trauma-focused cognitive-behavioural therapy for children sustained impact of treatment 6 and 12 months later. Child Maltreat 17: 231-241.
- Gillies D, Taylor F, Gray C, O'Brien L, D'Abrew N (2012) Psychological therapies for the treatment of post-traumatic stress disorder in children and adolescents. Cochrane Database Syst Rev 12: CD006726.
- Gillies D, Taylor F, Gray C, O'Brien L, D'Abrew N (2013) Psychological therapies for the treatment of post-traumatic stress disorder in children and adolescents (Review). Evid Based Child Health 8: 1004-1116.
- Scott TA, Burlingame G, Starling M, Porter C, Lilly JP (2003) Effects of individual client-centered play therapy on sexually abused children’s mood, self-concept, and social competence. Int J Ther 12: 7-30.
- Pifalo T (2006) Art therapy with sexually abused children and adolescents: Extended research study. Art Ther 23: 181-185.
- Dietz TJ, Davis D, Pennings J (2012) Evaluating animal-assisted therapy in group treatment for child sexual abuse. J Child Sex Abus 21: 665-683.
- Ewing CA, Macdonald PM, Taylor M, Bowers MJ (2007) Equine-facilitated learning for youths with severe emotional disorders: a quantitative and qualitative study. Child Youth Care Forum 36: 59-72.
- Cummings M, Berkowitz SJ, Scribano PV (2012) Treatment of childhood sexual abuse: an updated review. Curr Psychiatry Rep 14: 599-607.
- Keeshin BR, Strawn JR, Luebbe AM, Saldaña SN, Wehry AM, et al. (2014) Hospitalized youth and child abuse: a systematic examination of psychiatric morbidity and clinical severity. Child Abuse Negl 38:76-83.
- Kolko DJ, Baumann BL, Caldwell N (2003) Child abuse victims' involvement in community agency treatment: service correlates, short-term outcomes, and relationship to reabuse. Child Maltreat 8:273-287.
- Paul LA, Gray MJ, Elhai JD, Massad PM, Stamm BH (2006) Promotion of evidence-based practices for child traumatic stress in rural populations: identification of barriers and promising solutions. Trauma Violence Abuse 7: 260-273.
- Holm JW, Hansen DJ (2004) Examining and addressing potential barriers to treatment adherence for sexually abused children and their non-offending parents.
- Foa EB, McLean CP, Capaldi S, Rosenfield D (2013) Prolonged exposure vs supportive counseling for sexual abuse–related PTSD in adolescent girls: a randomized clinical trial. JAMA 310: 2650-2657.
- Foa EB, Johnson KM, Feeny NC, Treadwell KR (2001) The child PTSD Symptom Scale: a preliminary examination of its psychometric properties. J Clin Child Psychol 30:376-384.
- Gillihan SJ, Aderka IM, Conklin PH, Capaldi S, Foa EB (2013) The child PTSD symptom scale: psychometric properties in female adolescent sexual assault survivors. Psychol Assess 25: 23-31.
- Nixon RD, Meiser-Stedman R, Dalgleish T, Yule W, Clark DM, et al. (2013) The Child PTSD Symptom Scale: an update and replication of its psychometric properties. Psychol Assess 25: 1025-1031.
Citation: Linder JM, Silverstone PH (2016) Initial Long-Term Findings from a Multimodal Treatment Program for Child Sexual Abuse Victims Demonstrate Reduction of PTSD Frequency and Symptoms. J Child Adolesc Behav 4: 297. DOI: 10.4172/2375-4494.1000297
Copyright: © 2016 Linder JM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 12162
- [From(publication date): 6-2016 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 11195
- PDF downloads: 967