Inflammation and Immunological Responses in Atherosclerosis: Origins and Therapeutic Targets for Innovative Cardiovascular Disease (CVD) Therapies
Received: 02-May-2023 / Manuscript No. asoa-23-100322 / Editor assigned: 04-May-2023 / PreQC No. asoa-23-100322 (PQ) / Reviewed: 18-May-2023 / QC No. asoa-23-100322 / Revised: 24-May-2023 / Manuscript No. asoa-23-100322 (R) / Accepted Date: 30-May-2023 / Published Date: 31-May-2023 DOI: 10.4172/asoa.1000211
Abstract
This study focuses on atherosclerosis, a prominent cause of cardiovascular disease (CVD). Atherosclerosis is a chronic inflammatory disorder characterised by immunological competent cells in lesions that primarily generate proinflammatory cytokines. The presence of dead cells and oxidised versions of low density lipoproteins (oxLDL) is significant in this syndrome. The rupture of atherosclerotic plaques is the main cause of CVD. At larger concentrations, oxLDL has features that promote inflammation and immunological activation, causing cell death. It also includes inflammatory phospholipids, notably phosphorylcholine (PC), which is an intriguing epitope. Antibodies that target PC (anti-PC) may have atheroprotective benefits, possibly due to their anti-inflammatory qualities. While the participation of bacteria and viruses in atherosclerosis has been discussed, direct proof has been difficult to come by, and antibiotic studies have failed. Heat shock proteins have the potential to be targets for atherogenic immune responses. Pro-inflammatory cytokines, chemokines, and lipid mediators are other contributors in plaque rupture. To establish inflammation as a cause of atherosclerosis and CVD, clinical trials using anti-inflammatory and immune-modulatory therapy are required. This review investigates the possible origins of immunological responses and inflammation in atherosclerosis, as well as therapeutic techniques that target inflammation for innovative CVD therapies.
Keywords
Atherosclerosis; Inflammation; Cardiovascular disease; Immune reactions; Cytokines; Therapeutic approaches; Atherothrombosis
Background
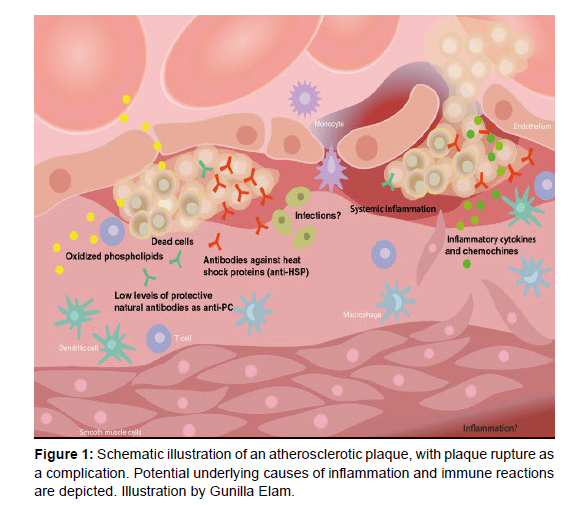
Atherosclerosis, the leading cause of cardiovascular disease (CVD), which includes disorders such as myocardial infarction, heart failure, stroke, and claudication, arises mostly in the intima of medium-sized and large arteries, particularly near arterial division sites. This localisation may be altered by blood flow dynamics, since regions exposed to normal shear stress have protective properties, with endothelial cells expressing anti-atherosclerosis genes [1]. Furthermore, adventitia, which is characterised by lymphocyte infiltrates, may have a role in the development of atherosclerosis [2]. Atherosclerotic lesion and offers an outline of the potential mechanisms that lead to inflammation and immunological responses inside it (Figure 1). The activation of endothelium in the early stages of atherosclerosis is marked by the expression of adhesion molecules, which allows mononuclear leukocytes such as monocytes, T-cells, and, to a lesser extent, dendritic cells, mast cells, neutrophils, and B-cells to adhere to and infiltrate the intima. Smooth muscle cells (SMC) in lesions phenotypically convert into synthetic SMC and move from the media towards the intima. The number of immunological capable cells in lesions, which produce cytokines, particularly proinflammatory cytokines, supports the inflammatory character of atherosclerosis [3].
The significance of immunity in atherosclerosis, specifically the participation of activated T-cells and B-cells, is poorly known, particularly in humans. Emerging evidence shows, however, that immunological variables contribute to inflammation in humans and that immune regulation can impact atherosclerosis in animal models, notably mice [4]. As a result, discussing inflammation and immunity in the context of atherosclerosis is critical. While atherosclerosis can induce decreased blood flow owing to stenosis, which can contribute to CVD, the predominant mechanism is atherothrombosis, which happens when plaques are destroyed. When a plaque ruptures, it exposes prothrombotic material to the coagulation system, resulting in decreased blood flow and the development of CVD. Hypertension, smoking, diabetes, and dyslipidemia are major modifiable risk factors for atherosclerosis (and CVD), with age and male sex also playing important roles [4]. This study focuses on the probable direct causes of inflammation and immunological reactivity in atherogenesis and plaque problems, taking both genetic and epigenetic variables into account. Oxidised low-density lipoprotein (LDL) and associated chemicals are early contributors to atherosclerosis. During the early stages of atherosclerosis, LDL penetrates the intima and attaches to the proteoglycan matrix, where it is further modified by oxidation or enzymatic activities to generate oxidised LDL (oxLDL). Even in advanced stages, oxLDL and similar chemicals are abundant in lesions [5,6]. OxLDL is immunogenic, activating endothelial cells, monocytes/ macrophages, and T cells [7-9]. Higher oxLDL concentrations are hazardous and can cause cell death inside lesions. Enzymatically modified LDL, promoted by phospholipase 2 (PLA2) production in both normal and atherosclerotic lesions, may play a substantial role and can activate dendritic cells [10,11]. Inflammatory phospholipids seen in atherosclerotic lesions, such as lysophosphatidylcholine (LPC), imitate the proinflammatory and immune-stimulatory properties of oxLDL [12,13]. These phospholipids, which include LPC, have phosphorylcholine (PC) as a critical epitope that allows them to interact with the platelet activating factor (PAF)-receptor, which is one of the methods through which oxLDL exerts its effects [14,15].
Interaction with Toll-like receptors and scavenger receptors is involved in other pathways [16,17]. Aside from oxidised and/or enzymatically changed phospholipids, there are numerous other probable reasons of oxidised LDL (oxLDL)’s pro-atherogenic and pro-inflammatory actions. Epitopes revealed during LDL modification and/or oxidation have been postulated to constitute a conserved evolutionary system of danger-associated molecular patterns (DAMP), comparable to pathogen-associated molecular patterns (PAMP). Malondialdehyde (MDA), which is formed during the oxidation of LDL, is an example of a DAMP, along with phospholipid (PL)-related epitopes like PC. Adducts of MDA develop on proteins, peptides, carbohydrates, and DNA. Modified and oxidised versions of apoB and cholesterol may potentially play a role, however the particular processes involving these molecules are not as well-known as those involving PC-exposing epitopes. While epidemiological studies show a strong association between smoking and atherosclerosis and CVD [18,19], the particular mechanisms by which smoking causes artery inflammation remain unknown. Increased lipid oxidation is one intriguing explanation, as smoking has been linked to higher amounts of oxidised lipids [20]. Smoking enhances the formation of atherosclerotic lesions in animal models studied for the link between smoking and atherosclerosis [21- 23], with oxidative stress being one suggested underlying mechanism [24]. Clinical research has revealed evidence that inflammatory phospholipids have a role in atherosclerosis. In diseases linked with increased atherosclerosis, such as hypertension and systemic lupus erythematosus (SLE), we have shown an increase in PC-exposing LDL [25]. Diabetes-related oxidative stress can potentially contribute to atherogenesis by increasing LDL oxidation [26]. Another possible factor contributing to atherosclerosis (and CVD) in diabetes is the production of advanced glycation end products (AGEs), which have proinflammatory and potentially atherogenic features.
Dead cells
The involvement of cell death in atherosclerosis and plaque rupture is complicated and likely changes based on the stage of the illness as well as the kind of cell death involved, such as apoptosis or necrosis. It is possible that a lack of apoptotic cell clearance, resulting in necrosis, might contribute to inflammation. Dying cells can stimulate the innate immune system and initiate an inflammatory response, which is characterised by the production of the proinflammatory cytokine IL-1beta, which activates the inflammasome. The production of endogenous factors known as damage-associated molecular patterns (DAMPs) following cell death, according to the danger hypothesis, might cause inflammation [27]. DAMPs include molecules like highmobility group protein B1 (HMGB-1) and double-stranded DNA, as well as amyloid-peptides and heat-shock proteins (HSP). While cell death does not appear to be an early event in the development of atherosclerosis (the creation of fatty streaks and the infiltration of monocytes/macrophages and T cells appear to occur earlier), it may contribute to inflammation later on. Cell death may have a role in plaque rupture, however this has yet to be demonstrated convincingly.
Phospholipid-related epitopes
Antibodies that target phospholipids (aPL), namely cardiolipin (aCL), have been associated to cardiovascular disease (CVD), notably in people with systemic lupus erythematosus (SLE). However, conclusive proof of aPL as a causal factor in atherosclerosis has been difficult to establish, with both positive and negative findings published [25]. We found no link between aPL and the occurrence of atherosclerotic plaques in SLE patients in a recent research. Pathogenic aPL often rely on plasma cofactors to induce CVD, such as beta2-glycoprotein I (beta2GPI). Direct effects on the endothelium and interaction with anticoagulant proteins such Annexin A5 are two possible mechanisms of action.
Cardiolipin (CL) is present in bacteria as well as the inner mitochondrial membrane of eukaryotic cells and has a characteristic double structure composed of four fatty acid chains. This is noteworthy because mitochondria are thought to have evolved from bacteria. Unlike antibodies against cardiolipin (aCL), our new findings show a negative relationship between antibodies against oxidised forms of cardiolipin (aOxCL) and cardiovascular disease (CVD), with low levels associated with a greater risk and high levels associated with a reduced risk. Unlike aCL, aOxCL is not activated by beta2- glycoprotein I (beta2GPI). One such mechanism is the suppression of oxidised low-density lipoprotein (oxLDL) binding and absorption in macrophages. Natural antibodies that target phosphorylcholine (anti-PC) are another example. Animal studies, experimental studies, and clinical cohort studies all imply that anti-PC may have a role in atherogenesis. Immunisation with pneumococcae resulted in lower atherosclerosis development as well as higher levels of anti-PC antibodies in a mouse model. In mouse models, both passive and active PC immunisation alleviated atherosclerosis. Our published research has repeatedly found a link between immunoglobulin M (IgM) anti- PC and the development of atherosclerosis and the risk of CVD. Low levels are usually associated with an increased risk, whereas high levels are often associated with a lower risk. We were among the earliest to establish that anti-PC is a protective marker against the development of atherosclerosis in humans, equivalent to anti-MDALDL and antioxLDL antibodies. Anti-inflammatory effects, inhibition of proinflammatory actions by inflammatory phospholipids, inhibition of oxLDL uptake via scavenger receptors, and prevention of cell death induced by lysophosphatidylcholine (LPC), a major inflammatory phospholipid are some of the mechanisms by which human anti- PC may mitigate atherosclerosis and CVD. Furthermore, the inflammatory impact of anti-PC was verified in another investigation employing a mouse model, indicating enhanced phagocytosis as one of the mechanisms. Natural IgM antibodies, such as anti-PC, may slow the progression of atherosclerosis by attaching to dead and dying cells within lesions, encouraging phagocytosis and the removal of damaging pro-inflammatory chemicals. Therefore, low levels of anti-PC could potentially contribute to inflammation in atherosclerosis, although the precise mechanisms are not yet fully understood. We have proposed that a Western lifestyle and certain infections uncommon in the Western world could be contributing factors that raise anti-PC levels. Additionally, relatively recent evolutionary factors such as gluten consumption might play a role. Genetic factors may also contribute, as the heritability of anti-PC is estimated to be 37%.
Heat shock proteins
Heat shock proteins (HSPs), notably HSP60 but also perhaps HSP70 and HSP90, are fascinating potential sources of inflammation in atherosclerosis. Cross-reactivity with microbial HSPs, such as those present in bacteria, may potentially cause immunological reactions. Clinical data supports this concept, as there are links between HSP60/65 antibodies and atherosclerosis, and animal research has indicated that HSP60/65 immunisation worsens atherosclerosis. HSPs can also cause inflammation through other methods. HSPs or their peptides can stimulate the immune system in ways other than being particular T-cell antigens given by antigen-presenting cells. HSPs act as chaperones and can generate immunological complexes with other antigens, including tumour antigens. These complexes can be delivered by antigen-presenting pathways of class I or class II. HSPs can be released passively, as in cell necrosis, or actively, as in exosomes. HSPs may operate as endogenous ligands in the extracellular space, activating the innate immune system via Toll-like receptors or by interacting with endotoxins. The processes by which hypertension causes inflammation in the arterial wall remain unknown. One theory is that the endothelium becomes dysfunctional in response to damage, resulting in pro-inflammatory alterations. Previous research suggested that hypertension might cause inflammation by inducing the formation of immunogenic HSP60/65, which is likewise stimulated by oxLDL. Furthermore, we found that HSP70 is a preventive factor against the formation of atherosclerosis in hypertensive people, however the underlying mechanism is unknown. The possible role of infections in immune activation and inflammation in atherosclerosis has received a great deal of attention. Prior to the advent of the lipid theory, pathologists and lesions observers worried about the potential of viral origins based on microscopic and macroscopic aspects of atherosclerosis.
An antibiotic therapy targeting CP was used to undertake a more rigorous test of the infectious theory. Four big trials, however, had negative results and did not support the concept that CP causes cardiovascular illness. However, there might be other explanations for these undesirable effects. Chronic CP infection may be difficult to cure independently of cardiovascular disease, and treatment studies have primarily included individuals with advanced-stage illness, suggesting that early stages may be more responsive. Microorganisms found in the mouth, such as PG and AA, are potentially fascinating candidates. Although clinical and epidemiological research have revealed links, controlling for confounding variables has been difficult, particularly in the context of these drugs. The American Heart relationship has issued a scientific statement acknowledging an independent relationship between periodontal disease and atherosclerosis, although current data do not show causality. Nonetheless, periodontal disease therapies have been shown to reduce systemic inflammation and enhance endothelial function. CMV belongs to the Herpes virus family, which is quite common in the general population, making interpretation of correlations difficult. Notably, there has been evidence of a link between active CMV infection and transplant problems such as vasculopathy. A link between CMV infection and transplant vascular problems looks more feasible than connections with atherosclerosis in general. Many investigations have shown CMV in atherosclerotic lesions, however not consistently. It is worth noting that CMV has been identified in healthy arteries, which suggests that CMV may be an unwitting bystander. CMV, on the other hand, has properties that make it a possible contributor to atherosclerosis. HP, a well-known cause of gastritis and ulcers, has also been linked to cardiovascular disease and atherosclerosis, albeit animal studies have shown less solid data than CP. Nonetheless, there have been instances of decreased cardiovascular disease after HP elimination. HP does not evoke the same local inflammatory response as CP, CMV, and numerous other infections. Notably, no live HP has been isolated from atherosclerotic plaques, and mice tests have shown no conclusive evidence that HP causes atherosclerosis. HIV, Epstein-Barr virus (EBV), influenza, Mycoplasma pneumoniae, and Streptococcus pneumoniae have all been discussed and reported as probable causes of cardiovascular disease and atherosclerosis. Borrelia is another intriguing situation with evidence from human investigations, albeit experimental data or plaque data are not currently accessible to the best of my knowledge. However, the evidence for these drugs is less solid, with no compelling data from human trials. Although the infectious hypothesis has been studied for several decades in cardiovascular disease and atherosclerosis, direct proof of an infectious agent’s causal involvement remains limited, with largely indirect data available. Recent studies involving the gut bacterial ecology are another fascinating development that indirectly links infections, atherosclerosis, and cardiovascular disease. The gut microbiota converts choline and phosphatidylcholine into trimethylamine (TMA), which is then converted into proatherogenic trimethylamine-N-oxide (TMAO). Recent research has shown that the intestinal microbiota’s metabolism of dietary l-carnitine in red meat creates TMAO and promotes atherosclerosis in mice. These data point to a possible relationship between gut flora and atherosclerosis. Pathogens use PC in this context to generate a favourable environment for themselves in the host. One fascinating theory is that PC exposed in atherosclerotic plaque modifies the local immune response into an unresolved chronic inflammation, much like PC-exposing bacteria do in chronic infections. More study is needed to establish if the reported connections have a causal effect in people. Although ideas on the order of events in the development of atherosclerosis differ, it is probable that numerous variables interact. Furthermore, there may be individual differences, with some people having greater inflammation in their atherosclerotic lesions than others. Infection may also have a substantial influence in some subgroups of people and patients. In addition to the well-studied immune responses in the intima, novel elements of immunological processes in atherosclerosis have recently been discussed. While Virchow and Rokitansky observed adventitial inflammation in atherosclerosis, and cellular immune infiltrates were characterised in the early 1960s, a more thorough analysis of this phenomena has only recently occurred. Even in normal arteries, the adventitia appears to be a more complicated area than the intima and media. It is made up of a variety of cell types, including fibroblasts, dendritic cells, monocytes/macrophages, mast cells, and T-cells. It also contains nerve endings, tiny blood arteries (vasa vasorum), endothelial progenitor cells, and other components. Data from atherosclerosis animal models give intriguing insights, indicating the presence of B and T lymphocytes in the adventitia, which produce inflammatory follicle-like structures. Several studies [2] imply that adventitial lymphocytes play a crucial function. Proinflammatory IL-17A-producing T cells, for example, are located in the adventitia, and inhibiting IL-17A has been demonstrated to diminish aortic macrophage accumulation and atherosclerosis. Although immunecompetent lymphocytes, including T cells and B cells, have been found in adventitial lymphoid follicles in both the aorta and coronary arteries, our knowledge of the adventitia’s function in human atherosclerosis remains restricted. In atherosclerotic lesions, an important concern is how the adventitia interacts with the intima. In contrast to their prevalence in the adventitia of atherosclerotic lesions, B cells are not typically seen in the intima. According to research in animal models, the involvement of B cells in atherosclerosis is likely dependent on subsets, with B2 lymphocytes being atherogenic and B1 lymphocytes providing protection. Intimal haemorrhage is another condition that may lead to cardiovascular disease (CVD), plaque rupture, and latestage atherosclerosis. Late-stage lesions include a high concentration of erythrocyte membranes, which can function as proinflammatory agents and increase the likelihood of plaque rupture. Immune modulatory treatment, which targets certain immune responses, might be used to treat atherosclerosis and/or cardiovascular disease (CVD). Targeting epitopes from oxidised low-density lipoprotein (oxLDL) is one example of such treatment. Immunisation with modified forms of LDL was identified in the mid-1990s to ameliorate atherosclerosis, showing the possibility of suppressing atherosclerosis development by immunisation. As previously stated, LDL oxidation produces a variety of chemical components, including fragmented apoB and oxidised phospholipids. One approach is to use apoB-derived peptides with immunomodulatory characteristics to target the apoB component. Another line of study and potential therapy focuses on employing monoclonal antibodies to target the phospholipid component, especially phosphocholine (PC). Cohort studies, animal trials, and in vitro research have all validated this method, demonstrating antiinflammatory benefits, cell death suppression, and decreased oxLDL absorption in macrophages. The delivery of immunoglobulins (Igs) is a less specific way of immunomodulation. Animal trials employing human Ig produced from pooled donors, such as IVIG, have yielded encouraging outcomes.
Discussion
Collectively, atherosclerosis, a chronic inflammatory disorder affecting large and medium-sized arteries, is the leading cause of death and considerable morbidity globally, particularly in industrialised nations. The presence of active immune cells within the walls of damaged arteries emphasises the critical role of inflammation in atherosclerosis. Inflammation is thought to have a substantial role in plaque rupture, the direct cause of CVD. Several ideas have been advanced to explain the underlying causes of atherosclerosis inflammation, including the participation of oxidised or modified forms of LDL, infections, heat shock proteins (HSPs), and non-specific systemic inflammation. Antiinflammatory and immunological modulatory therapies are being investigated in ongoing or prospective investigations. However, the causative involvement of inflammation in atherosclerosis remains a theory until human studies provide evidence of better atherosclerosis outcomes. The artery wall is divided into three different layers. The tunica intima, or initial layer, is lined with endothelial cells that come into direct touch with the circulation. It also contains smooth muscle cells (SMCs) in humans. The second layer, referred to as the media, is made up of SMCs and extracellular matrix. The third layer, known as the adventitia, is the most complicated of the three. Although the adventitia’s specific significance in atherosclerosis is unknown, it contains a variety of cell types, including fibroblasts, dendritic cells, monocytes/macrophages, mast cells, and T-cells. Nerve endings, tiny arteries (vasa vasorum), endothelial progenitor cells, and a matrix are also found in the adventitia.
Conclusion
Several early processes occur during the development of atherosclerosis. The endothelial cell monolayer gets stimulated, causing adhesion molecules to be expressed. Monocytes and macrophages from the blood, dendritic cells, T cells, and some B cells move into the intima. Modified versions of LDL bind to matrix components as well. Monocytes/macrophages proliferate and change into foam cells, which are largely packed with modified LDL. Smooth muscle cells (SMCs) from the media move into the intima and take on a synthetic phenotype, contributing to matrix component formation. A fibrous cap grows to cover the atherosclerotic plaque as it advances. Dying and dead cells amass over time, with many of them originating from foam cells. Microvessels form within the plaque as well. The fracture or rupture of the fibrous cap is a concerning complication of atherosclerosis that might be considered a typical component of ageing. The blood coagulation components are exposed to plaque material, including tissue factor, resulting in thrombosis and ultimately infarction. The precise origin of inflammation and subsequent plaque rupture is unknown, while there are several theories that are not mutually incompatible. It has been discovered that oxidised LDL (oxLDL) activates T cells and stimulates monocytes/macrophages and other cell types within the plaque. Inflammatory phospholipids are most likely involved in this impact. Natural antibodies against phosphocholine (anti-PC) and other phospholipids may have a protective function by reducing inflammation. Reduced levels of these antibodies may have a role in inflammation. Heat shock proteins (HSPs), which are produced in the plaque by stress, oxLDL, and other stimuli, may become immunogenic and stimulate immunological responses that lead to atherosclerosis inflammation. Many infectious agents are present within the lesions, as has been thoroughly addressed. However, the evidence for their possible causal role in atherosclerosis is ambiguous, as they might be unwitting bystanders. Cytokines and chemokines may play an important role as initial triggers of plaque rupture.
Acknowledgement
Not applicable.
Conflict of Interest
Author declares no conflict of interest.
References
- Gimbrone MA Jr, Topper JN, Nagel T, Anderson KR, Garcia-Cardena G (2000) Endothelial dysfunction, hemodynamic forces, and atherogenesis. Ann N Y Acad Sci 902:230-239.
- Campbell KA, Lipinski MJ, Doran AC, Skaflen MD, Fuster V, et al. (2012) Lymphocytes and the adventitial immune response in atherosclerosis. Circ Res 110:889-900.
- Frostegard J, Ulfgren AK, Nyberg P, Hedin U, Swedenborg J, et al. (1999) Cytokine expression in advanced human atherosclerotic plaques: dominance of pro-inflammatory (Th1) and macrophage-stimulating cytokines. Atherosclerosis 145:33-43.
- Libby P, Ridker PM, Hansson GK (2011) Progress and challenges in translating the biology of atherosclerosis. Nature 473:317-325.
- Camejo G, Lalaguna F, Lopez F, Starosta R (1980) Characterization and properties of a lipoprotein-complexing proteoglycan from human aorta. Atherosclerosis 35:307-320.
- Tabas I, Williams KJ, Boren J (2007) Subendothelial lipoprotein retention as the initiating process in atherosclerosis: update and therapeutic implications. Circulation 116:1832-1844.
- Frostegard J, Nilsson J, Haegerstrand A, Hamsten A, Wigzell H, (1990) Oxidized low density lipoprotein induces differentiation and adhesion of human monocytes and the monocytic cell line U937. Proc Natl Acad Sci USA 87:904-908.
- Frostegard J, Wu R, Giscombe R, Holm G, Lefvert AK, et al. (1992) Induction of T-cell activation by oxidized low density lipoprotein. Arterioscler Thromb 12:461-467.
- Berliner JA, Territo MC, Sevanian A, Ramin S, Kim JA, et al. (1990) Minimally modified low density lipoprotein stimulates monocyte endothelial interactions. J Clin Invest 85:1260-1266.
- Elinder LS, Dumitrescu A, Larsson P, Hedin U, Frostegard J, et al. (1997) Expression of phospholipase A2 isoforms in human normal and atherosclerotic arterial wall. Arterioscler Thromb Vasc Biol 17:2257-2263.
- Atout R, Karabina SA, Dollet S, Carreras M, Payre C, et al. (2012) Human group X secreted phospholipase A2 induces dendritic cell maturation through lipoprotein-dependent and -independent mechanisms. Atherosclerosis 222:367-374.
- Huang YH, Schafer-Elinder L, Wu R, Claesson HE, Frostegard J (1999) Lysophosphatidylcholine (LPC) induces proinflammatory cytokines by a platelet-activating factor (PAF) receptor-dependent mechanism. Clin Exp Immunol 116:326-331.
- Goncalves I, Edsfeldt A, Ko NY, Grufman H, Berg K, et al. (2012) Evidence supporting a key role of Lp-PLA2-generated lysophosphatidylcholine in human atherosclerotic plaque inflammation. Arterioscler Thromb Vasc Biol 32:1505-1512.
- Frostegard J, Huang YH, Ronnelid J, Schafer-Elinder L (1997) Platelet-activating factor and oxidized LDL induce immune activation by a common mechanism. Arterioscler Thromb Vasc Biol 17:963-968.
- Watson AD, Leitinger N, Navab M, Faull KF, Horkko S, et al. (1997) Structural identification by mass spectrometry of oxidized phospholipids in minimally oxidized low density lipoprotein that induce monocyte/endothelial interactions and evidence for their presence in vivo. J Biol Chem 272:13597-13607.
- Greig FH, Kennedy S, Spickett CM (2012) Physiological effects of oxidized phospholipids and their cellular signaling mechanisms in inflammation. Free Radic Biol Med 52:266-280.
- Miller YI, Choi SH, Wiesner P, Fang L, Harkewicz R, et al. (2011) Oxidation-specific epitopes are danger-associated molecular patterns recognized by pattern recognition receptors of innate immunity. Circ Res 108:235-248.
- Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, et al. (2004)Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case–control study. Lancet 364:937-952.
- Yanbaeva DG, Dentener MA, Creutzberg EC, Wesseling G, Wouters EF (2007) Systemic effects of smoking. Chest 131:1557-1566.
- Morrow JD, Frei B, Longmire AW, Gaziano JM, Lynch SM, et al. (1995) Increase in circulating products of lipid peroxidation (F2-isoprostanes) in smokers smoking as a cause of oxidative damage. N Engl J Med 332:1198-1203.
- Penn A, Snyder CA (1993) Inhalation of sidestream cigarette smoke accelerates development of arteriosclerotic plaques. Circulation 88:1820-1825.
- Zhu BQ, Sun YP, Sievers RE, Isenberg WM, Glantz SA, et al. (1993) Passive smoking increases experimental atherosclerosis in cholesterol-fed rabbits. J Am Coll Cardiol 21:225-232.
- Gairola CG, Drawdy ML, Block AE, Daugherty A (2001) Sidestream cigarette smoke accelerates atherogenesis in apolipoprotein E−/− mice. Atherosclerosis 156:49-55.
- Kunitomo M, Yamaguchi Y, Kagota S, Yoshikawa N, Nakamura K, et al. (2009) Biochemical evidence of atherosclerosis progression mediated by increased oxidative stress in apolipoprotein E-deficient spontaneously hyperlipidemic mice exposed to chronic cigarette smoke. J Pharmacol Sci 110:354-361.
- Frostegard J (2005) Atherosclerosis in patients with autoimmune disorders. Arterioscler Thromb Vasc Biol 25:1776-1785.
- Dimitriadis E, Griffin M, Owens D, Johnson A, Collins P, et al. (1995)Oxidation of low-density lipoprotein in NIDDM: its relationship to fatty acid composition. Diabetologia 38:1300-1306.
- Beckman JA, Goldfine AB, Gordon MB, Creager MA (2001) Ascorbate restores endothelium-dependent vasodilation impaired by acute hyperglycemia in humans. Circulation 103:1618-1623.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Coppe G (2023) Inflammation and Immunological Responses inAtherosclerosis: Origins and Therapeutic Targets for Innovative CardiovascularDisease (CVD) Therapies. Atheroscler Open Access 8: 211. DOI: 10.4172/asoa.1000211
Copyright: © 2023 Coppe G. This is an open-access article distributed under theterms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 932
- [From(publication date): 0-2023 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 675
- PDF downloads: 257