Inferio-Parotid Transmasssetric Approach for Mandibular Subcondylar Fracture: A Novel Approach
Received: 23-Jan-2023 / Manuscript No. ocr-23-87673 / Editor assigned: 24-Jan-2023 / PreQC No. ocr-23-87673 / Reviewed: 09-Feb-2023 / QC No. ocr-23-87673 / Revised: 13-Feb-2023 / Manuscript No. ocr-23-87673 / Published Date: 23-Feb-2023
Letter to the Editor
Apropos to the article by [1] entitled "Variations in the retromandibular transparotid approach to the condyle-transparotid versus anteroparotid transmassetric- a prospective clinical comparative study," a few clarifications are in order. According to the author, the mandibular condylar processes are one of the most common sites of fracture in mandibular fractures. The condylar fracture accounts for almost 20% to 50% of all maxillofacial fractures due to the thin neck and the location against a strong cranial base condyle, increasing the chances of fracture during load transfer.
There is an inadequacy in this study since the authors stated that the surgical procedure for condylar neck and subcondylar fractures is still debated widely. Open-ended treatment of mandibular condyle fractures relies on accurate diagnosis, appropriate surgical approach, and minimizing severe osteosynthesis and broken condyle, which provides good results and immediate function compared to close reduction. The closed reduction technique has been associated with closed weight loss and dysfunction, leading to complications such as facial nerve damage, mandibular asymmetry, trismus, ankylosis, and malocclusion.
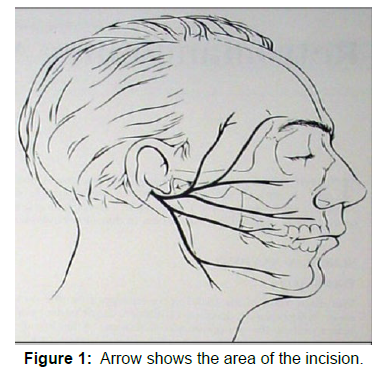
The authors mentioned in their review that extraoral surgical approaches to ORIF include preauricular, submandibular, retromandibular, and transmassetric anteroparotid approaches. Furthermore,the authors reported five cases who were treated with an inferioparotid transmassetric approach, respectively. Using this approach did not result in postoperative infection, haemorrhage, occlusal discrepancy, limited mouth opening, or facial nerve weakness (Figure 1).
The advent of treatments aimed at alleviating joint trauma led Hinds and Girotti to introduce a new technique called retromandibular in 1967, which was later modified by [2] providing access to treat condylar and subcondylar neck fractures and complications such as infection, Frey's syndrome, parotid fistula, and neurological damage.
Therefore, the ongoing review does not represent an effective approach with minimal postoperative complications. In light of this study, insight is gained into a central element of alleviating complications caused by low condylar fractures. Low condylar fractures treated conservatively can cause facial nerve and parotid gland damage [3,4].
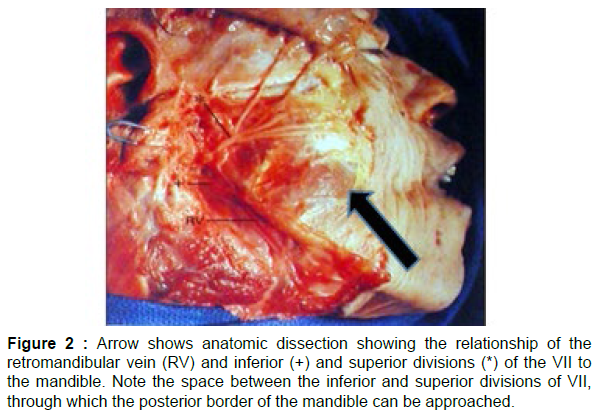
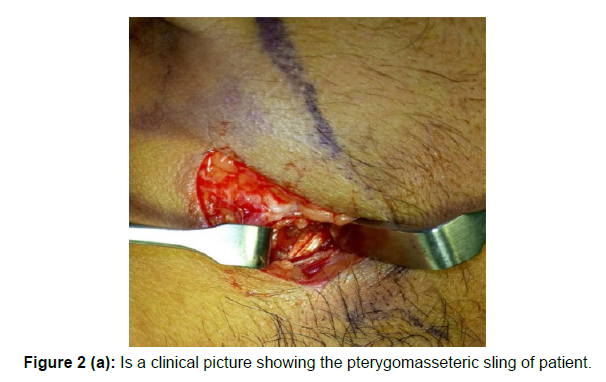
The incision begins 0.5cm below the ear lobe and continues inferiorly 3 to 3.5 cm to the posterior border of the mandible, extending below the mandible angle according to the amount of exposure. The incision is made through the skin and subcutaneous tissue (Figure 2). Subcutaneous dissection is performed above the layer of the SMAS (superficial musculoaponeurotic system). The angle between the mandible and the lower border of the parotid gland is identified. The platysma just below the angle of the mandible or lower border of the parotid gland is subsequently incised. In this procedure, the masseter fascia or muscle is incised [5, 6]. Dissection of the ramus of the mandible is performed subperiosteally so that the condylar process can be exposed (Figure 2 (a)).
Figure 2 : Arrow shows anatomic dissection showing the relationship of the retromandibular vein (RV) and inferior (+) and superior divisions (*) of the VII to the mandible. Note the space between the inferior and superior divisions of VII, through which the posterior border of the mandible can be approached.
It would be pragmatic to consider the above-mentioned prepositions in the review to obtain reliable conclusions regarding alleviating the complications of treating low condylar fractures through an inferioparotid transmassetric approach.
Author contribution
Research concept and design: Dr. Raheel Memon
Collection and assembly of data: Dr. Raheel Memon, Dr. Syeda Adeena Hasan
Data analysis and interpretation: Sidra Zaheer
Writing the article: Dr. Adeena Hasan, Sharjeel Chaudhry
Critical revision of the article: Dr. Shaheen Ahmed, Dr. Abdul Hafeez Sheikh
Declaration of conflicting interests
The author(s) reported no relationship that could be construed as a conflict of interest.
References
- Bhutia O, Kumar L, Jose A, Roychoudhury A, Trikha A (2014) Evaluation of facial nerve following open reduction and internal fixation of subcondylar fracture through retromandibular transparotid approach. Br J Oral Maxillofac Surg 52: 236-240.
- Agostino D, Trevisiol L, Procacci P, Favero V, Odorizzi S, et al. (2017) Is the retromandibular transparotid approach a reliable option for the surgical treatment of condylar fractures?. J Oral Maxillofac Surg 75: 348-356.
- Imai T, Fujita Y, Motoki A, Takaoka H, Kanesaki T, et al. (2019) Surgical approaches for condylar fractures related to facial nerve injury: deep versus superficial dissection. Int J Oral Maxillofac Surg 48: 1227-1234.
- Kanno T, Sukegawa S, Tatsumi H, Karino M, Nariai Y, et al. (2016) Does a retromandibular transparotid approach for the open treatment of condylar fractures result in facial nerve injury?. J Oral Maxillofac Surg 74: 2019-2032.
- Ramaraj P N, Patil V, Singh R, George A, Vijayalakshmi G, et al. (2020) Variations in the retromandibular approach to the condyle-transparotid versus anteroparotid transmasseteric–a prospective clinical comparative study. J Stomatol Oral Maxillofac Surg 121: 14-18.
- Shi D, Patil M, Gupta R (2015) Facial nerve injuries associated with the retromandibular transparotid approach for reduction and fixation of mandibular condyle fractures. J Craniomaxillofac Surg 43: 402-407.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Memon R, Ahmed S, Shaikh AH, Hasan SA, Chaudhry S, et al. (2023) Inferio-Parotid Transmasssetric Approach for Mandibular Subcondylar Fracture: A Novel Approach. Otolaryngol (Sunnyvale) 13: 506.
Copyright: © 2023 Memon R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1542
- [From(publication date): 0-2023 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 1223
- PDF downloads: 319