Induction of Labor and Its Determinant Factors: Retrospective Cross-Sectional Study from a Public Hospital in Ethiopia
Received: 19-Aug-2018 / Accepted Date: 11-Sep-2018 / Published Date: 18-Sep-2018 DOI: 10.4172/2376-127X.1000388
Keywords: Induction of labor; Oxytocin; Misoprostol
Abbreviations
ANC: Ante Natal Care; AOR: Adjusted Odd Ratio; CI: Confidence Interval; COR: Crude Odd Ratio; EPI-INFO: Epidemiological Information Software; OR: Odd Ratio; PROM: Premature Rupture of Membrane; SD: Standard Deviation; SPSS: Statistical Package for Social Science; WHO: World Health Organization
Introduction
Induction of labor is an obstetrical procedure which is done to help mothers give birth vaginally after viability of the fetus (after 28 weeks of gestation in Ethiopia context). Induction of labor done mainly to reduce the risk of still birth, intrauterine fetal death, rate of cesarean section and infection but sometimes it leads to poor maternal and neonatal outcomes.
Multiple pharmacological, non-pharmacological, mechanical and complementary methods are available to do this procedure.
There are different factors which determine the magnitude of induction of labor. So, we are carrying out retrospective chart review to look all determinants routinely mentioned in patients chart. We included 384 mothers chart in the review. Four variables were identified and significantly associated with induction of labor. These were antenatal care follow up at private clinic, hypertension disorder during pregnancy, premature rupture of pregnancy and fetal structural anomalies.
Approximately four million fetuses annually are still born after the age of viability, similarly more than 500 women death as a result of birth. Majority of these deaths occur in poor resources setting countries. The prevention of these maternal and neonatal deaths sometimes requires the prompt and early delivery after the age of viability but before the onset of labor through induction of labor [1].
Induction of labor is one of the most common procedure in obstetrics and one of the fastest growing procedures in the world mainly in developed countries. The reason why it rises is unclear but there are some assumptions, like a growing use of labor induction for post term pregnancies, an increasing trend towards elective induction of labor and induction with mothers’ request [2].
The risks associated with induction of labor include uterine hyper stimulation, increased rates of operative deliveries and caesarean sections, fetal heart rate pattern abnormalities, premature deliveries, infections in some cases and in the worst scenario may result uterine rupture [3]. Higher need of postpartum uterotonic drugs, nearly threefold risk of admission to intensive care unit, fivefold risk of postpartum hysterectomy and increase need of anesthesia/analgesia are also some of maternal adverse events [4]. Some countries like; United States of America encourage to hold annual training session/meeting and having induction guideline to provide information for clinicians regarding admitting privilege and to have well stated indication for induction [5]. Due its complication induction of labor should be done with tangible reasons, use proper medications and it needs close follow up [6].
Induction of labor may be less efficient and having more strain on labor wards than spontaneous labor, but has advantages like, reduce risk of intrauterine fetal death, stillbirth, sepsis and need of cesarean section [7].
Currently the rate of induction of labor increased in United States of America, due to the expanding and utilization of ultrasound which help to early identify intrauterine fetal death, intrauterine growth restriction and also help to estimate gestational age [8].
The incidence of induction of labor is ranging from approximately 6% in 3rd world countries and 20% in developed countries. More than 70% of women would prefer not to have induction of labor by any means [9,10].
Vaginal misoprostol compared with other methods of induction of labor, resulted with higher rate of tachsystole and lower rate of postpartum hemorrhage but, no significant different in mode of delivery, maternal and neonatal outcomes [11]. The average rates of induction of labor in African and Asian countries were 4.4% and 12.1% respectively [12].
African countries had lower rates of labor induction (lowest, Niger 1.4%) compared with Asian countries (highest, Srilanka 35.5%) [13]. The study conducted in Latin America showed that the average induction of labor was 11.4% (lower, 5.1% in Peru and higher, 20.1% in Cuba). Whereas the factors like: Age ≥ 35years, being unmarried, Parity, PROM, hypertension during pregnancy and number of ANC visit ≥ 4 were significantly associated to the rate of induction of labor [14].
In Australia the induction rate in nulliparous was 12.5%, United Kingdom (32.3%) and Germany (23%) among both multi and nulliparous mothers [15-17]. Institutional based cross sectional chart review study conducted in United Kingdom revealed that, distance from the health care facility (comes from rural), prolonged pregnancy, PROM, poly/oligohydramnios, ante partum hemorrhage, previous still birth and primipara have been associated with induction of labor [16].
In Nigeria, the magnitude of induction of labor was 6.5% and in D.R. Congo which was 3.2% [18,19]. There research conducted in Ethiopia, Addis Ababa two teaching hospitals (Gandhi and St. pauls) magnitude of induction of labor was 4% [20].
Induction of labor is an important practice that is carrying out in modern obstetrics, and very vital to decrease maternal and perinatal morbidity and mortality. On the other hand, it might have potential harm and increasing costs for national health services and again it may also lead to poor maternal and neonatal outcomes. But, the knowledge on determinants and magnitude of labor induction may be a useful tool for monitoring the frequency and place of induction, as well as whether it is being overused or underused.
Therefore, this finding will helps for clinicians work to minimize or avoid those preventable factors and conditions which increase the frequency of induction of labor and wake up call to do further survey in national level.
Materials and Methods
Study area and period
This study was carried out at Lemlem Karl Hospital which is a general hospital in Miachew town, Tigray regional state, Ethiopia form August 1 to 30, 2016. This hospital located within the town of Maichew 127 km far from Mekelle, the capital of Tigray regional state and 665 km north of Addis Ababa. According to 2007 Census conducted by the Central Statistical Agency of Ethiopia report, this town had a total population of 23,419, of whom 11,024 were males and 12,395 were females. There are a total of eight health intuitions in the town; two governmental health centers, five private clinics and one general hospital. Lemlem Karl Hospital was one of the awarded hospital in 2016 in national level with their remarkable documentation, client satisfaction and clean and safe environment. At this hospital, 1189 clients gave birth per year and among these births 357 were by cesarean section. The obstetrics and Gynecology department had 31 beds and the department served by 9 midwifes (4 degree and 5 diploma holders), one Obstetrician and one master holder in integrated obstetrics and surgery.
Study design
Hospital based cross sectional study design was conducted using retrospective chart review.
Source population
All charts of women who gave birth at Lemlem Karl hospital.
Study population
Charts of women who gave birth at Lemlem Karl Hospital from July 30, 2015 to July 30, 2016 and selected systematically.
Sampling technique
Systematic sampling technique.
Sample size determination
The sample size was calculated by using single population proportion formula. The following assumptions were considered: 50% prevalence was taken since no local data, Z: The standard score corresponding to a 95% confidence interval, a: The risk of rejecting the null hypothesis (0.05) and d: Margin of error (5%). Finally the required sample size became 384.
Sampling procedure
There were a total 1189 mothers who gave birth over one year at Lemlem Karl hospital from July 30, 2015 to July 30, 2016. Among them by using, systematic sampling technique in every three interval 384 study participants’ charts were identified and traced using their medical recording number.
Data collection instruments and procedure
Checklists or formats prepared in English after reviewing different studies related to this topic and used as data extraction instrument. All the variables of interest list down in the chart were assessed accordingly. Three individuals (two diploma holders and one Bachelor science in Midwifery profession) and one supervisor involved in data extraction process and supervision respectively. Training was given to the data abstractors and supervisor. Finally data abstractors traced and extracted data from systematically identified charts of mothers who gave the most recent birth within one year prior to the study period.
Data quality control
High quality data abstractor involved and intensive discussion was conducted on the purpose of the study, contents of checklists and how extracts data. Supervisor was monitoring the study progress and hold periodic meeting. Completeness, accuracy and consistency of data recording were cross checked on daily basis.
Data processing and analyzing
The data were computerized using EPI-info version 7.0 and transported to SPSS version 20 for analysis. Descriptive statistics (both frequency tables and graphs) were used to describe study variables. Bivariate logistic regression analysis was used to identify factors associated with induction of labor. Independent variables significant in the bivariate analysis were then, entered into multivariate logistic analysis. The association were estimated by Odds Ratio (OR) and 95% Confidence Interval (CI). The differences were deemed significant when P<0.05.
Eligibility criteria
Inclusion criteria: All registered charts of women who gave birth at Lemlem Karl hospital from July 30, 2015 to July 30, 2016.
Results
Socio demographic characteristics of women who gave birth at Lemlem Karl hospital from 2015-2016
A total 384 mothers’ chart extracted in this study. The mean (± SD) of the mothers’ age was 26 (± 5) years. The maximum and minimum age in years was 44 and 16. Majority 334 (87%) were in the age group of 20 to 34 years which was followed by 31(8.1%) participants age were ≥ 35 years and 19 (4.9%) of the them were ≤ 19 years old. Most of the study participants 365 (95.1%) were married and 9 (2.3%), 6 (1.6%) and 4 (1%) were divorce, single and widowed respectively. More than half 227 (59.1%) of the study mothers were from urban and the remaining 157 (40.9%) of them residence were rural.
Obstetrical factors and complications during pregnancy of women who gave birth at Lemlem Karl Hospital from 2015-2016
More than half (52.1%) were multipara. Two hundred five (53.4%) of the study participants had a total four times ANC visits at the time of chart reviewing in the most recent pregnancy followed by: 116 (30.2%) three, 27 (7%) two, 22 (5.7%)five and 10 (2.6%) six times. The mean (± SD) of gestational age was 39+2 (± 1+4) weeks. Almost all mothers (93.5%) were term pregnancy at the time of delivery. Nearly three fourth 283 (73.7%) of study participants gestational age was confirmed by using their last normal menstrual period. Of the total participants, 19 (4.9%) and 10 (2.6%) were developed ante partum hemorrhage and intrauterine fetal death type of complications during the most recent pregnancy respectively (Table 1).
| Variables(n=384) | Frequency | Percentage | |
|---|---|---|---|
| Parity | Primipara | 200 | 52.10% |
| Multipara | 184 | 47.90% | |
| Institution of ANC visit | Health Center | 197 | 51.30% |
| Hospital | 140 | 36.50% | |
| Private Clinic/hospital | 47 | 12.20% | |
| Number of ANC visits | 1-3 visits | 147 | 38.30% |
| ≥ 4 visits | 237 | 61.70% | |
| Gestational age | ≤ 258 days | 12 | 3.10% |
| 259-293 days | 359 | 93.50% | |
| ≥ 294 days | 13 | 3.40% | |
| GA confirmed | By U/S | 52 | 13.50% |
| LNMP | 283 | 73.70% | |
| Both | 49 | 12.80% | |
| PROM | No | 351 | 91.40% |
| Yes | 33 | 8.60% | |
| PIH | No | 360 | 93.80% |
| Yes | 24 | 6.20% | |
| Fetal anomaly | No | 358 | 93.20% |
| Yes | 26 | 6.80% | |
| Other medical illness (renal, | No | 383 | 99.70% |
| Cardiac and GDM) | Yes | 1 | 0.30% |
| Amniotic fluid disorder | No | 377 | 98.20% |
| Yes | 7 | 1.80% | |
| Previous still birth | No | 381 | 99.20% |
| Yes | 3 | 0.80% | |
Table 1: Shows obstetrical factors and complications during pregnancy of women who gave birth from July 30, 2015 to July 30, 2016 at Lemlem Karl Hospital (n=384); ANC: Antenatal Care, GA: Gestational Age, PROM: Premature Rupture of Membrane, PIH: Pregnancy Induced Hypertension, GDM: Gestational Diabetic Mellitus, U/S: Ultrasound and LNMP: Last Normal Menstrual Period
Magnitude of induction of labor and other related conditions of the women who gave birth at Lemlem Karl Hospital from 2015-2016
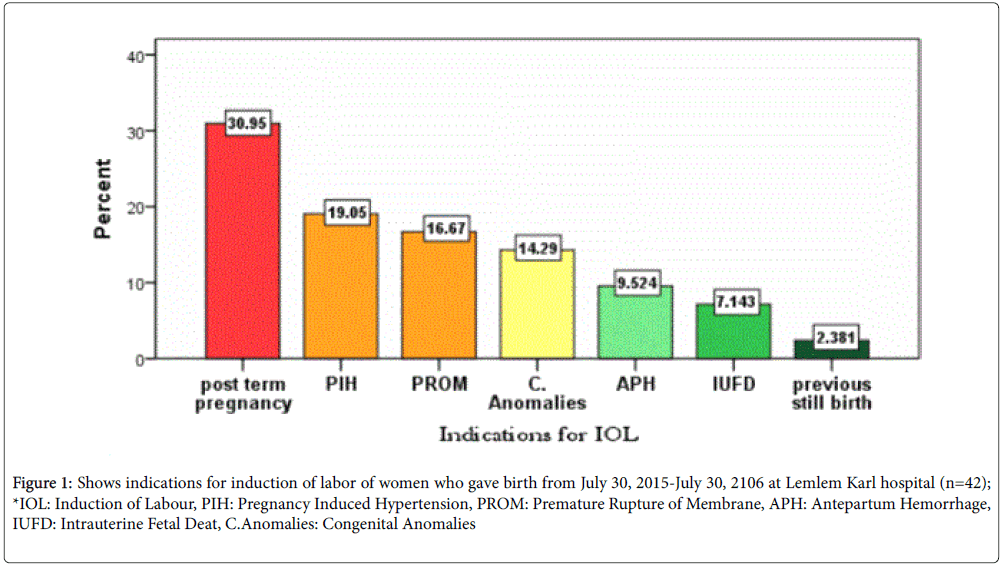
Majority 342 (89.1%) of the mothers labor were initiated spontaneously and the remaining 42 (10.9) were by induction. From the indications of induction of labor, Post term pregnancy was the commonest 13 (31%). Regarding to the method of induction more than half 25 (59.5%) of them were induced by misoprostol (prostaglandin E1) alone and 11 (26.2%) were with both misoprostol and Pitocin intravenous. Among mothers who were induced by misoprostol alone, all of them received through vagina. Of 42 induced study participants 31 (73.8%) of them gave birth via vaginally and 11 (26.2%) by caesarean section. The indications for caesarean section were failed induction and non-reassuring fetal heart beat pattern, each accounts 5 (45.5%) and the remaining were cephallo-pelvic disproportion. The mean (± SD) time interval from induction to delivery was 15 (± 6) h (Figure 1).
Figure 1: Shows indications for induction of labor of women who gave birth from July 30, 2015-July 30, 2106 at Lemlem Karl hospital (n=42); *IOL: Induction of Labour, PIH: Pregnancy Induced Hypertension, PROM: Premature Rupture of Membrane, APH: Antepartum Hemorrhage, IUFD: Intrauterine Fetal Deat, C.Anomalies: Congenital Anomalies
Determinant factors with the induction of labor
During bivariate analysis a total of eight variables showed significant association to the induction of labour and have been taken in multiple logistic regression with P value of ≤ 0.05. Those were; residence, place (institution) of antenatal follow up, parity, gestational age of the pregnancy, the presence of premature rupture of membrane, intrauterine fetal demise, pregnancy induced hypertension and fetal anomaly. However, in multivariate logistic analysis institution of antenatal care visit, premature rupture of membrane, pregnancy induced hypertension and fetal anomalies were significantly associated with P value of Table 2).
| Variables(n=384) | Induction of labour | ||||
|---|---|---|---|---|---|
| (Frequency & %) | COR(95%CI) | AOR (95% CI) | |||
| No | Yes | ||||
| Residence | Urban | 190 (83.7%) | 37 (16.3%) | 1 | - |
| Rural | 152 (85%) | 5 (3.2%) | 0.169 [0.65-0.44] | 0.173 [0.05-1.57] | |
| Parity | Multipara | 172 (93.5%) | 12 (6.5%) | 1 | - |
| Primipara | 170 (85%) | 30 (15%) | 2.529 [1.253-5.105] | 1.903 [0.749-4.837] | |
| Place of ANC visits | H. Center | 179 (90.9%) | 18 (9.1%) | 1 | - |
| Hospital | 132 (94.3%) | 8 (5.7%) | 0.603 [0.254-1.428] | - | |
| P. Clinic | 31 (66%) | 16 (34.0%) | 5.13 [2.367-11.13] | 3.856 [1.29-11.50]* | |
| GA | ≤ 258 days | 3 (25%) | 9 (75%) | 1 | - |
| 259-293 | 336 (93.6%) | 23 (6.4%) | 0.023 [.006-.090] | 0.027 [.005-1.149] | |
| ≥ 294 day | 3 (23.1%) | 10 (76.9%) | 1.11 [.177-6.970] | - | |
| PROM | No | 317 (90.3%) | 34 (9.7%) | 1 | - |
| Yes | 25 (75.8%) | 8 (24.2%) | 2.984 [1.248-7.130] | 3.57 [1.185-10.76]* | |
| PIH | No | 325 (90.3%) | 35 (9.7%) | 1 | |
| Yes | 17 (70.8%) | 7 (29.2%) | 3.824 [1.484-9.86] | 5.033 [1.44-17.62]* | |
| Fetal anomaly | No | 324 (90.5%) | 34 (9.5%) | 1 | |
| Yes | 18 (69.2%) | 8 (30.8%) | 4.235 [1.714-10.47] | 5.7 [1.614-20.12]* | |
| IUFD | No | 336 (89.8%) | 38 (10.2%) | 1 | |
| Yes | 6 (60.0%) | 4 (40.0%) | 5.895 [1.59-21.82] | 4.85 [0.427-55.178] | |
Table 2: Shows determinant factors to induction of labor among women who gave birth from July 30, 2015 to July 30,2016 at Lemlem Karl General Hospital (n=384); *Variables significantly associated with induction of labor (P<0.05), ANC: Antenatal Care; GA: Gestational Age; PROM: Premature Rupture of Membrane; PIH: Pregnancy Induced Hypertension; IUFD: Intra Uterine Fetal Death
Discussion
Induction of labour is one of the fastest growing medical procedures in current obstetric practice. Generally, there were conflicting results. In this study the magnitude of induction of labor was 10.9%. This finding was almost similar with the survey done by world health organization from 24 selected Asian, African and Latin American countries 9.6%, the survey done in selected six South American countries 11.4% and the study conducted in Nigeria which was 11.5 % [13,14,21].
The magnitude of induction of labor in this study was much higher than the research done in selected African countries by WHO (4.4%), Democratic Republic of Congo (3.2%) and Addis Ababa (4%) [12,19,20]. This much discrepancy could be due to, in Addis Ababa the study participants were only term and post term mothers and method of induction was only oxytocin. In Democratic Republic of Congo study participants were women gave birth only at term and in selected African countries, it might be cumulative effects and instead they have used other alternative like, Cesarean Section.
On the other hand this magnitude was much lesser than the study conducted in United Kingdom which was 32.3% and in Germany (23%) [16,17]. This difference might be due to induction with patients’ request is common in developed countries and they are good in utilization of intrauterine monitoring device and early ultrasound scanning is routine activities to terminate congenital fetuses as the form of abortion.
Institution of ANC follow up was identified to be an independent risk factor f or induction of labor in this study. Mothers who had antenatal follow up at private clinic were 3.9 times more likely to be induced [AOR=3.856, 95% CI (1.293-11.499)]. It was supported with the survey done in South America, mothers who had ANC follow up at socially secured institution were 20% more likely to get induction of labour compare to mothers who had at public health facilities [14].
This study also noted that mothers admitted with the diagnosis premature rupture of membrane were 3.6 times more likely to had induction of labour [AOR=3.571, 95% CI (1.185.10.759)]. It was almost the same value the study done in United Kingdom and the survey done in Latin America [14,16].
Women admitted with the diagnosis of pregnancy induced hypertension were 5 times more likely to had induction of labour [AOR=5.033, 95% CI (1.438-17.62)]. It was low but supported with the study done in Latin America and United Kingdom [14,16].
Fetal structural condition was matters for induction of labor in this study. Mothers who pregnant anomalic fetuses were 5.7 times more likely to get induction of labor [AOR=5.698, 95% CI (1.614-20.116)]. It was not significantly associated in other researches. This may be due to wide use of sophisticated imaging modalities and biochemical laboratories to diagnosis and terminate early the pregnancies as the form of abortion.
Limitation of the study
This finding is vital, considering the scarcity of data in obstetrical procedures in the country level. However, there was one main limitationSince, the source of data was patient records allowing only to use available variables but further factors were remained untested. Like, body mass index, urinary tract infection, Depression, educational level etc.
Conclusion and Recommendations
The magnitude of induction of labor was a bit high than other previous studies conducted from different region of Africa and the average African induction of labor rate stated by WHO. Independent Factors like, premature rupture of membrane, pregnancy induced hypertension, fetal anomaly and place of antenatal care follow-up were found to have statistically significant association with induction of labor. Therefore, improving the quality of antenatal care and prepare induction guidelines which works for both governmental and private health care and do surveillance in national level have to be considered to reduce the rate of unnecessary induction of labor.
Declarations
Ethical approval and consent to participants
Written ethical approval was obtained from Mekelle University, College of Health Science of Institutional Ethical Review Board (ref. no: ECR 0786/2016). Permission was obtained from Lemlem Karl Hospital officials after discussing the objective of the study. Personal patient information used for only study purpose (individuals persons detail data, image or videos not used). After taking necessary data from patients’ chart, the charts had given back to the card room.
Availability of data and materials
The data which helped to get these findings are available but it is not one hundred percent open because there are some sensitive issues. The data are available from the corresponding authors upon reasonable request.
Authors’ contributions
BK was the study coordinator and involved in the study design, analysis, report and manuscript writing. BD and AB were participated in section of manuscript, analysis and report writing. YM, ZM and AY were also involved in the data collection, processing, carried out statistical analysis and helped to draft the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We would like to express our deepest thank to Mekelle University for funding to conduct this study. Mekelle University provided fund for data collectors. Next, our gratitude goes to Lemlem Karl hospital staffs for their willingness and support to access the data.
References
- Ade-Ojo IP, Akintayo AA (2013) Induction of labour in the developing countries-an overview. J Med Med Sci 4: 258-262 .
- Sanchez-Ramos L (2005) Induction of labour . Obstet Gynecol Clin North Am 32: 181-200.
- Hurissa BF, Geta M, Belachew T (2015) Prevalence of failed induction of labor and associated factors among women delivered in hawassa public health facilities, Ethiopia. J Womens Health Care 4: 253.
- Guerra GV, Cecatti JG, Souza JP, Faúndes A, Morais SS, et al. (2011) Elective induction versus spontaneous labour in Latin America . Bull World Health Organ 89: 657-665.
- APHA (2014) Reducing non medically indicated elective induction of labor.
- Fourth Edition of the ALARM International Program (2006) Induction of labour.
- American College of Obstetricians and Gynecologists (2009) ACOG practice bulletin on induction of labor.
- McCarthy FP, Kenny LC (2013) Induction of labour. Obstet Gynaecol Reprod Med 24 : 9-15.
- Tang J, Kapp N, Dragoman M, De-Souza JP (2013) WHO recommendations for misoprostol use for obstetric and gynecologic indications . Int J Gynaecol Obstet 121: 186-189.
- Crane JM, Young DC (2003) Induction of labour with a favourable cervixand/or pre-labour rupture of membranes Best Pract Res Clin Obstet Gynaecol 17: 795-809.
- Vogel JP, Souza JP, Gülmezoglu AM (2013) Patterns and outcomes of induction of labour in africa and asia: A secondary analysis of the WHO global survey on maternal and neonatal health. PLoS One.
- Guerra G, Cecatti J, Souza J, Faundes A, Morais S, et al. (2009) Factors and outcomes associated with the induction of labour in Latin America. BJOG 116: 1762-1772.
- Patterson JA, Roberts CL, Ford JB, Morris JM (2011) Trends and outcomes of induction of labour among nullipara at term. Aust N Z J Obstet Gynaecol 51: 510-517.
- Humphrey T, Tucker JS (2009) Rising rates of obstetric interventions: Exploring the determinants of induction of labour. J Public Health 31: 88-94.
- Rossi AC, Prefumo F (2015) Pregnancy outcomes of induced labor in women with previous cesarean section: A systematic review and meta-analysis Arch Gynecol Obstet. 291: 273-280.
- Ayuba II, Obilahi-Abhulimen, Ekine AA (2012) The safety of induction of labour in the niger delta region, Nigeria. Greener J Med Sci 2: 173-178 .
- Tandu-Umba B, Tshibangu R, Muela A (2013) Maternal and perinatal outcomes of induction of labor at term in the university clinics of Kinshasa, DR Congo. Open J Obstet Gynecol 3: 154-157.
- Berhan Y, Dwivedi AD (2007) Currentely used oxytocin regimen outcomemeasures at termand post term I: Outcome indicators in relation to parity and indication for induction.Ethiop Med J 45: 235-242.
- Lawani OL, Onyebuchi AK, Iyoke CA, Okafo CN, Ajah LO (2014) Obstetric outcome and significance of labour induction in a health resource poor setting. Obstet Gynecol Int J.
Citation: Rade BK, Mitku YM, Weldemicheal AB, Zenebe ZM, Desalegn AY, et al. (2018) Induction of Labor and Its Determinant Factors: Retrospective Cross-Sectional Study from a Public Hospital in Ethiopia. J Preg Child Health 5: 388. DOI: 10.4172/2376-127X.1000388
Copyright: © 2018 Rade BK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5254
- [From(publication date): 0-2018 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 4263
- PDF downloads: 991