Induction of Labor and Factors Associated with its Outcome in Ethiopia A Systemic Review and Meta-Analysis
Received: 27-Dec-2021 / Manuscript No. jpch-21-50674 / Editor assigned: 29-Dec-2021 / PreQC No. jpch-21-50674(PQ) / Reviewed: 10-Jan-2022 / QC No. jpch- 21-50674 / Revised: 14-Jan-2022 / Manuscript No. jpch-21-50674(R) / Accepted Date: 17-Jan-2022 / Published Date: 17-Jan-2022 DOI: 10.4172/2376-127X.1000509
Abstract
Background: Induction of labor is one of the most common procedures to prevent adverse birth out comes of mother and the newborn yet if not performed under clear indication; it may result in devastating effects. Therefore, this systematic review and meta-analysis aimed to assess the prevalence of Induction of labor and factors associated with its outcome among pregnant women in Ethiopia.
Methods: The data bases used were: PUBMED, Google Scholar, HINARI, EMBASE, African Online Journals and on line repositories. This meta- analysis used twelve observational studies (cross-sectional and case control) which included 7401 participants. Different searching terms were applied based on the adapted PICO principles to achieve and access all the essential articles. Subgroup and sensitivity analysis were conducted with the evidence of heterogeneity. Egger test with funnel plot were used to investigate publication bias. The data were entered and analyzed using Microsoft Excel and Stata11 software respectively.
Results: Twelve studies were included in this systematic review and meta-analysis. The overall pooled prevalence of IOL was 16.43% (95% CI; 9.2, 23.67) in Ethiopia. Gestational age < 42 weeks (AOR: 4.3) and Bishop score > 5 (AOR:5) were associated with successful induction of labor while Nulliparity (AOR:2.9), Gestational age > 42 weeks (AOR:4.5) and Unfavorable Bishop score (AOR 5.2) showed significant association with failed induction.
Conclusion: Gestational age < 42 weeks and Bishop Score > 5 was associated with success of induction of labor while Nulliparity, Gestational age > 42 weeks and Unfavorable Bishop score showed significant association with failed induction. This finding is important to design strategic policies and to prevent emergency neonatal and women complications during the childbirth and postpartum periods.
Keywords: Induction of labor; Successful induction; Failed induction; Pregnant women; Systematic review; Meta-analysis; Ethiopia
Keywords
Induction of labor; Successful induction; Failed induction; Pregnant women; Systematic review; Meta-analysis; Ethiopia
Abbreviations
CI: Confidence Interval
GC: Gregorian Canader
IOL: Induction of Labor
OR: Odd Ratio
WHO: World Health Organization
Introduction
Induction of Labor (IOL) is defined as the process of artificially stimulating the uterus to start labor. It is usually performed by administering oxytocin/prostaglandins or by manually rupturing the amniotic membranes [1]. IOL is one component of the comprehensive obstetrics care services aimed to decrease the risk of maternal and neonatal morbidity and mortality by ending the pregnancy in presence of many obstetrics and medical conditions [2]. IOL is one of the most common procedure in obstetrics and now a days it is one of the fastest growing procedures in the world specially in developed countries compared to the developing ones however its complications are still observed in countries like Ethiopia [3].
IOL may be indicated by medical or obstetrical complications of pregnancy or may be requested or chosen for non-medical or social reasons [4]. Some of the indications include post term pregnancy, hypertensive diseases of pregnancy, premature rupture of membrane, abruptio placentae, chorioamnionitis, fetal demise, Premature Rupture of Membranes (PROM), maternal medical conditions like diabetes mellitus, renal disease, chronic pulmonary disease, chronic hypertension and fetal compromise as severe fetal growth restriction, iso-immunization [5]. IOL carries various risks including failed induction, low heart rate, infection, uterine rupture and bleeding after delivery [6].
Prevalence of IOL varied widely across the world. In United States of America it was 24.5% and from 6.8 to 33% in Europe but in Nigeria 6.5%, in D.R. Congo it was 3.2%, in Tanzania it was 21.63% and in Ethiopia, Addis Ababa it was 4% [7-12].
The outcome of labor induction will be either success or failure. The Bishop score at onset of induction parity of the woman, the indication for the induction and other factors manly affect the success [3, 13]. On the contrary many factors lead to failed induction such as initial poor cervical Bishop's score at induction, fetal macrosomia, high body mass index and advanced maternal age [9-11]. When induction fails to end up in vaginal delivery increased rate of operative vaginal delivery, Caesarean birth, excessive uterine activity, abnormal fetal heart rate patterns, uterine rupture, maternal water intoxication, and possibly cord prolapse are expected as its complication [10, 14].
Induction of labor is carried out in approximately 20% of pregnancies. It has been strongly associated with poor maternal and perinatal outcomes and Ethiopia, as most sub-Saharan countries, experience high maternal and perinatal mortality [11, 15] where some can be related to intra partum interventions as IOL. In areas with a high rate of maternal mortality and morbidity due to poor access to comprehensive emergency obstetric care, knowing the prevalence and factors commonly showing association with its outcome following IOL is crucial. Therefore, this systematic review aimed to estimate the pooled prevalence of induction of labor and associated factors of its outcome in Ethiopia.
Methods
Search strategy
A systemic review and meta-analysis were conducted using the published and unpublished studies to estimate the pooled prevalence of induction of labor and its associated factors in Ethiopia following preferred finding items for systematic reviews and meta-analysis guideline [16-20]. The databases used were; PubMed, HINARI, EMBASE, Google Scholar and African Journals Online. Prevalence of induction of labor OR induction of labor OR labor induction OR outcome of induction of labor OR associated factors of induction of labor AND Ethiopia and related search were used. Searching terms were based on adapted PICO principles to search through the above listed databases to access all the essential articles. The last date of searching was October 18, 2020.
Eligibility criteria
This review included articles which were presented in all forms of observational study design that are reported in English language focused on induction off labor and factors associated with its outcome. Studies without full text and abstract, commentaries, letters, anonymous reports, and editorials than the English were excluded [21].
Data extraction and quality assessment
After the search was conducted, data were extracted using a prepiloted data extraction form developed by the authors. It included the name of the author, year of the study, the region in the country, study design, sample size, and overall prevalence. The first author conducted the primary data extraction and then second and third authors examined the data independently. All of the included articles scored (NOS) 7 and more can be considered a “good” study and have low risk of bias for cross-sectional studies and 9 or more scores for case control and cohort chosen to indicate a high standard for comparative observational studies.
Outcome of measurement
The magnitude of Induction of labor was the primary outcome of the study where-as factors associated with its out-come (successful or failed) was secondary out-come. The odds ratio was calculated for the common risk factors of the reported studies. The most common associated factors included in this systematic review and metaanalysis were gestational age < 42 weeks and favorable bishop score for successful induction whereas nulliparity, unfavorable bishop score and gestational age > 42 for failed induction. Successful induction of labor means when a woman had achieved vaginal birth within 12 hr. after induction of labour was started. A failed induction is failure to achieve a vaginal delivery within 12 hr. after induction of labour was commenced.
Statistical analysis
The extracted data were entered into the excel sheet and imported to STATA 11 for analysis. Heterogeneity among reported prevalence was assessed by using the inverse variance (I2) with Cochran Q statistic of 25%, 50% and 75% as low, moderate and considerable heterogeneity respectively with a p-value less than 0.05 (Rücker, Schwarzer, Carpenter, & Schumacher, 2008). The forest plot was also used to visualize the presence of heterogeneity. Possible variations between studies were evaluated by subgroup analyses and meta-regression. Findings were explained using forest plot with respective odds ratio and 95% confidence intervals. For the second outcomes, pooled odds ratios with 95% CI for each determinant was used to determine the association between induction of labor and its factors [22].
Results
Study selection
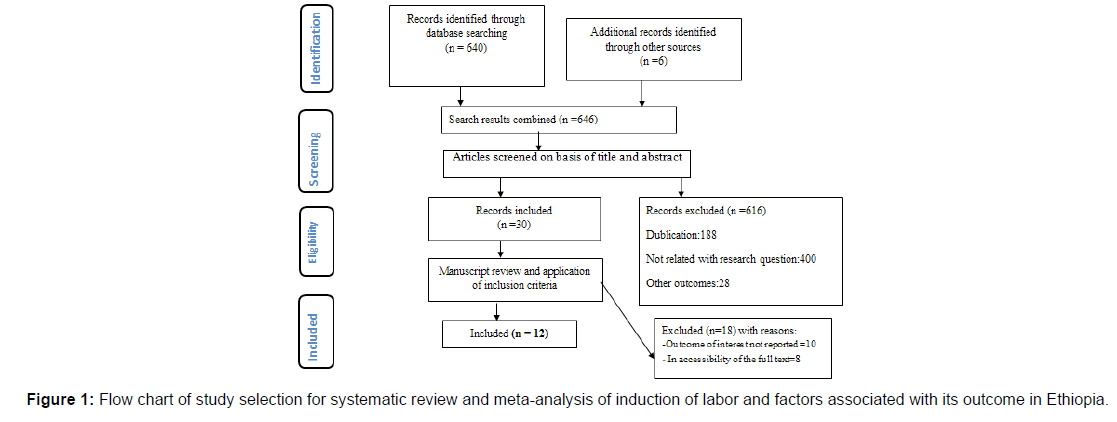
This review included published articles on induction of labor and its outcomes among women in Ethiopia. The electronic search was conducted on several databases, which include; PUBMED, Google Scholar, HINARI, EMBASE, African Online Journals and online repositories. The review found a total of 646 published articles. From this, 316 duplicate records were removed and 300 records were excluded after screening by title and abstracts [23]. A total of 30 full- text articles were screened for eligibility. From this, 18 were excluded based on the exclusion criteria, stated below. Finally, 12 studies were included in the final quantitative meta-analysis (Figure 1).
Characteristics of the included studies
This systematic review and Meta-analysis consist of 10 crosssectional and 2 case-control studies with a total of 7401 participants in different regions in Ethiopia (Table 1).
| Authors | Year of publication | Study region | Study design | Sample size | P (%) of failed induction | P (%) of successful induction |
|---|---|---|---|---|---|---|
| Sara Hiluf | Online | Addis Ababa | cross-sectional | 347 | 40.30 | 59.70 |
| Mulugeta Wodaje | Online | Amhara | cross-sectional | 365 | 9.04 | 15.34 |
| Eyasu M | 2020 | Addis Ababa | cross-sectional | 339 | 25.40 | 74.60 |
| Abenezer M | Preprint | Amhara | case-control | 336 | ---- | |
| Tenagnework D | 2019 | Amhara | cross-sectional | 319 | 19.70 | 53.30 |
| Bekana F | 2015 | SNNPR | cross-sectional | 294 | 17.30 | 72.70 |
| Woubishet G | 2016 | Oromia | cross-sectional | 280 | 21.40 | 65.70 |
| Garang D | 2020 | Tigray | cross-sectional | 3834 | 0.88 | 6.68 |
| EyasuT | 2018 | SNNPR | cross-sectional | 347 | 26.50 | 59.70 |
| Abdulkadir Y | 2017 | Oromia | cross-sectional | 340 | 9.40 | 12.94 |
| Bayew K | 2018 | Tigray | cross-sectional | 384 | --- | |
| Melese G | 2020 | Oromia | comparative cross-sectional | 216 | 38.10 | 61.10 |
Table 1: Study characteristics included in this systematic review and meta-analysis of induction of labor and its outcome in Ethiopia (n=12).
Pooled prevalence of induction of labor in Ethiopia
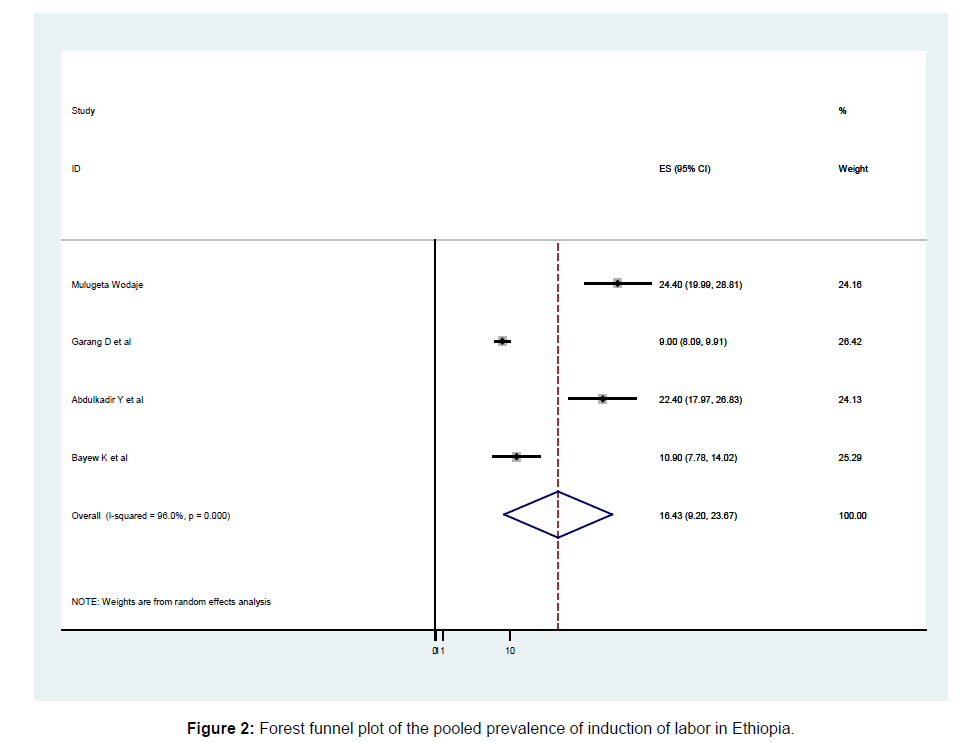
The overall pooled prevalence of this systematic review and metaanalysis of induction of labor in Ethiopia was 16.43% (95% CI; 9.2, 23.67; I2=96.0, P ≤ 0.001) presented with a forest plot (Figure 2).
Outcomes of Induction of labor in Ethiopia
The two main outcomes of induction of labor, falied and successful induction of labor, are presented below. The overall pooled prevalence of failed and successful induction of labor in Ethiopia was 20.65% and 48.12% respectively (Table 2).
| Outcomes of induction | Pooled P (95%CI) | No. of studies | I2 (%) | P-value |
|---|---|---|---|---|
| Failed | 20.65 | 10 | 98.9 | ≤ 0.001 |
| Success | 48.12 | 10 | 99.7 | ≤ 0.001 |
Table 2: Summary of failed and successful induction of labor in Ethiopia.
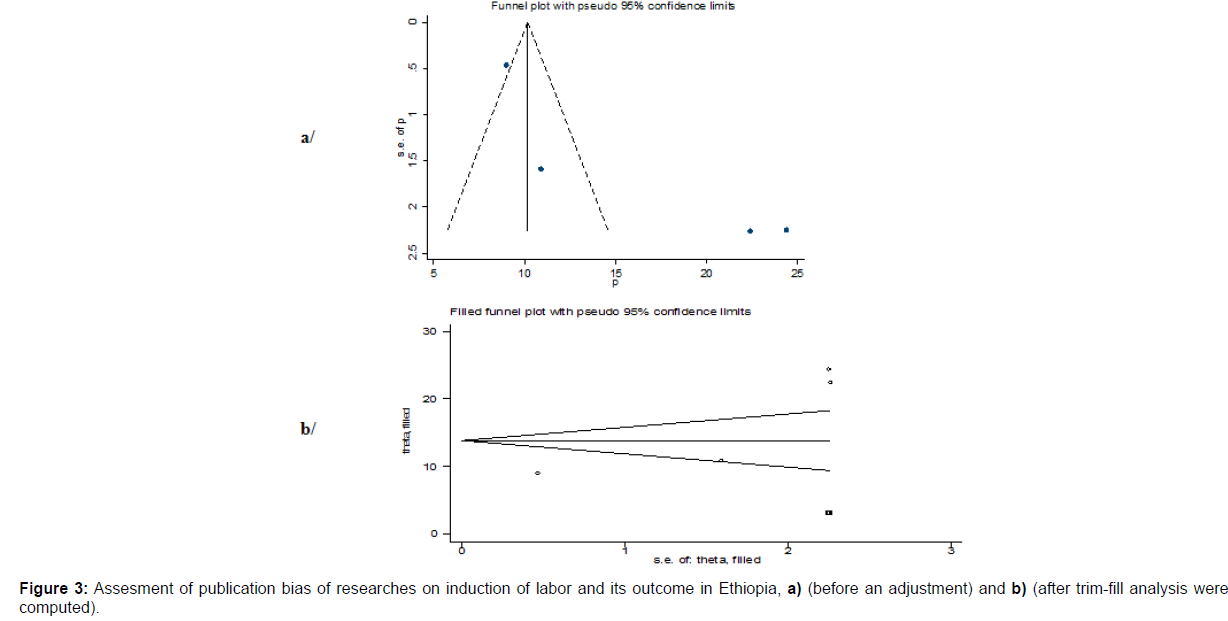
Publication bias
A funnel plot was assessed for the asymmetry distribution of induction of Labor in Ethiopia by visual inspection (Figure 3). Egger's regression test showed with a p-value of 0.004 indicated the evidence for publication bias. Hence, trim and fill analysis was conducted to overcome the publication bias. 1 study filled with a total of 4 studies and overall, 5 studies were enrolled and computed through the trim and fill analysis with a pooled prevalence of 13.83% (95% CI; 7.64- 20.0.3) using a random effect model [24].
Sensitivity analysis
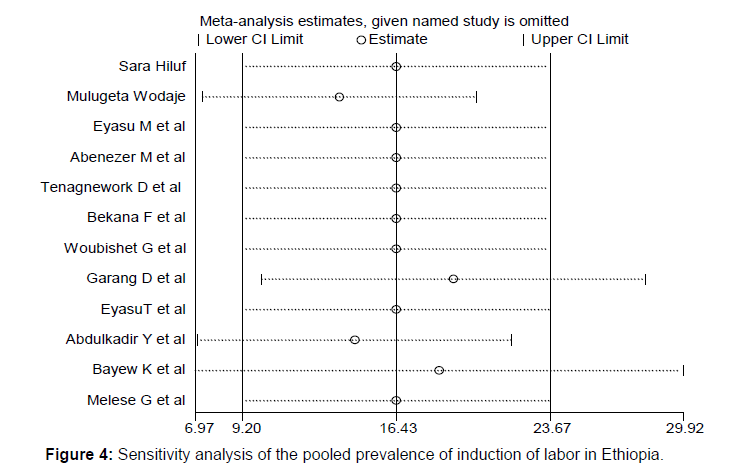
This systematic review and meta-analysis showed the point estimate of its omitted analysis lies within the confidence interval of the combined analysis (Figure 4).
Factors associated with successful induction of labor in Ethiopia
For this systematic review and meta-analysis, the most associated risk factors with successful induction of labor included gestational age < 42 weeks and Bishop score > 5 (Table 3).
| Variables | Model | Egger test (P-value) |
Status of heterogeneity | AOR (95%CI) | I2 (%) |
|---|---|---|---|---|---|
| Gestational age < 42 weeks | Fixed | 0.655 | No heterogeneity | 4.3 (1.63,11.36) | 0.0 |
| Bishop score > 5 | Random | 0.742 | Low heterogeneity | 5 (3.59,6.97) | 42.3 |
Table 3: Summary of factors associated with success of induction of labor in Ethiopia.
Factors for failed induction of labor in Ethiopia For this systematic review and meta-analysis, the most commonly associated risk factors for failed induction of labor included nulliparity, gestational age > 42 weeks and unfavorable Bishop score (Table 4).
| Variables | Model | Egger test (P-value) |
Status of heterogeneity | AOR (95%CI) | I2 (%) |
|---|---|---|---|---|---|
| Nulliparity | Random | 0.546 | Moderate heterogeneity | 2.9(1.95,4.31) | 53.5 |
| Gestational age ≥ 42 weeks | Fixed | 0.655 | No heterogeneity | 4.5(2.47,8.05) | 0.0 |
| Unfavorable Bishop score | Random | 0.742 | Low heterogeneity | 5.2(3.65,7.31) | 21.0 |
Table 4: Summary of factors associated with failed induction of labor in Ethiopia.
Discussion
In this systematic review and meta-analysis, pooled prevalence of induction of labor in Ethiopia was 16.43% (95% CI; 9.2, 23.67). This is in line with findings from Nepal [9.72%] [25], SouthWest Nigeria [12.9%] [26] and Tanzania [21.63%] [12]. In the mean time this prevalence was higher than findinges of Nigera (11.5%) [11], DR congo (3.2%) [10] another study from Tanzania (2.3%) [27]. This may be due to the variance in study design, sample size, time gap and difrence in sociodemographic charecterstics of participants. In the study from Congo pregnancies lower than 37 weeks gestation were excludes and in the study from Tanzania fetouses with congenital anomalies and intrauterine dath were excluded. However the pooled prevalence of this study was lower than findings from The United States of America (24.5%) and Sri Lanka (35.5%) [28]. The reason behind might be deference in socio demographic characteristics of participants, expanded obstatric care available at the developed countries and Africa as whole is concidered to have the lowest number of induction of labor compared to western countreies [14].
The overall pooled prevalence of successful induction of labor in Ethiopia was 48.12%. This figure is lower than findings from Nigeria [75.9%] [11] Kenya [62%] [29] and Nepal [58.33%] [30]. The reason behind might be due to the difference in method where in the study from Nigeria induction was was primary done by using Misoprostol. Misoprostol ripens the cervex at the same time causes utrin contractions which makes it more effective. In the study from Kenya the difference may due to variation in defination of failed induction of labor which extended to 24 hr.
According to this systematic review and meta-analysis, successful induction of labor was associated with Gestational age < 42 weeks (AOR:4.3, 95% CI:1.63, 11.36) and Bishop score > 5 (AOR: 5 95% CI:3.59, 6.97).
Pregnancies where gestational age was < 42weeks had the odds of 4 time to have successful inducion of labor than their counter parts. Even though some literatures sugesst that induction prior to post-term leads to a substantially increased possible additional complications related to the intervention, initiating induction of labor specially at or beyond 37 weeks is associated with a sucssful vaginal delivery and clear reduction of both fetal and maternal morbidities. It also lowers caesarean rates without increasing rates of operative vaginal births and fewer NICU admissions due to induction [31].
Mothers that had a Bishop score > 5 were 5 times more likely to have a successful outcome of labor induction. Successful induction of labor is clearly related to the state of the cervix that is, the length, thickness, and particularly the consistency of the cervix were important parameters to consider before induction of labor [32].
The pooled prevalence of failed induction was 20.65%. This finding is comparable with the cohort study from Tanzania which is 19% [31]. However this finding was lower than the report from different countries which is 25% in Pakistan [33], 36.5% in South West Nigera [26] and 50.5% in India [34]. Justification for this variance could be difference in methdology, sociodemographic variation of participants and time gap. In the study from pakistan the diffrence could be due to the deference in methodology where only nulliparous woman were involved when being nuliparous is a known risk factor to develop a failed induction and in the study from India failed induction was defined based on mode of delivery which is caesarean section.
According to this systematic review and meta-analysis failed induction was significantly associated with Null parity (AOR:2.9, 95%CI:1.95, 4.31), Gestational age > 42 (AOR:4.595% CI:2.47, 8.05) and Unfavorable Bishop score (AOR 5.2:95% CI:3.65, 7.31).
Participants that are nulliparous were nearly 3 times more likely to have a risk of failed IOL than multiparous mothers. This finding is also mentioned on a number of literatures [3, 33, 35]
Being nulliparous is high-risk pregnancy with several associated obstetric complications like prolonged duration of labor and it is also associated with a higher rate of assisted vaginal delivery. Previous other studies in different parts of the word have show increasing rates of cesarean delivery in general and especially among nulliparous women due to failed induction [35].
Having a gestational age > 42 weeks had the odds of 4 times to develop failed IOL. This association is also supported by other studies [36, 37]. According to different literatures pregnancies that go beyond 42 weeks of gestation are associated with increased fetal and neonatal mortality and morbidity as well as maternal morbidity on the contrary when gestational age of a fetus is advanced induction of labor is justified to reduce the risk of perinatal mortality in post term pregnancies due to ageing of placenta [38]. Literatures suggest that fetal, neonatal and maternal complications associated with this condition have always been underestimated [39] and the finding from meta-analysis indicated that advanced gestational age is associated with failed induction due to intrapartum complications as fetal distress and prolonged duration of labor.
Mothers that had unfavorable Bishop score were 5 times more likely to encounter failed IOL. Which is also supported by studies done accrose the world [30, 40, 41]. Women with unfavorable cervix, who have not experienced cervical ripening phase prior to labor, present the greatest challenge with regard to labor induction. Many investigators have identified the importance of assessing cervical status prior to induction of labor [40]. Cervical ripening is required to increase the chances of successful induction of labor when the Bishop score is low [41].
Limitation
As many of the studies included were cross-sectional, the outcome variables might be affected by other confounding variables in nature and temporal cause and effect relationship may not be well addressed. 9.Conclusion
The overall pooled prevalence Induction of labor among pregnant women was highr than other African countries. Gestational age < 42 weeks and Bishop score > 5 were associated with success of induction of labor while Null parity, Gestational age > 42 weeks and Unfavorable Bishop score showed significant association with failed induction. This finding is important to design strategic policies and to prevent emergency neonatal and maternal complications during the childbirth and postpartum periods.
Declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Materials
All related data has been presented within the manuscript. The dataset supporting the conclusions of this article is available from the authors on request.
Competing Interests
The authors declare they have no competing interests.
Funding
No funding was obtained for this study.
Author’s Contributions
EA and FW took part in the design, selection of articles, data extraction and drafted the manuscript. FW performed statistical analysis. TW and BA critically reviewed the manuscript. All authors read and approved the final version of the paper.
Acknowledgments
Not applicable
References
- Organization WH. WHO recommendations for induction of labour: World Health Organization 2011.
- Leduc D, Biringer A, Lee L, Dy J, Azzam H, et al. (2015) Induction of labour. J Obstet Gynaecol Can 37: 380.
- Rade B, Mitku Y, Weldemicheal A, Zenebe Z, Desalegn A (2018) Induction of Labor and its Determinant Factors: Retrospective Cross-Sectional Study from a Public Hospital in Ethiopia. J Preg Child Health 5: 2.
- Mozurkewich EL, Chilimigras JL, Berman DR, Perni UC, Romero VC, et al. (2011) Methods of induction of labour: a systematic review. BMC Pregnancy and Childbirth 11: 84.
- Girma W, Tseadu F, Wolde M (2016) Outcome of induction and associated factors among term and post-term mothers managed at Jimma University specialized hospital: a two years retrospective analysis. Ethiop J Health Sci 26: 123-132.
- Tolcher MC, Hokenstad AN, Weaver AL, McGree ME, Rose CH, et al. (2019) Clinical Impact of a Restrictive Labor Induction Approval Process. Gynecol Obstet Invest 84: 166-73.
- Berhan Y, Dwivedi A (2007) Currently used oxytocin regimen outcome measures at term & postterm. I: Outcome indicators in relation to parity & indication for induction. Ethiop Med J 45: 235.
- Curtin SC, Osterman MJ, Uddin SF, Sutton SR, Reed PR (2013) Source of payment for the delivery: births in a 33-state and District of Columbia reporting area, 2010. National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Centre for Health Statistics, National Vital Statistics System 62: 1-20.
- Zeitlin J, Mohangoo A, Delnord M, Cuttini M (2013) Committee E-PS, The second European Perinatal Health Report: documenting changes over 6 years in the health of mothers and babies in Europe. J Epidemiol Community Health 67: 983-985.
- Tandu-Umba B, Tshibangu RL, Muela AM (2013) Maternal and perinatal outcomes of induction of labor at term in the university clinics of Kinshasa, DR Congo 2013. Open J Obstet Gynecol 3: 154-157.
- Lawani OL, Onyebuchi AK, Iyoke CA, Okafo CN, Ajah LO (2014) Obstetric outcome and significance of labour induction in a health resource poor setting. Obstet Gynecol Int 419621.
- Tarimo CS, Wu J, Obure J, Mahande MJ (2020) Prevalence, associated factors, and outcomes for labor induction at a tertiary hospital in Northern Tanzania: A retrospective cohort study 2000-2015.
- Batinelli L, Serafini A, Nante N, Petraglia F, Severi FM, et al. (2018) Induction of labour: clinical predictive factors for success and failure. J Obstet Gynaecol 38: 352-358.
- Vogel JP, Souza JP, Gülmezoglu AM (2013) Patterns and outcomes of induction of labour in Africa and Asia: a secondary analysis of the WHO Global Survey on Maternal and Neonatal Health 8: e65612.
- Melkie A, Ewunetu M, Asmer S, Mekie M, Dagnew E (2019) Determinants of failed oxytocin induction among women who gave birth at referral hospitals of Amhara region, Ethiopia, 2018: A case control study.
- Hiluf S (2015) Assessment of Prevalence and Factors Affecting Success of Induction of Labour among Women Attended Induction in Army Referral and Teaching Hospital Addis Ababa Jun 2015: Addis Ababa University.
- Wodaje M (2018) Prevalence and failure rate of inducvtion of labor with thier associated factors among women delivered in woldia general hospital, Northern Ethiopia 2018.
- Gebreyohannes RD, Mesfin E (2020) Determinants of outcome of Induction of Labor in Four Teaching Hospitals in Addis Ababa, Ethiopia. Ethiop Med J 58.
- Dilnessa T (2019) The Proportion of Failed Induction of Labour and Associated Factors among Women Undergoing Induction of Labour in Dessie Referral Hospital: Northeast Ethiopia 2019.
- Hurissa BF (2015) MGaTB. Prevalence of Failed Induction of Labor and Associated Factors Among Women Delivered in Hawassa Public Health Facilities, Ethiopia. J Women’s Health Care 4: 2-6.
- Lueth GD, Kebede A, Medhanyie AA (2020) Prevalence, outcomes and associated factors of labor induction among women delivered at public hospitals of MEKELLE town-(a hospital based cross sectional study). BMC Pregnancy and Childbirth 20: 1-10.
- Bekru ET, Yirdaw BE (2018) Success of labour induction institution based cross-sectional study Wolaita Sodo, South Ethiopia. Int J Nurs Midwifery 10: 161-167.
- Abdulkadir Y, Dejene A, Geremew M, Dechasa B (2017) Induction of labor prevalence and associated factors for its outcome at Wolliso St. Luke. Catholic Hospital, South West Shewa, Oromia. Intern Med 7: 2.
- Tesemma MG, Sori DA, Gemeda DH (2020) High dose and low dose oxytocin regimens as determinants of successful labor induction: a multicenter comparative study. BMC Pregnancy and Childbirth 20: 1-8.
- Lamichhane S, Subedi S, Banerjee B, Bhattarai R (2016) Outcome of Induction of Labor: A Prospective Study. Ann Int Med Dent Res 2: 6-10.
- Bello FA, Akinyotu OO (2016) Predictors of successful induction of labour at a tertiary obstetric service in Southwest Nigeria. Trop J Obstet Gynaecol 33: 143-148.
- Jaiswal S (2015) Indications, methods and outcome of induction of labor at Muhimbili national hospital, Dar es salaam, Tanzania: Muhimbili University.
- Rodrigo DN (2018) Induction of labour in an outpatient setting. Memorial Oration.
- Masan EJ (2013) Outcomes of induction of labor in women who delivered at Kenyatta national hospital: University of Nairobi.
- Rayamajhi RT KC, Shrestha N, Padhye SM (2009) Induction and predictors for failed induction at KMCTH. Kathmandu Univ Med J 7: 21-25.
- Tarimo CS (2019) Prevalence and predictors of failure in labor induction among pregnant women delivered in Northern-Tanzania 2000-2015: A Registry-based Retrospective Cohort Study. Tanzan Med J 30: 13-36.
- Lyndrup J, Legarth J, Weber T, Nickelsen C, Guldbæk E (1992) Predictive value of pelvic scores for induction of labor by local PGE2. Eur J Obstet Gynecol Reprod Biol 47: 17-23.
- Khan NB, Ahmed I, Malik A, Sheikh L (2012) Factors associated with failed induction of labour in a secondary care hospital. J Pak Med Assoc 62: 6.
- Tripathy P, Pati T, Baby P, Mohapatra SK (2016) Prevalence and predictors of failed. Int J Pharm Sci Rev Res 39: 189-94.
- Mbukani R, Kakoma J (2012) Is Nulliparity A Risk Factor For Poor Obstetrical And Neonatal Outcomes In Rwandan District Hospitals? A Prospective Observational Study at Muhima District Hospital. Rwanda Med J 69: 50-53.
- Heffner LJ, Elkin E, Fretts RC (2003) Impact of labor induction, gestational age, and maternal age on cesarean delivery rates. Obstet Gynecol 102: 287-293.
- Verhoeven CJ, Van Uytrecht CT, Porath MM, Mol BWJ (2013) Risk factors for caesarean delivery following labor induction in multiparous women. J Pregnancy 2013: 820892.
- Hannah ME (1993) Post term pregnancy: should all women have labour induced ? A review of the literature. Fetal Matern Med Rev 5: 3-17.
- Galal M, Symonds I, Murray H, Petraglia F, Smith R (2012) Post term pregnancy. Facts, Views & Vis Obstet Gyn 4: 175.
- Caughey AB, Sundaram V, Kaimal AJ, Cheng YW, Gienger A, et al. (2009) Maternal and neonatal outcomes of elective induction of labor. Evidence Report/technology Assessment 176: 1-257.
- Obstetricians ACo, Gynecologists (2009) ACOG practice bulletin no. 107: Induction of labor. Obstet Gynecol 114: 386-397.
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Citation: Kassahun EA, Sendeku FW, Gezahegn TW, Alemayehu BA (2022) Induction of Labor and Factors Associated with its Outcome in Ethiopia A Systemic Review and Meta-Analysis. J Preg Child Health 9: 509. DOI: 10.4172/2376-127X.1000509
Copyright: © 2021 Kassahun EA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2604
- [From(publication date): 0-2022 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 1989
- PDF downloads: 615