Indication Criteria of Imaging Exams for Diagnosing of Temporomandibular Joint Disorders
Received: 03-Aug-2014 / Accepted Date: 09-Sep-2014 / Published Date: 12-Sep-2014 DOI: 10.4172/2161-0681.1000190
Abstract
The various subtypes of temporomandibular disorders and different imaging exams available for diagnosis and indication influence the choice of the most appropriate examination front of clinical symptoms of the patient. This review aims to provide an indication of imaging tests for the diagnosis of pathological changes of the temporomandibular joint, discussing its accuracy and criteria for the prescription. The indication is considered appropriate when based on safety and clinical relevance of the examination requested. This sets the correct diagnosis and influences on the most appropriate treatment plan. We proposed that each of the imaging tests has its own sensitivity and specificity to subtypes and different manifestations of temporomandibular joint disorders.
Keywords: Temporomandibular joint disorders, Diagnostic imaging, Temporomandibular joint, Magnetic resonance imaging, Tomography, X-ray computed, Radiography
309980Introduction
The Temporomandibular Joint (TMJ) is the most used in the human body and is able to simultaneously move bilaterally by one jaw bone [1-3]. The components of TMJ-the condyle, glenoid fossa and articular tubercle, articular disc, retrodiscal tissue, synovial membrane and joint capsule [1,2]-often undergo remodeling processes and physiologic adaptation [3]. However, the Temporomandibular Disorder (TMD) is commonly observed with structural changes and functional derangements of the TMJ [4,5], stomatognathic own and adjacent structures such as chewing muscles, ligaments, teeth and periodontal tissue [4,5]. TMD patients complain of local or diffuse painful manifestations [6], committed by joint and / or muscle symptoms. The range of clinical signs and symptoms are wide and often diagnostic confirmation by different imaging tests available is required [6-11].
This review aims to present the main techniques of diagnostic imaging of the TMJ and stomatognathic structures. Discuss its indications, based on its accuracy, advantages and disadvantages.
Articular TMD Etiology, Classification and Diagnosis
The etiology of articular TMD is not fully understood [9,11] and its risk factors are about trauma, parafunctional habits, postural condition, occlusal microtrauma, systemic predisposition, sleep disorders, psychosocial deleterious change [9-16].
For didactic purposes, the American Academy of Orofacial Pain (AAOP) classified the DTM into two major groups: muscle and articular [12]. The articular TMD affects about 30% of the population as asymptomatic mode, in the form of joint internal derangement, comprising disk displacements and structural changes due to osteoarthritis and osteoarthrosis [4,13,14]. The Table 1 shows the diagnostic subtypes of articular TMD.
| Aplasia | |
|---|---|
| Congenital or developmental disorders | Hypoplasia |
| Hyperplasia | |
| Dysplasia | |
| Acquired disorders | Neoplasms |
| Disorders disc derangement | Disc displacement with reduction |
| Disc displacement without reduction | |
| TMJ dislocations (dislocations) | |
| Inflammatory disorders | Synovitis / capsulitis |
| Polyarthritis | |
| Noninflammatory disorders | Primary osteoarthritis |
| Secondary osteoarthritis | |
| Anchylosis | |
| Fracture (condyle) | |
Table 1: Classification diagnostic proposed by AAOP.
The evaluation of clinical history and physical examination show the diagnosis of articular TMD [9,11,17]. Nevertheless, methods of diagnostic imaging of the TMJ measure the degree of integrity of its components, the functional relationship between they confirm the extent or stage of progression of the disease known, evaluating and documenting treatment effects already set [11,12,18], needed for evaluation in cases of trauma, occlusal changes, limited mouth opening, presence of joint noises, systemic joint diseases, infection and failure of conservative treatment [16].
Diagnostic Imaging
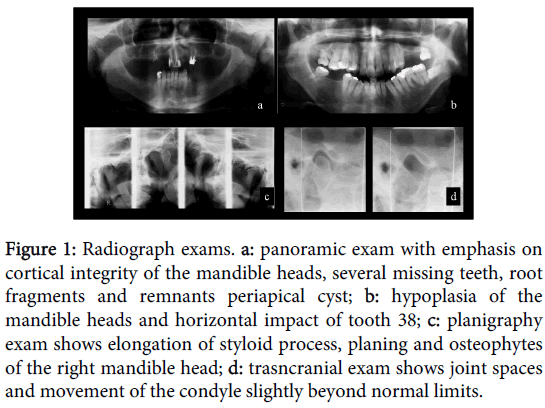
Radiographic methods of ATM assess the morphological characteristics of the osseous components of the joint, adjacent structures and the mouth opening function , however, are inefficient for viewing soft tissue [2,17,19]. The anatomical location and the technical limitations of radiographic techniques determine the difficulty of clear viewing and no overlap TMJ [19,20]. Therefore, one must consider the need of identifying details, the clinical manifestation, the number of symptomatic information for the diagnosis, the low-cost of these tests and their lower radiation dose compared to Computed Tomography (CT) [5,17]. The radiographic techniques used for diagnosis of TMD are: panoramic, transcranial and planigraphy [2,5,16,18] (Figure 1).
Figure 1: Radiograph exams. a: panoramic exam with emphasis on cortical integrity of the mandible heads, several missing teeth, root fragments and remnants periapical cyst; b: hypoplasia of the mandible heads and horizontal impact of tooth 38; c: planigraphy exam shows elongation of styloid process, planing and osteophytes of the right mandible head; d: trasncranial exam shows joint spaces and movement of the condyle slightly beyond normal limits.
The Panoramic radiographs favoring an overview of the jaws, so they are useful in the differential diagnosis of odontogenic changes [16,21]. It shows asymmetries, erosions, osteophytes, fractures, changes in size and shape, and degenerative metabolic evidence, growth changes, jaw tumors, metastases and ankylosis, especially when advanced [2,16,18,19]. The overlap of the images of the skull base and the zygomatic arch are their main limitation [5,17,19,21] (Figure 1a and 1b).
The planigraphy is also called panoramic specific programs for ATM and has considerable accuracy, with minimum overlap. In addition to the joint structures, it allows the contour evaluation of surrounding the TMJ structures as styloid process, mastoid process and zygomatic arch [5,18,22,23]. Provides a direct comparison of both sides as excursion of the condyle, which is useful in confirming the clinical suspicion of hypermobility [2,5]. Presents certain magnification cause of the technique, but it is useful for functional evaluation of mouth opening, evaluation of morphological change and joint spaces, dimension analysis, fractures and ankylosis [5] (Figure 1c).
The transcranial radiographs favor a good anatomical evaluation of the condyle, fossa and articular tubercle [2,17,20]. The x-ray is oblique through the skull to the contra lateral TMJ, aiming to decrease overlap by a sagittal view [20]. Useful for identifying bone abnormalities, visualization of displaced fractures of the neck and head of the mandible, tour and determination of radiographic joint space [5,17,20]. Some overlap and beyond the need to use complex positioning cephalostat are limitation of this projection [2,16,17,20] (Figure 1d).
Other radiographic techniques combined assess different planes and determine the fractures extent, degenerative joint disease, postoperative conditions, ankylosis and cancer [5]. Moreover, it promotes the anatomic relationships of the lesion adjacent areas with more diagnostic accuracy, surgical planning and promoting more efficient therapeutic [18]. Submental (or submentvertice), transfaringeana, transmaxillary reverse towne, anteroposterior and lateral radiograph are the main used [5,16,18]. The use of combined radiographic images has become less common due to increasing use and availability of CT [16,18].
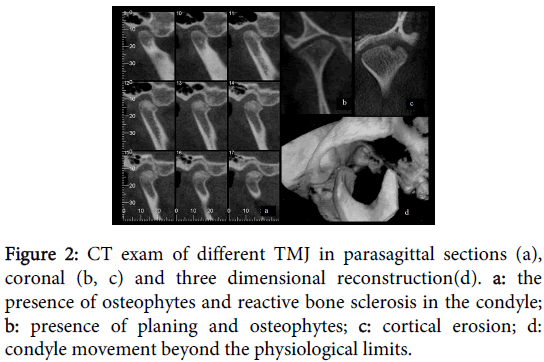
A computed tomography of the TMJ joint is a set of highly accurate images that use ionizing radiation X-controlled and processed by computer systems emission [4]. Maxillofacial dental diagnosis is usually made by cone beam computed tomography (CBCT) [5,24]. Its main advantage is the observation of the articular bone structures in planes: sagittal, coronal and axial [2,24], beyond the possible manipulation of images at different depths and three-dimensional reconstruction [17,24,25].
The main indications of CBCT include structural evaluation of osseous components of the TMJ, when it shows fractures, neoplasm, ankylosis, erosive degenerative changes, pseudo cystic, osteophytic asymptomatic bone remodeling, condylar hyperplasias, coronoid and styloid processes, persistent foramen Huschke, and synovial chondromatosis or metabolic arthritis. It also includes the assessment of pre and post-surgical conditions [4,17,18,22,25-27].
In this technique no bone overlaps and gets a great minimizing noise and artifacts [2,21,28]. However, the soft tissue and disc are not displayed retrodiscal [5,28]. Cost and radiation exposure are greater than conventional radiographic techniques [2,17,18,21].
Figure 2 shows morphological changes in the articular bone components diagnosed by the CBCT technique.
Figure 2: CT exam of different TMJ in parasagittal sections (a), coronal (b, c) and three dimensional reconstruction(d). a: the presence of osteophytes and reactive bone sclerosis in the condyle; b: presence of planing and osteophytes; c: cortical erosion; d: condyle movement beyond the physiological limits.
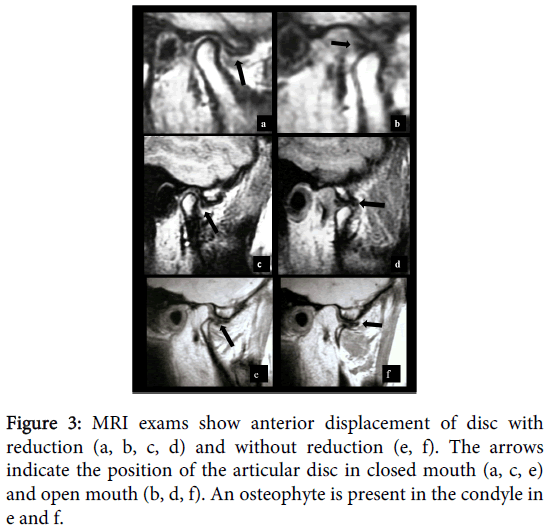
Pathological processes involving the TMJ soft tissue are better visualized by Magnetic Resonance Imaging (MRI) [4,29-33]. The high diagnostic accuracy promote articular disc evaluation, ligaments, retrodiscal tissues, synovial content, chewing muscle adjacent besides the cortical and medullar integrity of bone components [2,5,18,28]. By using computational mechanisms, the technique allows three-dimensional analysis in the axial, coronal and sagittal planes, such as computed tomography. It is considered the gold standard for the disc place assessment and moderately sensitive to degenerative changes intrarticular [5,29,33].
The persistent symptoms of joint pain or preauricular after conservative treatment and clicks remains, crackles, functional changes during mouth opening, subluxations and dislocations frequent, limited mouth opening movement with end stiffness, suspicion of neoplasic processes, osteoarthritic symptoms or asymptomatic osteoarthritis determine the MRI indication [2,4,16,18,22,27]. Often, the MRI records the usual maximum intercuspidal position, maximum mouth opening and intermediate opening positions in T1-weighted, T2 and proton density (PD), in the sagittal and coronal planes [18]. At T1 weighting is possible to get an improved anatomical detail; while PD shows injuries and disc changes [33]. T2-weighted images record the intrarticular inflammation, characterized by joint effusion and bone marrow edema [4,5,33].
Its main advantages include: detection of changes in soft tissue, necrosis, edema, is a noninvasive procedure and does not offer exposure to ionizing radiation [4,5,18,19,33]. Its disadvantages are the high cost, need for sophisticated systems, be contraindicated for patients with poor adherence, claustrophobic, patients with pacemakers, metal heart valves, ferromagnetic foreign bodies and pregnant women [17,18,29]. Figure 3 shows morphological changes of the articular disc and bone structures diagnosed by MRI.
The use of ultrasound examination (US), mainly as high-resolution imaging instruments are a useful option to the disc place evaluation [7,29]. Though present considerable diagnostic sensitivity, specificity has insufficient for identification of osteoarthritis [30]. However, the method is able to identify the effusion in patients with this inflammatory condition associated with pain, demonstrated by MRI examination [29,31]. Even with limitations, it is a useful option for the first study of internal TMJ dysfunction [18,29,30], especially in patients contraindicated for MRI [17]. Moreover, it is more affordable, promotes real-time without the use ionizing radiation and is faster and more comfortable exam [7,29-31].
The US is commonly used in the differential diagnosis of glandular changes and adjacent structures such as TMJ and masseter [32]. It clarifies the symptoms between sialadenitis, sialolithiasis, Eagle’s syndrome, TMD, myofascial pain, nerve pain syndrome and orofacial pain [25]. Another indication of the US examination is the correct place of the joint spaces for infiltrative therapies as arthrocentesis and viscosupplementation. It provides dynamically and in real-time, the correct site of the articular components, as the joint spaces assessment at post adequate washing and lubrication [34].
The nuclear medicine examinations deal with the diagnosis by detecting specific pharmacological concentrations of radioactive substances, which determine changes in metabolic bone activity expressed by images [35]. Bone scintigraphy has requested for defining regions of neoplasia, metabolic disorders, bone growth, synovitis and osteoarthritis [17,18,35,36,37]. It is a test with considerable sensitivity, lower aggressive, high organ specificity, using low levels of radiation [38]. Have some advantages over x-rays, CT and conventional MRI, cause it provide metabolism and inflammation estimation [35-37]. It can perform early diagnosis and provide more affordable cost than CT and MRI [37]. However, it does not differentiate scar bone abnormalities, infections and tumors or osteoarthritic manifestations [18].
The positron emission tomography (PET) is usually indicated for evaluation and staging of metastatic tumours. It is able to show precise morphological and functional metabolic information [22,38]. Its main advantages are images in three dimensions, ease of anatomical visualization, significantly reducing the time required for diagnosis and treatment [18]. Currently, there is the use of SPECT/CT examination with 99m Tc-MDP (Single Photon Emission Computed Tomography with Technetium-Metilenodisfosfonato99m) [35]. This technology allows multiplanar imaging acquisition, and 3D visualization. The 99mTc radiopharmaceutical is able to show osteometabolic local rate, while the tomographic technique shows the mapping of disease [35,37]. As in PET, a single image displays the anatomical and functional data. Its highly sensitive and specific are the greatest advantage [35,38]. The nuclear medicine examinations differ by radiopharmaceuticals / radioisotopes, capture form, radiation dose, sensitivity and results presentation [18].
Prescription Imaging for the Diagnosis of Articular TMD
The correct indication of an imaging exam should to base on the own need of the patient, his clinical symptoms and complaints investigated, obtained during history taking and physical examination [18,39,40]. The basic principle of further examination indication says that only when the clinical evaluation is not enough for making the diagnosis and treatment plan guides the professional as to control unnecessary requests [24]. One of the flaws in the drafting of diagnosis and treatment planning process occurs by misguided or unnecessary indication of diagnostic exams for purposes that are not intended. This fact occurs due to lack of knowledge by professionals in the directions of the applicable exams [39]. To conservative or non-surgical joint treatment, one should consider the risk of damage and the safety of diagnostic techniques [18]. Conventional radiographs and CT scans are dangerous due to absorption of radiation by these techniques [18,39].
The need diagnostic imaging, or the staging of the disease, or when the exam is essential for treatment plan determine the use of higher doses radiation technical. The metabolic changes to growth and metastasis define the nuclear medicine examinations use due its complex diagnosis and treatment [35-39]. However, still need confirmation of the nature of growth through specific tests such as histopathology or immunohistochemistry [18]. For the articular TMD, physical exams palpation, measurement of movement, functional testing and evaluation of joint sounds are instruments of great diagnostic validity when performed by trained and calibrated professional [9]. However, the overlap of muscle and joint symptoms may interfere with diagnostic characterization as both manifest functional impairment. In this and in cases of non-specific symptoms (inflammation, cancer, and trauma), additional imaging exams are essential to clarify the diagnosis and definition of right therapy [4,9].
Imaging exams, from simple to more complexes, have different degrees of sensitivity and specificity, properties that confer their diagnostic power [41]. MRI and CT are methods with higher accuracy compared with conventional radiology, because of the higher resolution anatomical they provide. CT is gold standard for bony structures evaluation and the method of choice for the trauma face, whereas MRI is considered to study soft tissue [2,4,19,29,39]. The two methods often complement the study of changes in TMJ, constitute important tools for muscle and joint differential diagnosis [4]. Though the MRI is able to diagnose all bone changes of TMJ, TC is more accurate to these hard structures [28]. Recent Searches [7,8,29-31,34,40] recommend us as a safe diagnostic technique, non-invasive and considerable accuracy for the positioning of the articular disc, especially for patients contraindicated to MRI examination or underwent interventions real-time, as viscosupplementation.
However, radiographs may show high diagnostic accuracy, especially when associated with clinical symptomatology data [21]. An example is the case of radiographic records of the condyle hyper excursive movement patients with clinical presentation of joint clicks terminal, determining the diagnosis of hypermobility joint, evident by a simple image as transcranial or planigraphy [5]. This example shows the image is very sensitive, whereas clinical data confer specificity, ruling out other diagnostic possibilities. Similarly, morphological alterations of the styloid, coronoid and condylar process are evaluated with high diagnostic accuracy by radiographs low-cost and complexity of implementation, as planigraphy and panoramic [23,39], even though the TC indicated as the gold standard for evaluation these changes [4].
The decision on the choice of the exam should consider its influence on the diagnostic and therapeutic proposition. The professional should to assess If the clinical indication is a conservative therapy can control symptoms in the short-term [2,18]. At the most, when conservative therapy is faulty and there is invasive therapeutic indication, the professional should choose highly sensitive diagnostics. Elaborate treatment plans also require accurate and complete images [39,41]. For suspected fractures, for example, CT is able to diagnose its occurrence, providing exact location and sizing, determining the appropriate surgical rehabilitative therapy [4]. Such reasoning is the same to tumor changes evaluation [42]. A study that compared the accuracy of imaging for detection of bone tumors revealed that diagnostic nuclear medicine examinations has greater sensitivity and specificity than CT scans, MRI and radiographic [35,37-39,42].
Table 2 gathers and sorts the information in different examination techniques for the TMJ images, based on their indications, risks and diagnostic power.
| Disorders | Sign Researched | Main exams indicated | |
|---|---|---|---|
| Congenital or developmenta l disorders |
Aplasia | no structure | CT, Radiographics Exams |
| Hypoplasia | size reduction | CT, Radiographics Exams | |
| Hyperplasia | dimensional increase | CT, Radiographics Exams | |
| Dysplasia | structural change | Nuclear Medicine, CT, Radiographics Exams | |
| Acquired disorders | Neoplasm | formation / bone destruction | Nuclear Medicine, CT, MRI |
| growth of the soft tissue | Nuclear Medicine, MRI, US | ||
| metastasis | Nuclear Medicine | ||
| Disorders disc derangement | displacement | ||
| with reduction | disc recapture | MRI, US | |
| displacement | |||
| without reduction | no disc recapture | MRI, US | |
| TMJ dislocations (dislocations) | open lock | Clinical Diagnosis, Radiographics Exams, CT | |
| Inflammatory disorders | Synovitis / capsulitis | effusion, inflammation, pain | MRI, US |
| Polyarthritis | Polyarticular cortical remodeling | CT, MRI, Radiographics Exams | |
| Non inflammatory disorders | Primary osteoarthritis | uni / bilateral cortical alteration, remodeling | |
| Secondaryosteoarthritis | CT, MRI, Radiographics Exams | ||
| Anchylosis | bone formation, compromised moviment | CT, Radiographics Exams, MRI | |
| Fracture (condyle) | asymmetry, the fracture | CT, Radiographics Exams | |
Table 2: Indication of imaging exams for the articular TMD diagnosis. CT: Computed Tomography; MRI: Magnetic Resonance Image; US: Ultrasound.
Conclusion
The factors evaluated during indication of TMJ imaging tests involve: the necessity of determining the disease and its prognosis on clinical information available; doubt for the differential diagnosis of TMD; the development stage of the disease; the preoperative preparation; treatment assessment; safety and accuracy of the exam.
The different exams have specific indications for the diagnosis of articular TMD:
Radiographic examinations have lower cost and lower radiation dose and lower sensitivity. They diagnostic less complex assessments and first differential diagnosis between TMD and inflammatory dental and jaw conditions.
CT scans are sensitive and specific for the morphological, degenerative and articular fractures bone changes. CBCT is the gold standard for reviews of maxillofacial hard tissue.
Inflammatory changes, articular disc place and other soft tissue structures are clearly visualized and evaluated by MRI examination. It can also be assessed by US examination, which is also indicated for the differential diagnosis between TMD and painful conditions of major salivary glands. It is useful to pre and post-assessment of therapies for infiltration, as viscosupplementation and arthrocentesis.
Nuclear medicine examinations are primarily indicated for evaluation of metabolic change, growth, and tumor metastasis.
References
- Bó WAD, Martins Junior JC, Hoyuela C, Guimarães S, Keim FS, et AL (2012) Efetividade da cirurgiaartroscópica da ATM empacientes com limitação de abertura de bocadecorrente do deslocamento anterior do disco articular semredução: revisão de literatura. Rev Bras Cir Craniomaxilofac 15(1): 25-34.
- Mahl CRW, Silveira MW (2002) Diagnósticoporimagens da articulaçãotemporomandibular: técnicas e indicações. JBA 2(8): 327-332.
- Bonis RD (2007) Articulaçãotemporomandibular: estudoanatômico e videofluoroscópico. Radiol Bras 40(5): 320.
- Garcia MM, Machado KFS, Mascarenhas MH (2008) Ressonânciamagnética e tomografiacomputadorizada da articulaçãotemporomandibular: além da disfunção. Radiol Bras 41(5): 337–342.
- Guimarães JP, Ferreira LA (2012) Atlas de diagnósticoporimaginologia das desordenstemporomandibulares, Editora UFJF, Juiz de Fora Brazil.
- Gatchel RJ, Stowell AW, Wildenstein L, Riggs R, Ellis E 3rd (2006) Efficacy of an early intervention for patients with acute temporomandibular disorder-related pain: a one-year outcome study. J Am Dent Assoc 137: 339-347.
- Landes CA, Goral WA, Sader R, Mack MG (2006) 3-D sonography for diagnosis of disk dislocation of the temporomandibular joint compared with MRI. Ultrasound Med Biol. 32(5):633-639.
- Cakir-Ozkan N, Sarikaya B, Erkorkmaz U, Aktürk Y (2010) Ultrasonographic evaluation of disc displacement of the temporomandibular joint compared with magnetic resonance imaging. J Oral MaxillofacSurg 68: 1075-1080.
- Carrara SV, Conti PCR, Barbosa JS (2010) Termo do 1º consensoemdisfunçãotemporomandibular e dororofacial. Dent Press J Orthod.15: 114-120.
- Ferreira LA, de Oliveira RG, Guimarães JP, Carvalho AC, De Paula MV (2013) Laser acupuncture in patients with temporomandibular dysfunction: a randomized controlled trial. Lasers Med Sci 28: 1549-1558.
- Liu F, Steinkeler A (2013) Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent Clin North Am 57: 465-479.
- Fujiwara M, Honda K, Hasegawa Y, Hasegawa M, Urade M (2013) Comparison of joint pain in patients diagnosed with and without articular disc displacement without reduction based on the Research Diagnostic Criteria for Temporomandibular Disorders. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 116: 9-15.
- Grossmann E, Januzzi E, Iwaki Filho L (2013) O uso do hialuronato de sódio no tratamento das disfunçõestemporomandibularesarticulares. Rev Dor. 14: 301-306.
- Güler N, Uçkan S, Imirzalioglu P, Açikgözoğlu S (2005) Temporomandibular joint internal derangement: relationship between joint pain and MR grading of effusion and total protein concentration in the joint fluid. DentomaxillofacRadiol. 34: 175-181.
- Hunter A, Kalathingal S (2013) Diagnostic imaging for temporomandibular disorders and orofacial pain. Dent Clin North Am 57: 405-418.
- Vasconcelos BCE, Silva EDO, Kelner N, Miranda KS, Silva AFC (2002) Meios de diagnóstico das desordenstemporomandibulares. Rev Cir TraumatBuco-Maxilo-Facial. 1(2):49-57.
- Lewis EL, Dolwick MF, Abramowicz S, Reeder SL (2008) Contemporary imaging of the temporomandibular joint. Dent Clin North Am 52: 875-890, viii.
- Cozzolino FA, Rapoport A, Franzi SA, Souza RP, Pereira CAB et al.(2008) Correlação entre osachadosclÃnicos e imaginológicosnasdisfunçõestemporomandibulares. Radiol Bras. 41: 13–17.
- Almeida SM, Bóscolo FN, Pereira TCR (1997) Estudocomparativo entre duastécnicasradiográficastranscranianasutilizando o cefalostato ACCURAD-200, nasposiçõespadrão e corrigida, e confecção de gabaritosparadelimitação dos espaçosarticulares. Rev OdontolUniv São Paulo. 11: 51- 60.
- Hintze H, Wiese M, Wenzel A (2009) Comparison of three radiographic methods for detection of morphological temporomandibular joint changes: panoramic, scanographic and tomographic examination. DentomaxillofRadiol. 38: 134-140.
- Scolozzi P, Becker M, Lombardi T (2012) Mandibular condylar metastasis mimicking acute internal derangement of the temporomandibular joint. J Can Dent Assoc 78: c77.
- Guimarães SMR, Carvalho ACP, Guimarães JP, Gomes MB, Cardoso MMM, et al. (2006) Prevalência de alteraçãomorfológica do processoestilóideempacientes com desordemtemporomandibular. Radiol Bras.39: 407–411
- Rodrigues MGS, Alarcón OMV, Carraro E, Rocha JF, Capelozza ALA (2010) Tomografiacomputadorizadaporfeixecônico: formação da imagem, indicação e critériosparaprescrição. OdontolClÃnCient. 9: 115-118.
- Santana Júnior PJ, Teixeira KISS, Torres PPTS, Daher RT, Santana PKV, et al. (2009) Qual o seudiagnóstico? Radiol Bras. 42(4):XI–XII
- Reis HN, Carvalho ACP, Leite HF, Mello RCM, Xavier SS (2006) Persistência do forame de Huschke: um estudotomográfico. Radiol Bras. 39: 273-276.
- Gonzalez FM, Paes Junior AJO, Tornin OS, Souza RP (2005) Carcinoma espinocelular do condutoauditivoexterno: estudoportomografiacomputadorizada de seiscasos. Radiol Bras. 38: 181-185.
- Alkhader M, Ohbayashi N, Tetsumura A, Nakamura S, Okochi K, et al. (2010) Diagnostic performance of magnetic resonance imaging for detecting osseous abnormalities of the temporomandibular joint and its correlation with cone beam computed tomography. DentomaxillofacRadiol 39: 270-276.
- Jank S, Zangerl A, Kloss FR, Laimer K, Missmann M, et al. (2011) High resolution ultrasound investigation of the temporomandibular joint in patients with chronic polyarthritis. Int J Oral MaxillofacSurg 40: 45-49.
- Mello Junior CFD, Saito ODC, GuimarãesFilho Hà (2011) Avaliaçãoultrassonográfica dos distúrbiosintracapsularestemporomandibulares. Radiol Bras. 44: 355-359.
- Bas B, Yilmaz, N, Gökce E, Akan H (2011) Ultrasound assessment of increased capsular width in temporomandibular joint internal derangements: relationship with joint pain and magnetic resonance grading of joint effusion. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 112:112-117.
- Yang H, Huynh DH, Ceponis A, Kavanaugh A, Arthur (2013) Parotid ultrasound abnormalities among rheumatoid arthritis patients: prevalence and clinical correlates. Arthritis Rheum. 65: 400.
- Ramos ACA, Sarmento VA, Campos PSF, Gonzalez MOD (2004) Articulaçãotemporomandibular-aspectosnormais e deslocamentos de disco: imagemporressonânciamagnética. Radiol Bras. 37: 449-454.
- Dayisoylu EH, Cifci E, Uckan S (2013) Ultrasound-guided arthrocentesis of the temporomandibular joint. Br J Oral MaxillofacSurg 51: 667-668.
- Coutinho A, Fenyo-Pereira M, Dib LL, Lima EN (2006) The role of SPECT/CT with 99mTc-MDP image fusion to diagnose temporomandibular dysfunction. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 101: 224-230.
- Bittencourt LP, Souza SAL, Magnanini M, Fonseca LMB, Gutfilen B (2005) Verificação da atividadecondilarempacientes com padrãoesqueléticoclasse III porintermédio da cintilografiaóssea. Radiol Bras. 38: 273-277.
- Brasileiro CB, Cardoso VN, Ruckert B, Campos TPR (2006) Avaliação de processosinflamatóriosnaarticulaçãotemporomandibularempregandoleucócitosautólogosmarcados com tecnécio-99m emmodelo animal, Radiol Bras. 39: 283-286.
- Shintaku WH, Venturin JS, Yepes JF (2009) Application of advanced imaging modalities for the diagnosis of metastatic adenocarcinoma of the lungs in the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 107: e37-41.
- Pharoah MJ (1999) The prescription of diagnostic images for temporomandibular joint disorders. J Orofac Pain 13: 251-254.
- Bas B, Yılmaz N, Gökce E, Akan H (2011) Diagnostic value of ultrasonography in temporomandibular disorders. J Oral MaxillofacSurg 69: 1304-1310.
- Calderon PDS, Reis KR, Araujo CDRP, Rubo JH, Conti PCR (2008) Ressonânciamagnéticanosdesarranjosinternos da ATM: sensibilidade e especificidade. Rev Dent Press OrtodonOrtopedi Facial. 13: 34-39.
- Shintaku WH, Venturin JS, Langlais RP, Clark GT (2010) Imaging modalities to access bony tumors and hyperplasic reactions of the temporomandibular joint. J Oral
Citation: Ferreira LA, Francischetti FL, Ferraz Júnior AML, Paula MVQ, Januzzi E (2014) Indication Criteria of Imaging Exams for Diagnosing of Temporomandibular Joint Disorders. J Clin Exp Pathol 4:190. DOI: 10.4172/2161-0681.1000190
Copyright: © 2014 Ferreira LA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 22138
- [From(publication date): 11-2014 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 17189
- PDF downloads: 4949