Incomplete Ring of Cervical Abscesses
Received: 23-May-2016 / Accepted Date: 17-Jun-2016 / Published Date: 24-Jun-2016 DOI: 10.4172/2161-119X.1000240
Abstract
Cervical fascia and spaces can mobilize the spread of infections which are localized at first. Knowledge about these spaces and their relations are indispensable for the correct treatment of the abscesses in the deep neck spaces.
Background
Deep cervical infections are infections of various spaces created between the cervical fascia which divide the neck.
The neck can be divided into two major division cervical fascia: the superficial layer and the deep layer. They can extend from the skull base to the chest, and envelop muscles, neurovascular bundles, aerodigestive tract and thyroid gland, and create potential spaces.
• In suprahyoid neck: buccal, canino, masticador and parotid spaces.
• In infrahyoid neck: peritonsillar, submandibular, sublingual and parapharyngeal spaces.
• Anterior area: visceral space
• Posterior area: Retropharyngeal, danger and prevertebral and Carotid sheath
• Spaces
An understanding of this anatomy of neck is necessary to the adequate treatment of deep neck infection, because an infection of one of these spaces may spread to neighboring areas.
We describe the case of a patient who presented, in association with tonsillitis, abscesses in both parapharyngeal spaces, together with an affected retropharyngeal area, with an antelateral extension reaching the midline before the thyroid gland, creating an incomplete ring of abscesses in the deep spaces of the neck
Case Report
A 33 year old woman, immunocompetent, came to the emergency department for dysphagia and progressive neck pain. No associated difficulty in breathing or fever.
Three days earlier she had been diagnosed with tonsillitis and had started treatment with Amoxicillin 750 mg.
Physical examination revealed redness and tonsilar enlargement, and erythema together with swelling around the neck (mainly on the left side).
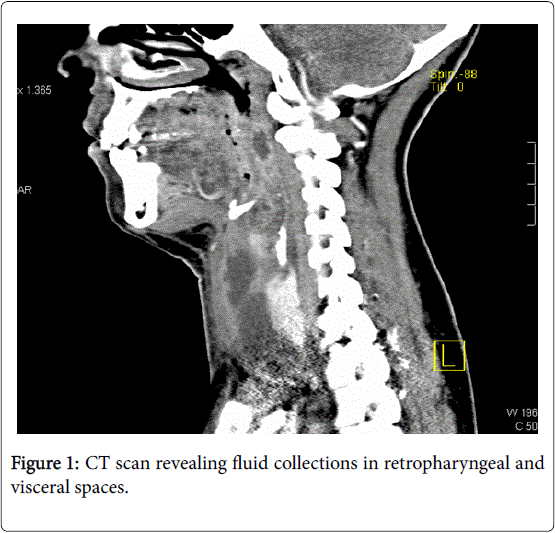
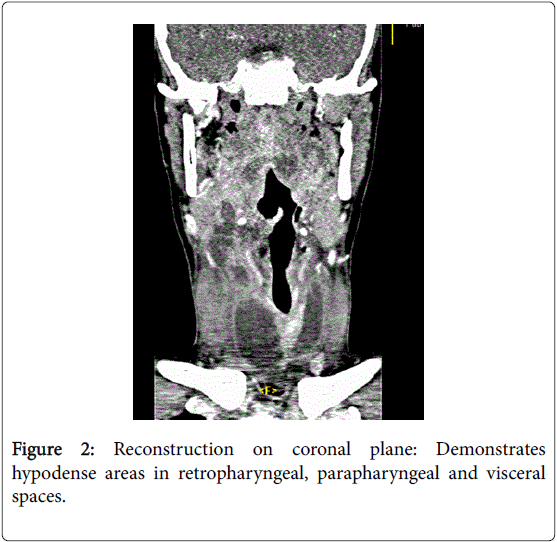
The CT showed several collections in the retropharyngeal, in both the parapharyngeal and visceral spaces (Figures 1 and 2).
Abscesses were drained with a combined approach (oral and anterior cervical discectomy to access the purulent material in different spaces) to and empirical treatment with meropenen and cloxaciline was established (which was maintained as the microbe isolated in cultures was Prevottella oralis), along with proton-pump inhibitor and corticosteroid therapy.
After completing 15 days of intravenous antibiotic treatment, with a good clinical response and improvement both in analytics (normalized to discharge) and radiological tests (the control CT did not show signs of collections) which led to the decision of discharging the patient home and outpatient monitoring.
Discussion
Although the incidence of deep cervical abscess has reduced since the use of antimicrobial drugs and improved of dental hygiene [1], currently there is still significant associated mortality. Failure to recognize this infection can lead to dramatic complications: compromised airways, jugular thrombophlebitis, carotid artery compromise, cavernous sinus thrombosis, Lemiere´s syndrome, Horner´s syndrome, epidural abscess, cranial nerve dysfunction (IXXII), mediastinitis and pericarditis [2].
The principal causes of deep cervical abscesses are oropharyngeal and odontogenic infections. Other causes are intravenous drug abuse, trauma, foreign bodies or salivary pathology [3].
Most abscesses are polymicrobial with aerobic and anaerobic bacteria. In our case, we only isolated Prevotella oralis , an anaerobic organism as common as Fusobacterium and Peptostreptococcus [1,4].
The main symptom in our patient was pain and neck swelling, but the deep cervical abscess can cause others such as a sore throat, fever, lockjaw and respiratory distress.
Currently the treatment is based on antibiotic use which covers the anaerobic and aerobic flora which may be the cause of these infections. On occasion surgical drainage of these abscesses is used, above all if deterioration is observed in the patient or there is no favourable response in the first 48 h of the antimicrobial treatment. Furthermore at times the permeability of the airway may be compromised which may require a tracheotomy in the patient (12-16% of patients with profound cervical abscesses) [5].
Learning Point
Anatomical knowledge on the fascia and cervical spaces of the neck are essential for understanding the routes of propagation in deep neck infections.
Pharyngealtonsillar infections are a frequent cause of cervical abscesses. From peritonsillar and parapharyngeal spaces, the infection can spread to surrounding areas such as the retropharyngeal space.
The retropharyngeal space affected especially in pediatric patients, by the involvement of retropharyngeal lymph nodes (Glands of Henle). Typically these nodes regress to 5-6 years of life (explaining the minor involvement of this region in adults).
Treatment of deep cervical abscesses includes antibiotics and sometimes surgical drainage.
References
- Parhiscar A, Har-El G (2001) Deep neck abscess: A retrospective review of 210 cases. Ann OtolRhinollaryngol 110: 1051-1054.
- Sethi DR, Stanley RE (1994) Deep neck abscessess – changing trends. J LaryngolOtol 108: 138-143.
- Gadre AK (2006) Chapter 47.Infections of the Deep Spaces of the Neck. In: Bailey BJ, Johnson JT, Newland SD. Head & Neck Surgery–Otolaryngology, 4th edn. Philadelphia, PA: Lippincott Williams & Wilkins.
- Weed HG, Forrest LA (2005) Deep Neck Infections. In: Cummings CW, Flint P, Harker LA. Cummings Otolaryngology, 4th edn. Philadelphia, PA: Elservier.
- Sakaguchi M, Sato S, Ishiyama T, Katsuno S (1997) Charaterization and management of deep neck infections. Int J Oral MaxillofacSurg 26: 131-134.
Citation: Maeso-Plaza AM (2016) Incomplete Ring of Cervical Abscesses. Otolaryngol (Sunnyvale) 6:240. DOI: 10.4172/2161-119X.1000240
Copyright: © 2016 Maeso-Plaza AM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 11068
- [From(publication date): 6-2016 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 10192
- PDF downloads: 876