Incidental case finding of a sublingual thyroglossal duct cyst
Received: 02-Apr-2024 / Manuscript No. roa-24-134241 / Editor assigned: 05-Apr-2024 / PreQC No. roa-24-134241 / Reviewed: 19-Apr-2024 / QC No. roa-24-134241 / Revised: 24-Apr-2024 / Manuscript No. roa-24-134241 / Published Date: 29-Apr-2024
Abstract
Thyroglossal duct cysts are prevalent congenital cervical anomalies, affecting approximately 7% of the population. They can emerge at various locations along the thyroid's migration path, extending from the base of the tongue to the lower neck. Here, we present the case of a 27-year-old female patient with an unremarkable medical history, who presented with a one-month history of nasal obstruction. Clinical examination is unremarkable. However, incidental findings on computed tomography and ultrasound revealed a mass located at the base of the tongue, corresponding to a sublingual thyroglossal duct cyst. This occurrence represents a rare and atypical location for such cysts, which we will detail in this article.
Keywords
Thyroglossal duct cysts; Sublingual masses; Cysticmasses
Description
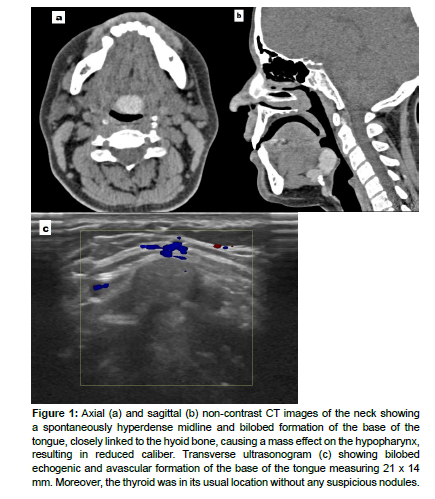
A 27-year-old female patient with no specific medical history presents with one-month history of nasal obstruction ; clinical examination is unremarkable ; computed tomography (CT) of the sinuses is requested [Figure 1].
Figure 1: Axial (a) and sagittal (b) non-contrast CT images of the neck showing a spontaneously hyperdense midline and bilobed formation of the base of the tongue, closely linked to the hyoid bone, causing a mass effect on the hypopharynx, resulting in reduced caliber. Transverse ultrasonogram (c) showing bilobed echogenic and avascular formation of the base of the tongue measuring 21 x 14 mm. Moreover, the thyroid was in its usual location without any suspicious nodules.
Diagnosis: Sublingual thyroglossal duct cyst.
Background
Thyroglossal duct cysts (TGDC) are the most common congenital cervical anomalies, occurring in 7% of the population. They can develop at any location along the thyroid's migration path from the base of the tongue to the lower neck. These cysts typically manifest as midline neck cysts closely linked to the hyoid bone [1].
The thyroglossal duct is the narrow tubular structure remaining from the thyroid’s descent and links the thyroid gland to the foramen cecum ; in normal circumstances it undergoes involution by the tenth week of gestation, but if any segment of the duct persists, secretions from the epithelial lining may lead to inflammation and the formation of TGDC [2,3].
TGDC occurs in 6 different locations[4]: infrahyoid cysts (26–65% of TGDCs), suprahyoid cysts (20–25%), juxtahyoid cysts (15%), suprasternal cysts (fewer than 10%), intralingual cysts (2%), and intralaryngeal cysts (very rare) [4].
We realize then that the tongue represents an uncommon localization for the TGDC, given that involution of the thyroglossal duct usually starts from the cranial end, where thyroid descent first begins [5].
Clinical Presentation
The age of discovery is typically in childhood but some cases can be observed at any age [6].
Classical TGDC often present as asymptomatic neck masses , however, in adults, they are far less common and are usually diagnosed when infected [6]; in this instance patients may report sore throat, erythema, swelling, dysphagia, hoarseness ; these symptoms result from cyst enlargement, with the most serious complication being airway occlusion [6].
A sublingual cyst differs from a classical thyroglossal cyst in many ways. First, it does not present as a neck swelling, secondly the chief complaint is different [7], it may be incidentally detected as is the case for our patient or presents with symptoms ranging from life-threatening neonatal respiratory distress to a seemingly innocuous dysphonia or feeding difficulties [5,8,9].
Key Diagnostic Features
On ultrasound (US), uncomplicated TGDC may appear anechoic and well-circumscribed or pseudosolid due to proteinaceous fluid content, cholesterol crystals, and keratin. The imaging appearance becomes more intricate in cases with a history of infection or hemorrhage, which can manifest as heterogeneous complexes with surrounding tissue edema and lymphadenopathy [10].
CT imaging reveal a well-circumscribed, thin-walled, hypoattenuating lesion with notable rim enhancement and inflammatory changes in the surrounding subcutaneous tissues in cases of infection. The existence of internal debris, high attenuation, or septations is indicative of a previous infection [6,10,11].
Magnetic resonance imaging (MRI) can be employed when there is uncertainty with CT or US imaging. On MRI, lesions will exhibit a high signal on T2-weighted images and a low to intermediate signal on T1-weighted images [11]; if an abscess forms, restricted diffusion will be observed. In cases of severe infection, fistulas may develop following external cyst rupture or in cases of recurrence after surgical resection [11].
Less than 1% of TGDC progress to carcinoma. Papillary carcinoma is the predominant malignancy, accounting for 92.1%, with squamous cell carcinoma following at 4.3%, in this case, the definitive diagnosis is histological [12].
Differential Diagnoses
Vallecular cyst: they are submucosal retention cysts that protrude between the base of the tongue and the anterior free margin of the epiglottis, without extending into the tongue muscles [13].
Dermoid cyst : typically resides above the geniohyoid muscles, appearing on the floor of the mouth, and rarely develops within the intralingual area [14,15]. The MRI examination of a dermoid cyst reveals a complex cyst structure with various compartments, displaying intensities resembling fat due to the presence of sebum or fat within the cyst. These elements exhibit hyperintensity on T1-weighted MR images [16].
Second branchial cleft cysts: situated laterally and do not have an association with the hyoid bone [12].
Benign tumours: haemangiomas, lipomas, papillomas, adenomas and fibromas are infrequently observed in this particular location [9].
Malignant tumours: squamous cell carcinoma and lymphoma [17].
Physiological swellings: hypertrophied lingual tonsil and lingual ectopic thyroid [17].
Treatment
It involves surgical removal to prevent recurring infections and mitigate the small risk of malignancy. Simple excision of these cysts is linked to a relatively high recurrence rate (45% to 55%).
The Sistrunk procedure is widely accepted as the standard surgical approach and has significantly decreased the likelihood of recurrence. This surgical method necessitates a more extensive resection, encompassing the central third of the hyoid bone and a core section of the base of the tongue tissue [18,19].
Informed Consent: Written informed consent was obtained from the patient.
References
- Garcia E, Osterbauer B, Parham D (2019) The incidence of microscopic thyroglossal duct tissue superior to the hyoid bone.Laryngoscope. 129: 1215-1217.
- Ma J, Ming C, Lou F (2018) Misdiagnosic analysis and treatment of pyriform sinus fistula in children. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 53: 381-384.
- Unsal O, Soytas P, Hascicek SO (2017) Clinical approach to pediatric neck masses: Retrospective analysis of 98 cases. North Clin Istanb. 4: 225-232.
- Mittal M, Malik A, Sureka A (2012) Cystic masses of neck: a pictorial review. Indian J Radiol Imaging 22: 334-343.
- Burkart CM, Richter GT, Rutter MJ (2009) Update on endoscopic management of lingual thyroglossal duct cysts. Laryngoscope 119: 2055-2060.
- Deaver MJ, Silman EF, Lotfipour S (2009) Infected thyroglossal duct cyst. West J Emerg Med 10: 205.
- Mukul S, Kumar A, Mokhtar E (2016) Sublingual thyroglossal duct cyst (SLTGDC): An unusual location. J Pediatr Surg Case Rep 10 : 3-6.
- Urao M, Teitelbaum DH, Miyano T (1996) Lingual thyroglossal duct cyst: a unique surgical approach. J Pediatr Surg 1574-1576.
- Santiago W, Rybak LP, Bass RM (1985) Thyroglossal duct cyst of the tongue. J Otolaryngol 261-264.
- Ahuja AT, Wong KT, King AD (2005) Imaging for thyroglossal duct cyst: the bare essentials. Clin Radiol 60 : 141-148.
- Patel S, Bhatt A (2019) Thyroglossal duct pathology and mimicsa . Insights into Imaging 10 : 1-12.
- Amos J, Shermetaro C. Thyroglossal Duct Cyst.
- Berger G, Averbuch E, Zilka K (2008) Adult vallecular cyst: thirteen-year experience. Otolaryngol Head Neck Surg 138: 321-327.
- Mathews J, Lancaster J, O’Sullivan G (2001) True lateral dermoid cyst of the floor of the mouth. J Laryngol Otol 115: 333-335.
- Myssiorek D, Lee J, Wasserman P (2000) Intralingual dermoid cysts: a report of two cases. J Ear Nose Throat 79: 380-383.
- Ro EY, Thomas RM, Isaacson GC (2007) Giant dermoid cyst of the neck can mimic a cystic hygroma: using MRI to differentiate cystic neck lesions. Int J Pediatr Otorhinolaryngol 71: 653-658.
- Gupta M, Singh S, Gupta M (2011) Lingual thyroglossal duct cyst treated by intraoral marsupialisation. Case Reports bcr1120103546-bcr1120103546.
- Pucher B, Jonczyk-Potoczna K, Kaluzna-Mlynarczyk A (2018) The Central Neck Dissection or the Modified Sistrunk Procedure in the Treatment of the Thyroglossal Duct Cysts in Children: Our Experience. Biomed Res Int 8016957.
- Kim JP, Park JJ, Woo SH (2018) No-Scar Transoral Thyroglossal Duct Cyst Excision in Children. Thyroid 28: 755-761.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Bougrine I (2024) Incidental Case Finding of a Sublingual ThyroglossalDuct Cyst. OMICS J Radiol 13: 562.
Copyright: © 2024 Bougrine I. This is an open-access article distributed underthe terms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 743
- [From(publication date): 0-2024 - Mar 29, 2025]
- Breakdown by view type
- HTML page views: 568
- PDF downloads: 175