Case Report Open Access
Improving Oral Health of Young Children: An Interprofessional Demonstration Project
Marguerite A. DiMarco*1, Karen Fitzgerald2, Evelyn Taylor3, Deborah Marino2, Marlene Huff2, Diana Biordi2 and Eric Mundy21Case Western Reserve University, Frances Payne Bolton School of Nursing, Room 322, C, Cleveland, OH 44106-4904, USA
3Nutrition Center, The University of Akron, USA
- *Corresponding Author:
- DiMarco MA
Associate Professor Emeritus, The University of Akron, Associate Professor Case Western Reserve University
Frances Payne Bolton School of Nursing, Room 322 C
Cleveland, OH 44106- 4904, USA
Tel: 216-368-0593, 330-416-9922
E-mail: mxd50@case.edu, dimarco@uakron.edu
Received Date: June 15, 2016; Accepted Date: June 24, 2016; Published Date: June 30, 2016
Citation: DiMarco MA, Fitzgerald K, Taylor E, Marino D, Huff M, et al. (2016) Improving Oral Health of Young Children: An Interprofessional Demonstration Project. Pediatr Dent Care 1:113. doi:10.4172/pdc.1000113
Copyright: © 2016 DiMarco MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Neonatal and Pediatric Medicine
Abstract
Introduction: The CDC report on oral health found that preschool children have increasing incidence of dental caries especially poor children. Profound disparities exist in dental services obtained by children, especially the poor. Objectives: The purpose of this project is to improve the oral health of vulnerable children via an interprofessional model through the Supplemental Nutrition Program for Women, Infants, and Children (WIC). Methods: This project tested the feasibility of integrating primary preventive interventions of oral health assessments/teaching, fluoride varnishing and referral to a dental home into regular practice at an urban and rural WIC site using nurses, registered dieticians and students. Results: After three years, 4091 children were enrolled and received fluoride varnish. Children who were seen by the nurse/dietician at the urban or rural WIC sites were found to have more children seeking dental services through a dentist between the 2nd and 3rd WIC visits (p<0.001). Children at both sites increased their brushing or cleaning their child’s teeth between the first and second visits (p<0.05 for the rural site; p<0.001 for the urban site). Conclusion: Interprofessional cooperation along with a community based approach is needed to tackle this increasing problem of early childhood dental caries.
Keywords
Oral health; Fluoride varnish; WIC; Preschool children; Interprofessional
Introduction
Our nation’s children are suffering! They are suffering from dental decay. The Surgeon General declared dental caries the “Silent Epidemic”. Profound disparities exist in dental services obtained by children, especially the poor. Even when providing dental services, children with Medicaid were statistically less likely to be treated by a dentist than those with private insurance, comparatively at percentages of 55% versus 68% [1]. Poor and/or minority families are affected most [2] with preschool children having increasing rates of dental caries compared to other age groups [3]. Approximately 23% of children aged 2–11 years have one or more untreated tooth decays and 20% of adolescents aged 12–19 years have one or more permanent tooth decays3. The American Dental Association and the American Academy of Pediatric Dentistry among others suggest the ideal standard is to establish a dental home by one year of age. Of particular concern is the low rate of early detection and preventive care for 3 year old and younger children eligible for Medicaid due to a shortage of dentists who accept Medicaid and who are willing to treat children. The CDC report on oral health found that preschool children have increasing incidence of dental caries with the prevalence of dental caries even higher in lower-income families3. Poor children have higher rates of dental disease compared to other children and their lack of access to dental care and untreated dental conditions can contribute to poor health, dysfunctional speech, compromised growth, and poor educational performance [4,5].
Successful primary prevention helps avoid the suffering, cost and burden associated with disease. It is considered one of the most cost-effective practices of health care. Therefore, an interprofessional primary prevention approach in a community setting, serving children and their caregivers focusing on dental education, oral hygiene skills, fluoride varnish application and referral to dental home is one means to manage this epidemic in low income children.
Children who receive early preventive dental care have 40% lower dental costs over their lifetime than those who do not receive this care [6]. Numerous studies demonstrate the value of applying fluoride varnish to children’s teeth as a means of decreasing the incidence of dental caries [7]. Caries reduction rates vary; however, a meta-analysis of Duraphat trials reveals 38% reduction in cavities; semi-annual application in 3-yr-olds produced a 44% reduction in two years [8]. In addition, primary health care providers can now be reimbursed through Medicaid for fluoride varnishes to preschoolers as a primary prevention method.
In this initiative, WIC eligible children (ages under 5) were recruited. WIC (Supplemental Nutrition Program for Women, Infants, and Children) is a national program that safeguards the health women, infants, & children who are at nutritional risk by providing nutritious foods to supplement diets, counsel on healthy eating, and referrals to health care. WIC clients are low income; eligibility requires a gross income at or below 185% of the U.S. Poverty Income Guidelines. WIC was chosen because poor and/or minority families are affected most with dental caries, with preschool children having increasing rates of dental caries compared to other age groups [9,10]. Children from impoverished families as well as uninsured families were significantly associated with feelings of caregiver burden, leading to less preventive dental use. According to a recent study run by the Department of Oral Health Sciences at the University of Washington, over 60% of participating dental providers had out-of-pocket health care expenses relating to a child’s oral condition, resulting in barriers stemming from financial burden [11]. Poor and minority children under 5 years of age are significantly less likely to have preventive or restorative dental visits, and to have more unmet treatment needs and more caries than non-minority children or those from higher incomes. Minority and low-income groups have barriers to dental services due to limited resources, competing family needs, and challenges related to providers and insurance [5,12].
Even when Medicaid provides dental services, only 33% of eligible children receive preventive or restorative dental service due to a shortage of dentists who accept Medicaid and who are willing to treat children [13]. Dentists only receive 60% of dental services billed to Medicaid and, depending on the procedures, may not receive any compensation. Accordingly, Michigan dentists were recently surveyed in accordance to AAPD (American Academy of Pediatric Dentistry) recommendations. Of the 229 participants, 47% were not willing to accept Medicaid patients [14]. Projected Medicaid and State Children’s Health Insurance Program cuts are expected to cause one million or more children to lose health coverage that paid for dental health. Uninsured children are 6 times more likely to lack a source of dental care than insured children and four times as likely to have unmet dental needs [15] and approximately one fourth of children in the U.S. do not have any form of private or public dental insurance [3]. In Ohio, dental care remains the most common unmet need for almost 157,400 children, regardless of financial status [16]. Primary care providers and other health professionals are needed to prevent caries in young children. Fewer than 3% of Medicaid children see a dentist before the age of three, but 78% of children fewer than 3 years of age see a primary health care provider and attend WIC [17].
Primary Causes of Tooth Decay
The bacterium S. mutans is the main contributor to tooth decay. Adults may have higher amount of S. mutans in their mouth and can transmit it to their infant or child through the exchange of saliva. Frequent sugary snacking and drinking interact with S. mutans, producing acids that can cause mineral loss from teeth increases the risk for tooth decay. Dental caries affect more children in the United States than any other chronic infectious disease. Tooth decay and other oral diseases that can affect children are preventable. Fluoride varnish can reduce cavities in preschool children by 30-40%. A panel of experts from the American Dental Association (ADA) Council on Scientific Affairs recently assessed 71 trials from 82 articles to establish the efficacy of topical fluoride caries-preventive agents. The ADA currently recommends 2.26 percent fluoride varnish for prevention of dental carries in children ages 6 and younger [7] (Figure 1).
Tooth decay of the front top teeth is referred to as Early Childhood Caries (ECC) formerly called Baby Bottle Tooth Decay. Causes of ECC include poor oral hygiene, not enough fluoride, sleeping with a bottle or sippy cup, frequent snacking and bottle/sippy cup, feedings containing beverages high in sugar, milk, or formula during the day or night, coating pacifiers with sweeteners like sugar or honey, and having a mother/caregiver or sibling who has had active tooth decay in the past 12 months. ECC and tooth decay in general is a multifactorial disease and a child could have a few of these factors and not have decay while other children may have only one factor and have decay. Also some foods cause tooth decay more than others called cariogenic foods ECC develop in young children who use Sippy cups or baby bottles constantly and have poor nutrition with a history of eating frequently or eating the wrong foods [18] (Table 1).
| Cariogenic foods (cause tooth decay) | Cariostatic foods (raise the oral pH and |
|---|---|
| Frequent intake and stickier textures increase | prevent tooth decay) |
| Breads, crackers, cereal | Cheese (Swiss, Monterey Jack, cheddar etc.) |
| Juice and sweetened drinks | Nuts (over 3 years of age) |
| Chips and pretzels | Vegetables (especially raw to stimulate saliva) |
| Dried fruits and chewy candies | Sugarless gum |
Table 1: Cariogenic foods (cause tooth decay) and Cariostatic foods (raise the oral pH and prevent tooth decay).
The process of decay is mostly influenced by sugars that can be fermented by the bacteria in the mouth, causing a lower pH or acidic environment [19]. This environment works on deteriorating the enamel of the tooth. This demineralization will incite a cavity. Caries in the primary dentition leads to the same in permanent teeth [20].
Another source of caries, aside from poor nutrition choices, is infection. Mothers who pick up their child’s pacifier and put the pacifier in their mouth to clean it off may inadvertently pass on the bacteria, mutans streptococci, which cause dental caries. Along with passing the infection by saliva and mouth kissing the baby, the frequency of eating significantly increases the presence of mutans streptococci [21]. The constant change of the acidity of the mouth’s saliva will cause wear down of the protective enamel setting up the possibility of decay. A human’s saliva has the ability to cause re-mineralization of the tooth’s enamel. Eating foods that keep the acidity of saliva high continues to cause demineralization and the potential for dental caries. The more the teeth are bathed in anything other than water or healthy saliva, the greater the chance of demineralization. Despite our understanding of the risk factors associated with caries in early childhood, caries remains one of the largest untreated conditions in preschool children [22].
Ways to prevent dental disease
Early Childhood Caries (ECC) is defined by the American Academy of Pediatric Dentistry (AAPD) as the presence of one or more decayed, missing (as a result of caries), or filled tooth surfaces in any primary tooth in a child 71 months of age or younger [23]. The AAPD and the American Academy of Pediatricians (AAP) recommend that primary care providers include the following oral health prevention strategies: (1) perform periodic risk assessments to determine the child’s relative risk of developing dental caries; (2) provide anticipatory guidance to parents about oral hygiene, diet, and fluoride exposure; (3) apply appropriate preventive therapies, such as fluoride varnish; and (4) help parents establish a dental home for their children by 12 months of age [24].
Purpose of Project
In Ohio, dental care remains the Number 1 unmet health care need of children and low income adults [16]. The purpose of this project is to improve the oral health of low income pregnant women, mothers, and children. WIC (Supplemental Nutrition Program for Women, Infants, and Children) is a national program implemented by the State. WIC clients are low income; eligibility requires a gross income at or below 185% of the U.S. Poverty Income Guidelines. Regular contact is mandated every 3-6 months between WIC staff and their clients, WIC education includes oral health modules and WIC’s mission of nutritional improvement has links to oral health.
Training non-dental specific health care professionals
The School of Nursing and the Nutrition and Dietetics at a Midwest university have collaborated on many projects. Each program also has educational and service relationships with local WIC sites in urban and rural locations. The objectives from Healthy People 2020 support the improvement of oral health in vulnerable populations [25]. Responding to these concerns, the School of Nursing proposed an interprofessional approach to oral health in vulnerable children and their at-risk mothers. This project employed Nurse Practitioners (NPs), Registered Dietitians (RDs), and Registered Nurses (RNs) at urban and rural pilot WIC sites, using a standard Ohio Department of Health (ODH) protocol to apply fluoride varnish to the teeth of children enrolled in WIC from the development of first tooth buds through 4 years of age. Additionally, the registered dietician’s (RD) scope of practice was systematically expanded by training in fluoride varnish application, oral health assessment and oral health prevention. The project used Smiles for Ohio, the current Ohio Department of Health (ODH) fluoride varnish program, which has well defined guidelines and training programs for non-dental health care personnel on placing fluoride varnish. This program is adapted from the AAP’s oral health programs. The specificity and proven safety of these guidelines make them an ideal template for use in an initiative to increase access to oral health care. A NP, with a specialty in pediatric oral health, conducted the training in standardized oral health assessment and varnishing for NPs, RDs and RNs. Drawing on the current program guidelines, the placement of fluoride varnish on children occurred after an oral health assessment by a NP. In this project the NP or RD performed the oral health assessment after completing the Smiles for Ohio oral health training. The NP and RD developed picture ratings from the AAP and AAPD to maintain inter rater reliability of what the RD and NP labeled a cavity. After the oral health assessment, the NP or RD administered the fluoride varnish to the child. Ongoing semi-annual assessments of the child continued as long as the child was still in the WIC program (under 5 years). The participants were tracked by the RD/NP for fluoride intervention, and parents of the participating child were provided education and referrals to dental homes for themselves and their children. The NP and RD kept the child’s record secure in their office. In addition, parents responded to survey questions at every visit which were entered in SPSS by the evaluators. IRB approval was obtained and permission from WIC was also obtained.
Project Goals
The goals of this project were to: 1) Improve oral health disease in this population; 2) Increase interprofessional collaboration by using NPs, RDs, and RNs to conduct oral health assessments and apply dental fluoride varnishes to at-risk children under five years of age; 3) Increase oral healthcare accessibility by linking services and care at WIC sites emphasizing preventive care, screening and fluoride varnishing, and establishment of a dental home; 4) Increase oral health workforce diversity, capacity, and flexibility through oral assessment and dental fluoride varnishing training programs for NPs, RDs, and RNs; 5) Increase interprofessional collaboration by using NPs, RDs, and RNs to conduct oral health assessments and apply dental fluoride varnishes to at-risk children through 4 years of age with dentist consultations, as needed; and 6) Overcome oral health barriers by using best practices and educational materials from established effective nutritional and oral health professionals and programs. Successful completion of this project will result in a model that can be used by WIC and other assistance programs in Ohio and, perhaps, nationwide to enhance oral health education to pregnant women and mothers and fluoride treatments to vulnerable children.
Project Objectives
The measurable objectives of this project were to: 1) Apply dental fluoride varnish to 40% of the children at each site between the eruption of first tooth buds to five years old in order to reduce the number of cavities in these children by 25%; 2) Enhance the oral health education of 40% of pregnant women and mothers at each site by demonstrating age appropriate oral health techniques; 3) Assist primary caregivers to establish a dental home for 75% of the children by age one as recommended by the American Association of Pediatrics and the American Association of Pediatric Dentistry or after 2 years in the program; 4) Expand the scope of practice for RDs in standardized oral health assessment and fluoride varnish application; 5) Use NPs, RDs, and RNs to apply fluoride varnish apart from well and sick baby visits; and 6) Provide cross-training opportunities for NPs, RDs, and RNs in oral health.
Materials and Methods
WIC program sites are ideal to implement this intervention. The WIC mission is to safeguard the health of low income women, infants, and children and the relationship between oral health, a healthy diet and good nutrition support this important initiative. WIC offers access to the at-risk population and regular contact because new and continuing WIC clients who must come in every 3 months to receive their food coupons. Every 6 months a recertification (verification of eligibility) is completed along with health and nutrition histories.
At most WIC locations nationwide, RDs assess nutritional status, provide nutrition counseling and prescribe food packages. RNs provide similar services at some locations. Each client meets for an individualized nutrition session in which an assessment is completed and nutrition risk determined for each client. Nutrition counseling is provided on areas of risk and referrals for other assistance are made as needed. WIC coupons for specific food packages are given for the next 3 months. There also is a visit every 3 months at which clients get more coupons and participate in nutrition education programs.
Counseling the primary caregiver about the importance of establishing a dental home for the child and other oral health education, followed by an oral health assessment and application of the fluoride varnish was completed during one of these 2 visits and again 6 months later. The routine visit with WIC staff will continue unchanged.
WIC clients were invited to participate in the oral health intervention and parents provided consent for their child to receive fluoride varnishing. Special care was taken in recruitment to avoid any hint that participation in the project will impact receiving food coupons. Mothers/primary child care provider received oral health education and counseling about oral health hygiene. After informed consent, the Project staff assessed the child’s oral health and applied varnish as indicated. Project staff worked with the mother to find a dental home for the child. Project staff conducted orientation sessions for WIC staff explaining project activities.
The typical day included:
1. NP or RD at the WIC clinics obtained informed consent from WIC clients about the free FDA approved fluoride varnish.
2. The guardian was asked to fill out an Oral Health Survey which asked simple questions about the child’s diet and dental care.
3. The RD or NP asked about the infant or child’s dental health, provided education on appropriate dental health, conducted an oral health assessment on child’s teeth, applied fluoride varnish to child’s teeth, kept a dental screen record, and provided written material on oral health
4. The child is seen every 6 months until the study is complete in three years or until the child is too old to participate (reaches their 5th birthday).
5. The RD or NP gave the guardian or parent a list of dentists that the child may be able to receive dental care.
6. After the fluoride varnishing procedure, the parent or guardian was given a satisfaction survey.
7. After the first time visit the child was given a goodie bag containing: Information pamphlets on good dental hygiene Toothbrush, toothpastes, coloring book, crayons, etc. (Figure 2).
Target geographic area
The immediate target area was two counties, an urban county and a rural county, in Ohio. Thereafter, depending on the success of the project, the target area is the entire state of Ohio, and if possible, those WIC sites in the United States which do not have a fluoride program. Expanding this intervention to other locations is voluntary on the part of WIC. For this pilot demonstration project, two WIC locations have enthusiastically agreed to participate, with the approval of the ODH Bureau of Nutrition Services. The urban site hosts 2,400 clients, 1,400 of whom are infants and children, while the rural site has 3,251 clients, which includes 743 women, 894 infants, and 1,614 children.
Target beneficiary
Approximately 4,000 children were projected in the rural and urban counties to be the beneficiaries of this project. Family gross income must fall at or below 185% of the U.S. Poverty Income Guidelines.
Nurse Practitioners (NPs), Registered Dietitians (RDs), and undergraduate/graduate nursing and nutrition students were also involved in the project. At each WIC location there is an individual (RD or NP) trained to apply fluoride varnish (FV) the teeth of WIC clients’ from the appearance of a child’s first tooth bud through four years of age. By training NP’s, RD’s, and RN’s to perform oral health assessment, fluoride varnishing, education, and other preventative care measures could reduce poor oral health in high risk populations.
Results
Demographics
The project ended in Dec. 2013 and the first goal was met as 4091 children participated in program with 1813 children in the urban county and 2278 children in the rural county. Over 1,700 of the children participating in the project (or 41.6%) have returned for a second follow up visit, and 658 (or 16.1%) have been seen for a third visit. Over 180 children (4.4%) have been in the program long enough to have received a fourth fluoride varnish, and even 22 of them have had a fifth varnish (0.5%) (Table 2). In the urban county, 61.5% of the children were black: 26.9% of the children were white: 3.8% of the children were Biracial, and 7.7% were Asian. In the rural county, 27.9% of the children were black; 66.3% of the children were white; 2.3% of the children were biracial, and 3.5% of the children were Asian.
| Program Participation | WIC Site | Both Sites Combined | ||||
|---|---|---|---|---|---|---|
| Urban | Rural | |||||
| n | % | n | % | n | % | |
| Visit 1 | 1,813 | 44.3 | 2,278 | 55.7 | 4,091 | 100 |
| Visit 2 | 697 | 41.0 | 1,005 | 59.0 | 1,702 | 100 |
| Visit 3 | 231 | 35.1 | 427 | 64.9 | 658 | 100 |
| Visit 4 | 43 | 23.6 | 139 | 76.4 | 182 | 100 |
| Visit 5 | 3 | 13.6 | 19 | 86.4 | 22 | 100 |
Table 2: Program Participation (number of children ever varnished).
Dental screening record results
This section outlines the results from the dental screening record. The dental screening record is a form designed to capture several criteria regarding the program participant’s dental characteristics. Such characteristics include the status of the gums and the number of missing, broken, decayed/discolored, filled, and silver capped teeth. The dental screening record also captures the child’s age and gender, as well as a host of materials and topics discussed with the child’s caregiver (parents or guardians).
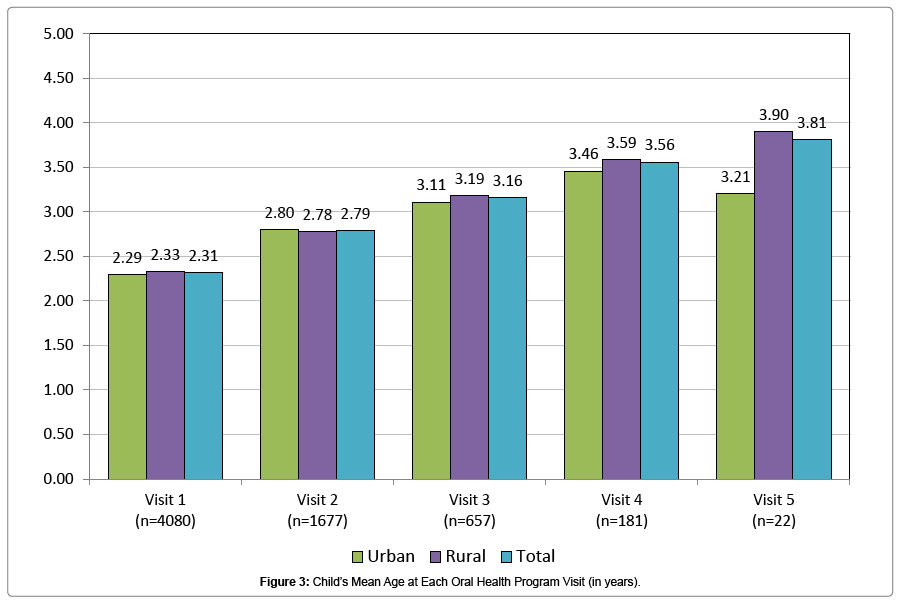
Figure 3 on the following page presents information about the mean ages of the children varnished up to five times through the Oral Health Project at each successive program visit. Results are depicted for each site as well as for the overall project combined.
Oral health habits as reported by parent/guardian
The Parent/Guardian Oral Health Survey is an instrument aimed at exploring children’s oral health habits as reported by their parents or guardians is reported for Tables 3-5. Table 3 also reports on the child’s dietary practices as reported by the parent. Tables 3 and 4 address visits to the dentist and cleaning or brushing of teeth as reported by the parent/guardian.
| Practices Reported: | Program Visit | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Visit 1 | Visit 2 | Visit 3 | Visit 4 | Visit 5 | |||||||||||
| Urban (n=1042) | Rural (n=1501) | Total (n=2543) | Urban (n=638) | Rural (n=959) | Total (n=1597) | Urban (n=229) | Rural (n=420) | Total (n=649) | Urban (n=41) | Rural (n=135) | Total (n=176) | Urban (n=3) | Rural (n=19) | Total (n=22) | |
| More than one sweet drink per day | 47 | 28 | 35.8 | 53.4 | 26 | 36.9 | 52.4 | 26 | 35.3 | 36.6 | 22.2 | 25.6 | 0 | 36.8 | 31.8 |
| Bottle use | 37 | 31.8 | 33.9 | 12.7 | 9.8 | 11 | 7.5 | 3.3 | 4.8 | 2.4 | 0 | 0.6 | 0 | 0 | 0 |
| Sippy cup use | 52.5 | 65.5 | 60.2 | 49.6 | 58.8 | 55.1 | 43.4 | 44.9 | 44.4 | 35.7 | 38.5 | 37.9 | 33.3 | 31.6 | 31.8 |
| Fruits/veggies at least once a day | 97.6 | 89.6 | 92.8 | 97.3 | 85.9 | 90.5 | 96.9 | 85.3 | 90.7 | 97.7 | 88 | 90.9 | 66.7 | 100 | 95.2 |
| High-sugar snacks | 21.2 | 12.9 | 16.3 | 25.9 | 20.1 | 22.4 | 22.7 | 24.1 | 23.6 | 28.6 | 29.6 | 29.4 | 33.3 | 21.1 | 22.7 |
Table 3: Parent/Guardian Reports on Child’s Dietary Practices at Each Oral Health Visit (in percent).
| Program Visit | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| First Visit | Second Visit | Third Visit | |||||||
| Urban | Rural | All | Urban | Rural | All | Urban | Rural | All | |
| Child seen by dentist in past six months | 26.1 (n=1738) | 18.8 (n=1732) | 22.1 (n=3871) | 40.9 (n=679) | 23.6 (n=962) | 30.8 (n=1641) | 46.5 (n=226) | 33.6 (n=423) | 38.1 (n=649) |
| Child’s teeth cleaned or brushed daily | 88.9 (n=1510) | 91.4 (n=1993) | 90.3 (n=3503) | 96.9 (n=636) | 95.2 (n=967) | 95.9 (n=1603) | 98.2 (n=226) | 95.3 (n=651) | 96.3 (n=651) |
Table 4: Child’s Oral Health Habits as Reported by Parent/Guardian at Each Oral Health Visit (in percent).
| First to Second Visit | Urban (n=502) | Rural (n=795) | Combined (n=1297) | |||
|---|---|---|---|---|---|---|
| 1st Visit | 2nd Visit | 1st Visit | 2nd Visit | 1st Visit | 2nd Visit | |
| 87.1 | 96.6** | 92.1 | 95.1* | 90.1 | 95.7** | |
| Second to Third Visit | Urban (n=200) | Rural (n=398) | Combined (n=598) | |||
| 2nd Visit | 3rd Visit | 2nd Visit | 3rd Visit | 2nd Visit | 3rd Visit | |
| 98 | 98 | 92.7 | 95.2 | 94.5 | 96.2 | |
| *Significant at .05 level **Significant at <0.01 level. | ||||||
Table 5: Comparison of Same Children Brushing or Cleaning Child’s Teeth Daily (average percent).
Dietary practices
Table 3 indicates that urban caregivers are more likely to report that their children snack on high sugar foods more than once a day or drink more than one cup of a sweet drink per day. This was especially the case for the first visit, but this difference waned in the case of snacks as visits progressed but not in the case of sweet drinks.
Oral health habits
Tables 4 and 5 outlines the results of two important oral health indicators: recent dentist visits and daily teeth brushings. In general, caregivers of the urban study participants were more likely to indicate their child had seen a dentist within the past six months compared to rural study participants. For instance, 26.1% of urban caregivers reported their child had seen a dentist within the past six months (at their first program visit) compared to 18.8% of rural caregivers at their first visit. The difference was even more dramatic at the second visit when 40.9% of urban caregivers reported their child had seen a dentist and only 23.6% of rural caregivers reported their child had seen a dentist.
A notable dynamic seen in the dental visits data is that the proportion of children seeing a dentist within the past six months increased with each subsequent visit. For instance, 22.1% of all participating children were said to have seen a dentist in the past six months at the first visit. By the second visit the proportion had increase to 30.8% and then to 38.1% by the third visit.
Although not significant, there was the same dynamic of increased activity with each subsequent visit with children’s teeth brushing activity. For instance, 90.3% of all participating children were said to have cleaned or brushed their teeth daily at their first program visit. At the second visit this percentage had increased to 95.9% and then to 96.3% at the third visit.
Early longitudinal comparisons
The following section outlines some early longitudinal analysis for child participants in the Oral Health Project. The analysis examines (1) daily teeth cleaning/brushing activity and (2) dental visits within the past six months for children tracked longitudinally in the program with at least two program visits, and up to three program visits (Table 4).
Teeth Cleaning/Brushing
Table 5 outlines a comparison of the same children with at least three visits to the program in terms of cleaning and brushing of teeth at least once daily between first and second visits, as well as a comparison of the same children from the second to third visits on the same two variables. Further this table presents the means (average proportions) for each visit, and significance test results for the difference of means results. (Pleases note: “Same” children are defined as those children tracked longitudinally. Each child had at least a second program visit and possibly a third visit. Their caregiver’s form or survey responses were linked and compared for analysis.)
The proportion of caregivers reporting that they cleaned or brushed their children’s teeth at least once daily increased from an average of 90.1% for the first program visit to 95.7% for the second program visit, when linking participant responses, across both sites. In the case of the urban comparison site, the proportion of caregivers reporting brushing or cleaning their child’s teeth daily increased from an average of 87.1% for the first program visit to 96.6% for the second program visit, when linking participant responses. At the rural comparison site, the proportion of caregivers reporting brushing or cleaning their child’s teeth daily increased from an average of 92.1% for the first program visit to 95.1% for the second program visit. In both instances, these increases were statistically significant.
In examining changes on the brushing or cleaning the child’s gum or teeth variable between the second and third visits, no significant change was found. This was likely attributable due to a ceiling effect, where many parents were already reporting brushing or cleaning their child’s teeth or gums. For instance, 98.0% of urban parents were already reporting cleaning and brushing their children’s teeth at the second and third program visits. Likewise, rural caregivers also reported high rates of teeth cleaning and brushing (Table 5).
Dental visits
Table 6 outlines a comparison of the same individual children with at least three visits to the program in terms of seeing a dentist between first and second visits, as well as a comparison of the same children from the second to third visits on the same two variables Further this table presents the means (average proportions) for each visit, and significance test results for the difference of means results.
In Table 6, the proportion of the same children seeing a dentist in the past six months has significantly increased for the children involved in the program between the first and second visits. As a case in point, the proportion of caregivers reporting that they have taken their child to the dentist in the past six months increased from an average of 17.7% for the first program visit to 31.4% for the second program visit, when linking participant responses. Moreover, the proportion of caregivers reporting taking their child to the dentist increased from an average of 23.1% from the second program visit to 38.0% for the third program visit. In both instances, these gains were statistically significant increases.
For the urban comparison site, the proportion of caregivers reporting that they have taken their child to a dentist within the past six months increased from an average of 24.0% for the first program visit to 41.5% for the second program visit, when linking participant responses. Furthermore, when comparing those participating in both a second and third program visit, the proportion of urban caregivers reporting that they have taken their child to a dentist within the past six months increased from an average of 33.8% for the second program visit to 45.7% for the third program visit. Likewise, the proportion of rural caregivers reporting that they have taken their child to a dentist within the past six months increased from an average of 17.2% for the second program visit to 33.7% for the third program visit. In all four cases, these increases were statistically significant changes (Table 6).
| Urban | Rural | Combined | ||||
|---|---|---|---|---|---|---|
| (n=638) | (n=880) | (n=1518) | ||||
| 1st Visit | 2nd Visit | 1st Visit | 2nd Visit | 1st Visit | 2nd Visit | |
| First to Second Visit | 24 | 41.5** | 13.1 | 24.0** | 17.7 | 31.4** |
| Urban (n=219) |
Rural (n=395) |
Combined (n=614) |
||||
| 2nd Visit | 3rd Visit | 2ndVisit | 3rd Visit | 2ndVisit | 3rd Visit | |
| Second to Third Visit | 33.8 | 45.7** | 17.2 | 33.7** | 23.1 | 38.0** |
| ** Significant at <0.001 level | ||||||
Table 6: Comparison of Same Children Seeing Dentist in Past Six Months (average percent).
Reasons for not going to the dentist
Also collected on the Parent Guardian Oral Health Survey form is the parent/guardian’s self-reported reasons for not seeing a dentist with their child within the past six months. Table 7 presents the results for parents’ reasons at each of the first three program visits for not seeing a dentist. The analyses took all children at first visit whose parents/guardians reported not seeing a dentist within the past six months. These children were then tracked on the second and third visit.
| Reason Given: | Program Visit | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Visit 1 | Visit 2 | Visit 3 | |||||||
| Urban (n=566) | Rural (n=932) | Total (n=1498)) | Urban (n=134)) | Rural (n=378)) | Total (n=512) | Urban (n=24) | Rural (n=129) | Total (n=153) | |
| My child is too young | 64.1 | 86.1 | 77.8 | 61.9 | 76.5 | 72.7 | 70.8 | 72.1 | 71.9 |
| I don’t know a dentist | 11.5 | 7.9 | 9.3 | 9 | 8.7 | 8.8 | 4.2 | 9.3 | 8.5 |
| fear going to the dentist | 1.8 | 2.5 | 2.2 | 2.2 | 3.4 | 3.1 | 0 | 0.8 | 0.7 |
| We do not have dental insurance | 4.8 | 0.2 | 1.9 | 3 | 0.8 | 1.4 | 8.3 | 0.8 | 2 |
| Transportation is a problem | 3.2 | 0.6 | 1.6 | 5.2 | 0.5 | 1.8 | 0 | 0.8 | 0.7 |
| We cannot afford to go | 1.8 | 0.2 | 0.8 | 0 | 0 | 0 | 4.2 | 0 | 0.7 |
| Don’t accept Insurance | 1.4 | 0.2 | 0.7 | 3 | 0 | 0.8 | 0 | 0 | 0 |
Table 7: Parent/Guardian Reasons for Child not Seeing a Dentist at Each Visit (in percent).
As the Table 7 reveals, by far the primary reason for not seeing a dentist is the misbelief that the child is still too young to see a dentist – despite the best efforts of the clinical staff to ensure parents that their child needs to be seen by a dentist. Over three-quarters, or 77.8%, of the caregivers that had not taken their child to a dentist (at the first program visit) indicated they had not done so because they thought their child was too young. It has been suggested that this pattern is due to some parents encountering dentists who will not see their children because he or she is too young.
The next leading reason cited by caregivers for not taking their child to a dentist (at their first program visit) was not knowing a dentist, or perhaps a dentist that treats young children to go to, with 9.3% non-dentist-seeking caregivers indicating this was the case. Only 2.2% of non-dentist-seeking caregivers reported (at their first program visit) that they had not taken their child to the dentist because they or their child feared the dentist. Smaller portions of non-dentist-seeking caregivers reported
(at their first program visit) that they had not taken their child to the dentist because of issues with transportation, affordability or the ability to pay, or issues with dental insurance or Medicaid (Table 7).
Topics discussed at program visits
Table 8 presents the topics discussed by the staff with the parent at each WIC oral health visit. The fact that at the WIC site “encouraging dental visits” continues at a pretty high rate even at the third visit suggests that perhaps the clinician there is having less success in having the rural families follow her advice or there are less providers.
| Program Visit | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Visit 1 | Visit 2 | Visit 3 | Visit 4 | Visit 5 | |||||||||||
| Topics Discussed: | Urban (n=1805) | Rural (n=2274) | Total (n=4079) | Urban (n=697) | Rural (n=1005) | Total (n=1702) | Urban (n=231) | Rural (n=427) | Total (n=658) | Urban (n=43) | Rural (n=139) | Total (n=182) | Urban(n=3) | Rural (n=19) | Total (n=22) |
| Written materialson oral health given | 98.3 | 98.4 | 98.4 | 96.4 | 97.2 | 96.9 | 97.8 | 99.3 | 98.8 | 100 | 98.6 | 98.9 | 100 | 94.7 | 95.5 |
| Appropriate brushing/use of fluoride for age | 98 | 98.9 | 98.5 | 96 | 97 | 96.6 | 97.4 | 99.3 | 98.6 | 100 | 98.6 | 98.8 | 100 | 100 | 100 |
| Frequency and type of carbohydrate rich snack/beverage | 92 | 53.6 | 70.6 | 91.2 | 33.6 | 57.2 | 87.9 | 35.4 | 53.8 | 81.4 | 29.5 | 41.8 | 33.3 | 31.6 | 31.8 |
| Appropriate use of bottle/Sippy cup | 49.4 | 56.8 | 53.5 | 42.5 | 50.4 | 47.2 | 36.8 | 36.1 | 36.3 | 37.2 | 33.1 | 34.1 | 33.3 | 15.8 | 18.2 |
| Fluoride concerns | 6.5 | 23.5 | 16 | 1.6 | 8.5 | 5.6 | 1.7 | 3.5 | 2.9 | 2.3 | 1.4 | 1.6 | 0 | 0 | 0 |
| Dental visit encouraged | 26.5 | 21.2 | 23.6 | 21.1 | 27.8 | 25 | 19.9 | 32.3 | 28 | 44.2 | 36.7 | 38.5 | 66.7 | 73.7 | 72.7 |
| Sharing germs –maternal/child | 11.9 | 2.1 | 6.4 | 4.9 | 0.2 | 2.1 | 0.9 | 0 | 0.3 | 2.3 | 0 | 0.5 | 0 | 0 | 0 |
Table 8: Topics Discussed By Staff at Each Oral Health Visit (in percent).
Discussion
The goals of the project.
Goal 1: Improve oral health disease in this WIC population.
Goal Met
On the basis of WIC figures, we projected a total target children’s population of about 4000 children at an urban and rural WIC site for preventive fluoride varnishing and education. In fact, even with several months remaining in the project, we have been able, with parental/ guardian permission, to examine and varnish the teeth of about 4100 children at least once (Table 2). A few more than 1700 had two varnishes, and about 700 will have had three varnishes at the conclusion of this project. The data also indicate that we have been able to reduce oral health disease.
Goal 2: Increase interprofessional collaboration by using NPs, RDs, and RNs to conduct oral health assessments and apply dental fluoride varnishes to at-risk children under five years of age; and
Goal 4: Increase oral health workforce diversity, capacity, and flexibility through oral assessment and dental fluoride varnishing training programs for NPs, RDs, and RNs;
Goal 5: Increase interprofessional collaboration by using NPs, RDs, and RNs to conduct oral health assessments and apply dental fluoride varnishes to at-risk children through 4 years of age with dentist (Table 8).
Goals 2, 4, and 5 Met
During the course of this grant, NP’s who are nurses with advanced degrees, taught registered dietitians (RD) how to place children in a comfort position of a child/caregiver’s choice, assess a child’s oral health through the conduct an oral examination, apply fluoride varnish to the child’s teeth, chart appropriately, and educate children and adults as needed. The two disciplines also taught their students the same activities and authenticated and authorized their activities with a certificate when the student’s completion of activities met completion and practice standards.
The two disciplines were able to conduct these activities and meet the standards with little difficulties. Students were able to learn the oral assessment, fluoride varnishing and welcomed having a certificate showing their achievement. Faculty and students saw fluoride varnishing and assessments as an opportunity to expand their scope of practice and demonstrate their competence.
3) Increase oral healthcare accessibility by linking services and care at WIC sites emphasizing preventive care, screening and fluoride varnishing.
6) Overcome oral health barriers by using best practices and educational materials from established effective nutritional and oral health professionals and programs
Goals 3 and 6 Met
The services we have provided at both WIC sites were extremely well liked by the dietetic and staff personnel, as well as the patients, at each site. We were requested to stay, if possible. The project has continued to strive to get more parents connected with a “dental home” (i.e., a steady patient-dentist relationship) at first visit. However the informal feedback received suggests that many caregivers are being turned down by dentists due to their children being too young. There may be an opportunity here to begin a dialog within the community as to the appropriate time for caregivers to begin taking their children to the dentist.
Another area for possible improvement for oral health is related to children’s dietary practices, as reported by the parents/guardians at visits. Nevertheless, the project should be commended for the progress in educating and socializing caregivers in terms of dental care.
Conclusions
The model could be adapted to other programs, such as Head Start programs or at immunization clinics. The project can be sustained by changing Federal and state reimbursements guidelines because current guidelines limit such reimbursements to FV. Such reimbursements can permit expansion of services at WIC locations leading to the possibility of increasing the future dental capacity at WIC participants.
The project had four strengths. 1) A large group of at-risk children, who had limited access to dental healthcare, were systematically identified and preventively treated with fluoride varnish. 2) The dental workforce was expanded to include other professionals, i.e., NPs, RDs, and RNs, thus helping relieve the current strain on dentists and underserviced dental areas. 3) Alternative financial reimbursement options and increasing professional scope of practice provided models for controlling health care costs. 4) Cross-disciplinary healthcare solutions provided a model for interprofessional work and offered opportunities for further collaboration in dental and other health needs, particularly relating to prevention and treatment.
Acknowledgments
Funded by the Kellogg Foundation. Katherine Zheng BSN research assistant for her help on the manuscript. Improving Oral Health of Young Children: An Interprofessional Demonstration Project.
References
- Chi D, Masterson E, Carle A, Mancl L, Coldwell SE (2014) Socioeconomic status, food security, and dental caries in US children: mediation analyses of data from the National Health and Nutrition Examination Survey, 2007-2008. Am J Public Health 104: 860-864.
- Bonito AJ, Cooper LY (2001) Dental care considerations of Disadvantaged and Special Care Populations 29: 108-116.
- Centers for Disease Control and Prevention. Healthy people 2010: progress reviews area 21 oral health presentations. 2014.
- Blumenshine SL, Vann WF, Gizlice Z, Lee JY (2011) Children's school performance: Impact of general and oral health. J Public Health Dent 68: 82-87.
- DiMarco MA, Huff M, Kinion E, Kendra MA (2009) The pediatric nurse practitioner’s role in reducing oral health disparities in homeless children. J Public Health Dent 23: 109-116.
- Edelstein BL, Chinn CH (2009) Update on disparities in oral health and access to dental care for america's children. Academic Pediatrics 9: 415
- Weyant RJ, Tracy SL, Anselmo T (2013) Topical fluoride for caries prevention. Journal of American Dental Association 144: 1279-1291.
- Petersson LG, Twetman S, Dahlgren H, Norlund A, Holm AK, et al. (2004) Professional fluoride varnish treatment for caries control: A systematic review of clinical trials. Acta Odontol Scand 62: 170-176.
- Tinanoff N, Reisine S (2009) Update on early childhood caries since the Surgeon General’s Report. Acad Pediatr 9: 396-403.
- Centers for Disease Control and Prevention (2011) Untreated dental caries (cavities) in children ages 2-19, United States.
- Chi D, McManus B, Carle A (2014) Caregiver burden and preventive dental care use for US children with special health care needs: A stratified analysis based on functional limitation. Matern Child Health J 18: 8828-8290.
- Weintrab JA, Ramos FG, Jue B, Shain S, Hoover CI, et al. (2006) Fluoride varnish efficacy in preventing childhood caries. J Dent Res 85: 172-176.
- Vargas CM, Ronzio CR (2002) Relationship between children's dental needs and dental care utilization: United States. Am J Public Health 92: 1816-1821.
- Clark SJ, Duong S, Fontana M (2014) Dental provider attitudes are a barrier to expanded oral health care for children ≤3 years of age. Global Pediatric Health Journal 1: 114.
- Newacheck PW, Hung YY, Park MJ, Brindis CD, Irwin CE (2003) Disparities in adolescent health and health care: Does socioeconomic status matter?. Health Serv Res 38: 1235-1252.
- Wymyslo T 2011) A report on the oral health of ohioans and their access to dental care. Ohio Department of Health.
- American Academy of Pediatrics (2011) Oral health coding fact sheet for primary care physicians.
- Sroda, R (2011) Nutrition for a healthy mouth, (4thedn) Lippincott, Williams & Wilkins Philadelphia, Pennsylvania, United States .
- Naidoo S, Myburgh N (2007) Nutrition, oral health and the young child. Matern Child Nutr 3: 312-321.
- Declerck D, Leroy R, Martens L, Lesaffre E, Garcia MJ, et al. (2008) Factors associated with prevalence and severity of caries experience in preschool children. Community Dent Oral Epidemiol 36: 168-178.
- Habibian M, Beighton D, Stevenson R, Lawson M, Roberts G (2002) Relationships between dietary behaviors, oral hygiene and mutans streptococci in dental plaque of a group of infants in Southern England. Arch Oral Biol 47: 491-498.
- Krol DM, Nedley MP (2007) Dental caries: State of the science for the most common chronic disease of childhood. Advances in Pediatrics 54: 215-239.
- Peterson SK, Stevens J (2010) Optimizing the health of infants and children: Their oral health counts. J Pediatr Nurs 25: 244-249.
- Herndon JB, Tomar SL, Lossius MN, Catalanotto FA (2011) Preventive oral health care in early childhood: Knowledge, confidence, and practices of pediatricians and family physicians in Florida. J Pediatr 157: 1018-1024.
- Griffin S, Barker L, Liang W, Li C, Albuquerque M, et al. (2014) Use of dental care and effective preventive services in preventing tooth decay among U.S. children and adolescents-medical expenditure panel survey, united states, 2003–2009 and national health and nutrition examination survey, united states, 2005-2010. Use of Selected Clinical Preventive Services to Improve the Health of Infants, Children, and Adolescents - United States 63: 54-60.
Relevant Topics
- About the Journal
- Birth Complications
- Breastfeeding
- Bronchopulmonary Dysplasia
- Feeding Disorders
- Gestational diabetes
- Neonatal Anemia
- Neonatal Breastfeeding
- Neonatal Care
- Neonatal Disease
- Neonatal Drugs
- Neonatal Health
- Neonatal Infections
- Neonatal Intensive Care
- Neonatal Seizure
- Neonatal Sepsis
- Neonatal Stroke
- Newborn Jaundice
- Newborns Screening
- Premature Infants
- Sepsis in Neonatal
- Vaccines and Immunity for Newborns
Recommended Journals
Article Tools
Article Usage
- Total views: 17140
- [From(publication date):
specialissue-2016 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 16051
- PDF downloads : 1089