Research Article Open Access
Improving Maternal Health in Rwanda: The Role of Community-Based Interventions: A Systematic Review (2005-2015)
Bucagu M*Department of Maternal, Newborn, Child and Adolescent Health, The World Health Organization, Geneva, Switzerland
- *Corresponding Author:
- Dr. Maurice Bucagu, MD, M. Med (O&G), PhD
Department of Maternal, Newborn
Child and Adolescent Health
The World Health Organization
20, Avenue Appia – CH-1211, Geneva 27, Switzerland
Tel: +41227911594
Fax: +41227911594
E-mail: bucagum@who.int
Received date: February 29, 2016; Accepted date: May 30, 2016; Published date: Jun 05, 2016
Citation: Bucagu M (2016) Improving Maternal Health in Rwanda: The Role of Community-Based Interventions: A Systematic Review (2005-2015). J Community Med Health 6:434. doi:10.4172/2161-0711.1000434
Copyright: © 2016 Bucagu M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Introduction: Rwanda has achieved Millennium Development Goal target (5A). To improve maternal health, the Government of Rwanda, in the context of its vision 2020 and related health sector reforms and policies, has been investing in the essential health interventions for reducing maternal mortality. We initiated this study aimed at exploring the role of community–based interventions.
Materials and Methods: This paper presents evidence on improvements in maternal health in Rwanda. We performed a systematic literature search in PubMed, limited to articles published between 2005 and 2015. Our literature search yielded 63 potentially relevant papers. This paper is a systematic review of 12 relevant peerreviewed articles.
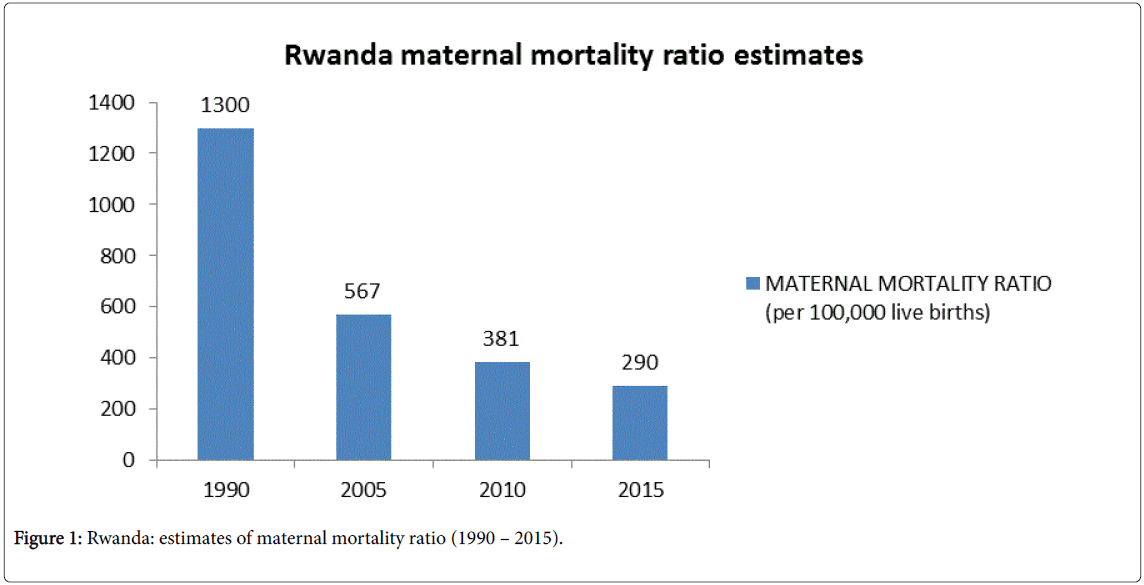
Results: The maternal mortality ratio in Rwanda has been reduced by 78% from 1,300/100,000 live births to 567/100,000 live births (2005) and 290/100,000 live births (2015), with fewer women dying from preventable causes of maternal death. The key maternal health indicators increased by two to four folds between 2005 and 2015, with the most significant changes registered in rural areas. Each village in Rwanda has a community health worker (CHW), ‘a female known as mobilizer for maternal Health’ who is responsible for community–based interventions during and after pregnancy. In 2011, a short message (SMS)-based system was set up to improve maternal and child health (MCH) using RapidSMS, a free and open–source framework, providing great opportunities for community health workers to contribute to implementing essential maternal health interventions, through communication. To achieve Millennium Development Goal 5A target, Rwanda has moved from ‘home birth’ to ‘facility–based childbirth’ policy, supported by innovative health sector reforms for the last two decades. Community health workers played a critical role in linking up communities to the health facilities and in providing relevant support for health promotion, maternal health service delivery and referral system, family planning as well as data collection for health system management.
Keywords
Rwanda; Maternal health; Community health workers; Interventions
Introduction
Rwanda has achieved Millennium Development Goal target (5A), based on the reduction of the maternal mortality ratio (MMR) by 78% between 1990 (1300/100,000 live births) and 2015 (290/100,000 live births) [1]. To improve maternal health, the Government of Rwanda, in the context of its vision 2020 and related health sector reforms and policies, has been investing in the essential health interventions for reducing maternal mortality, including family planning and access to other reproductive health services, skilled care during pregnancy and childbirth (including emergency obstetric care), post-partum care as well as post–abortion care, with special efforts to scaling up key maternal health services from 2005 to 2015 [2,3].
Since 2007, a reform was implemented nationwide with the goal of optimizing the role of community health workers in improving access to the maternal health interventions in Rwanda [4]. Several studies and reports from Governments, United Nations agencies, Nongovernmental organizations and global partners support the role of Community Health Workers (CHWs) in increasing access to primary health care interventions and services in low and middle income countries. However, the competencies of CHWs, their scope of work, and integration in national health systems vary widely and largely depend on country context [5]. Based on this background, we initiated this study aimed at exploring the role of community–based interventions in improving maternal health in the specific millennium development goals related context of Rwanda.
Materials and Methods
This paper presents evidence on improvements in maternal health in Rwanda from the literature published between 2005 and 2015. We identified the community–based interventions that we believe have contributed to expanding essential maternal health interventions in Rwanda.
We performed a systematic literature search in PubMed, limited to articles published between 2005 and 2015. We developed a comprehensive search strategy to identify studies matching the following terms: ("Rwanda"[MeSH Terms] OR "Rwanda"[All Fields]) AND ("community health planning"[MeSH Terms] OR ("community"[All Fields] AND "health"[All Fields] AND "planning"[All Fields]) OR "community health planning"[All Fields] OR ("community"[All Fields] AND "health"[All Fields] AND "system"[All Fields]) OR "community health system"[All Fields]).
Although grey literature on these topics exists, we limited the formal literature review to peer-reviewed publications, with no language restriction. The searches in PubMed were last performed on February 15, 2016.
We reviewed the papers returned by the search terms for relevance by screening the title, abstract and medical subject headings (MeSH). The full-text paper was retrieved for further review. Our literature search yielded 63 potentially relevant papers; the duplicates from multiple different search combinations are excluded from this number. On the basis of their titles, abstracts and MeSH terms, 12 full-text articles were selected to be retrieved for in-depth review. The references of those articles were manually tracked.
Documents available from WHO website provided other sources of evidence. These include estimates of global maternal mortality and relevant guidelines.
We also extracted data on maternal health coverage indicators from the Rwanda Demographic Health Surveys (2005, 2010 and 2015). The reports provide values for three five-year periods [6,7].
Focusing on the public sector and national results, we examined trends in four indicators: antenatal care; skilled provider assisted births; births in health facilities and contraceptive prevalence (mix modern methods).
To describe the trends in the selected indicators, we used the weighted average which refers to the percent distribution of live births in the five years preceding the survey by service provider (for antenatal care–4 visits plus, skilled provider assisted birth) and by place of delivery (for births in health facilities); and to the percentage of all surveyed women, currently married and sexually active unmarried women who have ever used any modern contraceptive method (for contraceptive prevalence).
This paper is a systematic review of 12 relevant peer-reviewed articles that are displayed in Table 1.
| Study | Study design and size | Study objectives | Conclusions |
|---|---|---|---|
| Bucagu et al.[2] | Systematic review (2000-2010). National data (Demographic and health surveys 2000, 2005, 2010). | To examine the extent to which more women in Rwanda began using delivery care with a skilled attendant, institutional delivery, including emergency obstetric care, and modern contraceptive methods. | Since 2000, more women in Rwanda have begun to receive maternity care with a skilled attendant and in a facility. More women have also begun to use modern family planning methods, particularly in rural settings where most poor and vulnerable women live. The primary factors in these improvements have been increasing the health workforce and their skills, performance-based financing, community–based health insurance and good governance. |
| Condo et al.[4] | Cross-sectional descriptive study. Focus group discussions (FGD) were used to collect qualitative information regarding educational background, knowledge and practices of CHWs and the benefits of community–based care as perceived by CHWs and household beneficiaries. A random sample of 108 CHWs and 36 beneficiaries was selected in 3 districts according to their food security level (low, middle and high). |
To assess the capacity of CHWs and the factors affecting the efficiency and effectiveness of the CHW programme. | CHWs were found to be closely involved in the community and widely respected by the beneficiaries. Rwanda’s community performance – based financing (cPBF) was an important incentive; but CHWs were also strongly motivated by community respect. The key challenges identified were an overwhelming workload, irregular trainings and lack of sufficient supervision. |
| Binagwaho et al. [8] | Debate | To discuss key causes and consequences of loss of early developmental potential and how this relates to human rights legal framework in Rwanda. | Realization of the human rights to health, education and economic prosperity requires and benefits from attention to the period of ECD, as early childhood has the potential to be an opportunity for expedient intervention or the first case of human rights neglect in a lifetime of rights violations. Efforts to improve ECD services and outcomes at the population level require multisector collaboration, at the highest echelons of government, as well as local education and participation at the community level. |
| Ingabire et al.[10] | ‘Open space’ participatory approach, as part of multidisciplinary horizontal research, involving medical, entomological, economical as well as behavioural components with the aim to empower communities. Sixty-two (62) and eighty-two (82) participants for two ‘open space’ sessions, from a population of 19,606. |
To explore and brainstorm community perceptions of the malaria problem in Rwanda – Ruhuha sector, their willingness to participate in a malaria elimination program and to determine the key actions to be taken by various stakeholders. | ‘Open space’ approach yields interesting findings as other participatory approaches and can serve as a platform to gather more information from various members of the community, to formulate measures to be taken and create motivation for key stakeholders to be involved in a health program, all within a short period of time. |
| Chin-Quee et al.[11] | 910 CHWs (7 health centres /Rusizi district) and 582 CHWs (7 health centres / Kicukiro district); to be compared with 1553 CHWs (13 health centres / Kayonza district) and 874 CHWs (12 health centres / Gasabo district). | The study combined perception and objective measures of workload to examine their effect on quality of services, worker performance, and job and client satisfaction. | Over 90% of CHWs reported manageability, job satisfaction, and motivation to perform their jobs. Clients were highly satisfied with CHW services and most stated preference for future services from CHWs. Accordingly, the initiative was scaled up in all 30 districts in the country. |
| McKenna et al.[12] | Qualitative case study, through in-depth interviews. 27 service providers and 19 policy makers and program implementers. |
To identify potential barriers and opportunities related to the introduction of a longer-acting injectable (LAI) at the policy, health system, clinic and client-levels. | Successful introduction of a potential longer-acting injectable may be enhanced by considering broader systemic issues, including managing cost to the health system and users, expanding access through community-based distribution and training providers on the latest service delivery guidelines. |
| Ngabo et al.[13] | Descriptive: RapidSMS-MCH system. 432 CHWs dealing with maternal and newborn health and implementing RapidSMS-MCH system design in Musanze district, with a population of 347,692 (Rwanda). |
To describe the design and implementation of a mobile phone-based communication system aimed at monitoring pregnancy and reducing the three delays in communication associated with maternal and newborn deaths in Rwanda. | RapidSMS-MCH demonstrates that mobile phone offers an opportunity to overcome barriers that limit access to quality maternal and child health. Mobile phones can help women, their families and local health workers to seek timely, appropriate medical help for an obstetric and newborn emergency by reducing the time that elapses between a health crisis and care. |
| Manzi et al.[14] | Cross-sectional study. 6,325 women age 15-49 (2010 Rwanda DHS). |
To understand factors associated with delayed antenatal care (ANC) visits in Rwanda. | The analysis revealed potential barriers to ANC service utilization. Distance to health facility remains a major constraint which suggests a great need of infrastructure and decentralization of maternal ANC to health posts and dispensaries. Interventions such as universal health insurance coverage, family planning and community health system could be part of effective strategies to address delays in ANC. |
| Mitsunaga et al. [15] | CHW data quality accuracy assessment. Cluster-lot quality assurance sampling was used to sample six CHWs per cell and six households per CHW; 204 CHW registers and 1224 households were assessed for accuracy across 34 cells in Southern Kayonza. |
To measure CHW data accuracy, defined as agreement between households registers compared to household member interview and client records in one district in Eastern province, Rwanda. | Point estimates across health centres ranged from 79 to 100% for individual indicators and 61 to 72% for the composite indicator. Overall, accuracy was largely ‘good’ across cells, with varying results by indicator. |
| Mitsunaga et al.[16] | Descriptive: CHW data Quality assessment. Lot quality assurance sampling, in 175 villages, representing the work of 463 CHWs (eight health centres / Southern Kayonza district). |
To assess CHW data quality. | While the results identified gaps in the current data quality, the assessment also identified opportunities for strengthening the data to ensure suitable levels of quality for use in management and evaluation. Appropriate interventions may address relevant factors at health units identified with poor data quality. |
| Munyaneza et al.[17] | Descriptive study on the use of community health workers’ (CHW) supervisors to map villages in a mountainous rural district of Northern Rwanda. A low literacy and skills-focused training in the local language (Kinyarwanda) to train 86 CHW supervisors and 25 nurses in charge of community health to collect the geographic coordinates of the villages using global positioning systems (GPS). |
To demonstrate the usefulness of the work, drinking water sources (DWSs) from data collected by CHW supervisors. DWSs were categorized as safe versus unsafe using WHO definitions. | Existing national CHW system can leveraged to inexpensively and rapidly map villages even in mountainous rural areas. These data are important to provide managers and decision makers with local – level GIS data to better target and evaluate interventions. |
| Sayinzoga et al.[18] | Retrospective cohort study. Nationwide facility-based study; 987 audited cases of maternal death. |
To present the results of 5 years of implementing health-based maternal death audits in Rwanda, showing causes of deaths, factors that have contributed to death, and recommendations for quality improvements in maternal care. | 987 audited cases representing 93.1% of all maternal deaths reported through the national management information system over the 5-year period. Almost 3 quarters of the deaths (71.6%) occurred at district hospitals. In 44.9% of these cases, death occurred in the postpartum period. Seventy per cent were due to direct causes, with post-partum haemorrhage as the leading cause (22.7%), followed by obstructed labour (12.3%). Indirect causes accounted for 25.7% of maternal deaths, with malaria as the leading cause (7.5%). Health system failures were identified as the main responsible factor for the majority of cases (61.0%); in 30.3% of the cases, the main factor was patient or community related. |
Table 1: Studies reviewed on the role of community-based interventions in improving maternal health in Rwanda (2005-2015).
Results and Discussion
Millennium development goal 5A target achieved
The maternal mortality ratio in Rwanda has been reduced by 78% from 1,300/100,000 live births to 567/100,000 live births (2005) and 290/100,000 live births (2015), with fewer women dying from preventable causes of maternal death, as Figure 1 shows [1].
The key maternal health indicators (Table 2), including four antenatal care visits, skilled provider assisted birth rate, institutional birth rate (including emergency obstetric care), as well as contraceptive prevalence rate, all increased by two to four folds between 2005 and 2015, with the most significant changes registered in rural areas, where majority of the Rwandan population in need live [6,7].
| Indicator | Scope of survey/Residence | DHS 2005 (n=11,321) |
DHS 2010 (n=13,790) |
DHS 2015 (n=12793) |
|---|---|---|---|---|
| Antenatal care (4 visits +) |
Urban (%) | 17.6 | 40.4 | 44.3 |
| Rural (%) | 12.6 | 34.7 | 43.9 | |
| Weighted average (%) | 13.3 | 35.4 | 44.1 | |
| Skilled provider assisted birth | Urban (%) | 63.1 | 82.4 | 96.8 |
| Rural (%) | 34.6 | 67.2 | 89.4 | |
| Weighted average (%) | 39 | 69 | 90.7 | |
| Births in health facilities | Urban (%) | 54.9 | 82 | 96.8 |
| Rural (%) | 23.8 | 67.1 | 89.4 | |
| Weighted average (%) | 28 | 68.9 | 90.7 | |
| Contraceptive prevalence (modern methods) | Urban (%) | 21.2 | 47 | 51.1 |
| Rural (%) | 8.6 | 44.9 | 46.7 | |
| Weighted average (%) | 10 | 45.1 | 47.5 |
Table 2: Trends of selected coverage indicators for maternal health in Rwanda (2005 – 2015).
Previous studies have explored the primary factors in these improvements. Those included increased health workforce and their skills (including community health workers), performance-based financing, community-based health insurance and good governance [2].
Community–based interventions for maternal health in Rwanda
The government of Rwanda, in the context of the post-1994 genocide against the Tutsi, embarked on strengthening the existing community–based interventions with the goal of using community health workers (CHWs) to complement the limited capacity of the health workforce, particularly for delivery of maternal and child health services. In 2007, the Ministry of Health initiated policy reforms of the national community health program, which was set up in 1995. The new guidance provided a minimum of 6 years of primary education as eligibility criteria for community health workers at village level. In 2014, Condo et al. reported a number 3 CHWs per village, including two general CHWs (a female and a male), responsible for community health, health education, nutrition, HIV prevention, and a CHW, known as ‘Mobilizer for Maternal Health’, a female responsible for community–based interventions during and after pregnancy, as well as for child care. This study showed that CHWs play key roles in linking the country’s primary health care system to the community, and mitigating the health professional shortage, by providing basic care. Based on lessons learned in the area of health financing, the government of Rwanda has implemented a community performance – based financing as a response to addressing issues of motivation and retention of CHWs who are organized in cooperatives to ensure accountability and income generation [2,4,8].
The network of 45,011 CHWs is managed by the Rwanda ministry of health. CHWs are attached to health centres which provide training, supportive supervision, commodities and supplies. In line with WHO recommendations on task shifting [9], CHWs are specifically tasked with providing community-based integrated management of child illness; growth monitoring of infants and children; family planning counselling; referral and condom provision; rapid tests for malaria diagnosis; directly observed treatment of tuberculosis; nutrition counselling; counselling on sanitation and home hygiene; Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome (HIV/AIDS) prevention, including male involvement as a strategy for prevention of mother to child transmission of HIV and support for people living with HIV/AIDS [4,10]. In this context, Chin – Quee at al., study findings strongly suggested that adding contraceptive pill and injectable re-supply would not adversely affect quality or the relationships between CHWs and clients. Accordingly, the initiative was scaled up nationwide [11]. Similarly McKenna et al., from their study findings, had previously concluded that majority of policy makers and programme implementers in Rwanda were supportive of letting community health workers provide a longer-acting injectable contraceptive [12].
In 2011, Rwanda set up a short message (SMS)-based system to improve maternal and child health (MCH) using RapidSMS, a free and open–source framework. This was customized to allow interactive communication between a community health worker (CHW) involved in the follow up of mothers and babies at community level, a national centralized database, the health facility, and in case of emergency, the ambulance driver. The RapidSMS-MCH system was piloted in Musanze district, Northern Province of Rwanda, over a period of 12 months. A total of 432 CHWs were trained and equipped with mobile phones. A total of 35,734 SMS were sent by the CHWs over a period one year, a total of 11,502 pregnancies were monitored. A 20% increase in facility–based childbirth was reported in the district for the pilot phase. The RapidSMS-MCH has provided opportunities for community health workers to contribute to implementing essential interventions for improving access to antenatal care, emergency obstetric and newborn care [13,14].
The Rwanda ministry of health has also established a standardized community health information system that makes CHW data available at sub-national and national levels. In this context, a data quality assessment system (DSA) to ensure quality data for program management, evaluation and quality assurance of CHW activities was piloted in Southern Kayonza. Mitsunaga et al. reported an overall ‘largely good’ accuracy of the DSA across lowest administrative units (known as cells), with varying results by indicator. From their findings, there is potential for the routinely-collected data by CHWs to be meaningful inputs for strengthening the community health program management [15,16].
The community health workers program, as a bridge between the primary health care system and communities, is a priority for Rwanda. Its major limitation has been the insufficient capacity of the national health system to provide CHWs with required competencies and skills for effective implementation of essential interventions for maternal health and to ensure it is sustainable.
Existing studies have documented the role of a similar model of disease and care management. Ciccone et al. [17,18], through ‘the Project Leonardo’ findings, have demonstrated feasibility and effectiveness of the specific system with care managers (trained nurses) providing support to the general practitioners (GPs) and specialists in the management of patients with cardiovascular diseases, diabetes, heart failure (chronic conditions). Those care managers worked directly with individual patients to help monitor their conditions, and to provide the necessary information and advice for better compliance with care recommendations. This model resulted in tangible improvements in the clinical parameters of the patients and better control of their conditions.
To achieve MDG 5, Rwanda has moved from ‘home birth’ to ‘facility–based childbirth’ policy, supported by innovative health sector reforms that were implemented by the government of Rwanda and its partners for the last two decades. Those reforms included namely decentralization of health services and community participation, improved financial access to health care through a 'Community-Based Health Insurance' scheme; health systems strengthening approach. In this context, community health workers played a critical role in linking up individuals, families and communities to the health facilities and in providing relevant support for health promotion, maternal health service delivery and referral system, family planning, HIV prevention as well as data collection for health system management [19-21].
References
- World Health Organization (2015) Trends in maternal mortality 1990 to 2015. Estimates by WHO, UNICEF, UNFPA, the World Bank Group and the United Nations Population Division.
- Bucagu M, Kagubare J, Basinga P, Ngabo F, Timmons KB, et al. (2012) Impact of health systems strengthening on coverage of maternal health services in Rwanda, 2000-2010: a systematic review. Reprod Health Matters 20: 50-61.
- World Health Organization (2015) Success factors for women’s and children’s health: Rwanda.
- Condo J, Mugeni C, Naughton B, Hall K, Tuazon MA, et al. (2014) Rwanda’s evolving community health worker system: a qualitative assessment of client and provider perspectives. Hum Resour Health 12: 71.
- World Health Organization (2015) Strengthening the capacity of community health workers to deliver care for sexual, reproductive, maternal, child and adolescent health.
- Rwanda National Institute of Statistics, Ministry of Health and ORC Macro Calverton, Maryland USA (2012) Rwanda Demographic and Health Survey 2010: final report.
- Rwanda National Institute of Statistics, Ministry of Health and ORC Macro Calverton, Maryland USA (2015) Rwanda Demographic and Health Survey 2014-2015: Key indicators.
- Binagwaho A, Scott KW, Harward SH (2016) Early childhood development in Rwanda: a policy analysis of the human rights legal framework. BMC Int Health Hum Rights 16: 1.
- World Health Organization (2012) Optimizing health worker roles to improve access to key maternal and newborn health interventions through task shifting. WHO recommendations.
- Ingabire MV, Alaii J, Hakizimana E, Kateera F, Muhimuzi D, et al. (2014) Community mobilization for malaria elimination: application of an open space methodology in Ruhuha sector, Rwanda. Malar J 13: 167.
- Chin-Quee D, Mugeni C, Nkunda D, Uwizeye MR, Stockton LL, et al. (2016) Balancing workload, motivation and job satisfaction in Rwanda: assessing the effect of adding family planning service provision to community health worker duties. Reproductive Health 13: 2.
- McKenna K, Arcara J, Rademacher KH, Mackenzie, Ngabo F, et al. (2014) Policy and programmatic considerations for introducing a longer – acting injectable contraceptive: perspectives of stakeholders from Kenya and Rwanda. Glob Health SciPract 2: 459-471.
- Ngabo F, Nguimfack, Nwaigwe F, Mugeni C, Muhoza D, et al. (2012) Designing and implementing an innovative SMS-based alert system (RapidSMS-MCH) to monitor pregnancy and reduce maternal and child deaths in Rwanda. Pan Afr Med J13: 31.
- Manzi A, Munyaneza F, Mujawase F, Banamwana L, Sayinzoga F, et al. (2014) Assessing predictors of delayed antenatal care visits in Rwanda: a secondary analysis of Rwanda demographic and health survey 2010. BMC Pregnancy Childbirth 14: 290.
- Mitsunaga T, Hedt-Gauthier B, Ngizwenayo E, Farmer DB, Karamaga A, et al. (2013) Utilizing community health worker data for program management and evaluation: systems for data quality assessments and baseline results from Rwanda. SocSci Med 85: 87-92.
- Mitsunaga T, Hedt-Gauthier B, Ngizwenayo E, Farmer DB, Gaju E, et al. (2015) Data for program management: an accuracy assessment of data collected in households registers by community health workers in southern Kayonza, Rwanda. J Community Health 40: 625-632.
- Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, et al. (2010) Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag 6: 297-305.
- Cecere A, Scicchitano P, Zito A, Sassara M, Bux F, et al. (2014) Role of care manager in chronic cardiovascular diseases. Ann Gerontol Geriatric Res 1: 1005.
- Munyaneza F, Hirschhorn LR, Amoroso CL, Nyirazinyoye L, Birru E, et al. (2014) Leveraging community health worker system to map montainous rural district in low resource setting: a low-cost approach to expand use of geographic information systems for public health.Int J Health Geogr 13: 49.
- Sayinzoga F, Bijlmakers L, van Dillen J, Mivumbi V, Ngabo F, et al. (2016) Maternal mortality audit in Rwanda 2009 – 2013: a nationwide facility – based retrospective cohort study. BMJ Open6: e009734.
- World Health Organization (2013) Counselling for maternal and newborn health care. A handbook for building skills.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 16343
- [From(publication date):
June-2016 - Jul 17, 2025] - Breakdown by view type
- HTML page views : 15039
- PDF downloads : 1304