Case Report Open Access
Improving Facial Esthetics for a Young Patient with Class III Malocclusion and Retention of Maxillary Central Incisors due to Supernumerary Teeth
Benkaddour A1*, Bahoum A1, El Mohtarim B2, Benyahia H1 and Zaoui F3
1Department of Dento Facial Orthopedics, Military Hospital of Instruction Mohamed V in Rabat, Morroco
2Chief of Odontology Department at the Military Hospital of Instruction Mohamed V in Rabat, Morroco
3Chief of Orthodontics Department , Faculty of Dentistry, University Mohamed V, Rabat, Morroco
- *Corresponding Author:
- Benkaddour A
Assistant Professor, Department of Dento Facial Orthopedics
Faculty of Dentistry, University Mohamed V, Rabat, Morroco
Tel: 00212668158289
E-mail: asmae-benkaddour@hotmail.fr
Received: November 06, 2015; Accepted: January 27, 2016; Published: January 30, 2016
Citation: Benkaddour A, Bahoum A, El Mohtarim B, Benyahia H, Zaoui F (2016) Improving Facial Esthetics for a Young Patient with Class III Malocclusion and Retention of Maxillary Central Incisors Due to Supernumerary Teeth. Dial Clin Pract 1:103. doi:10.4172/2572-4835.1000103
Copyright: © 2016 Benkaddour A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Dental Science and Medicine
Abstract
Supernumerary teeth are more frequently located in the premaxillary region. Mesiodentesare the most common supernumerary teeth, occurring in 0.15% to 1.9% of the population. They are frequently diagnosed in a random radiograph, or after clinical symptoms appear. The majority of the complications consist of retention or impaction, delayed or ectopic eruption of the permanent incisors. The present case report describes the clinical management of two impacted supernumerary teeth, which impeded the eruption of the maxillary central incisors in a 9-year-old patient with class III malocclusion, who was referred to our department of dento facial orthopedics with the chief complaint of his unsightly smile. A multidisciplinary treatment approach was planned, including the surgical removal of the supernumerary teeth and the orthodontic correction of the malocclusion and the unerupted permanent maxillary central incisors. Combined surgical and orthodontic treatment resulted in an aesthetically pleasant and balanced profile and occlusion. Thus, early multidisciplinary treatment is required for greater hard and soft tissue preservation, but also to have an immediate positive esthetic impact and redirect the unfavorable maxillary growth.
Keywords
Facial esthetics class III; Impacted incisors; Orthodontic and surgical extrusion; Supernumerary teeth
Introduction
Impaction of maxillary permanent incisors is not a frequent case in dental practice, but its treatment is challenging because of their impact on facial esthetics [1].
supernumerary teeth (hyperdontia) is a state which can be defined as any tooth substance in excess of the usual configuration of the normal number of deciduous or permanent teeth, [2] they constitute the main cause of the impaction of upper incisors. 56-60% of premaxillary supernumerary teeth cause impaction of permanent incisors [3]. Although several theories have been submitted to explain their development, the precise etiology of supernumerary teeth is not clearly understood [4]. But the common suggestion about their etiology is considered to develop as a result of horizontal proliferation or a hyperactivity of the dental lamina [5].
The prevalence of hyperdontia is reportedly between 0.15% and 3.9% [3-7]. Extra teeth may be present in both the permanent and the primary dentitions but are 5 times less frequent in the primary dentition [8-10]. A mesiodens is a supernumerary tooth located in the maxillary central incisor region; the overall prevalence of mesiodentes is between 0.15% and 1.9% [9-11]. Mesiodens can occur individually or as multiples (mesiodentes), may appear unilaterally or bilaterally, and often do not erupt [11]. Only 25% of all mesiodentes spontaneously erupt into the oral cavity [12].
After removal of the obstacle (supernumerary teeth) from the path of eruption, an impacted tooth, either erupt spontaneously if it has conserved its eruptive force (75% of cases), or else, an orthodontic force is required to bring the tooth in the normal position [1,12-14].
This case report describes the management of a bilateral central incisor impaction, caused by two supernumerary teeth in the path of their eruption, for a young patient with dental and skeletal class III malocclusion, and the improvement of his facial esthetics both by surgical and orthodontic approach.
Case Report
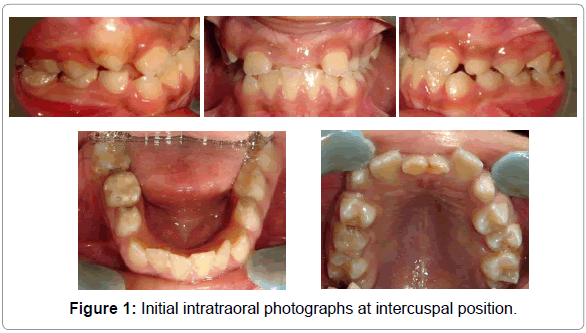
A 9-years-old boy was referred to our department of dento facial orthopedics, at the center of dental consultations and treatments in Rabat, with the chief complaint of his smile, which is made unattractive by non-eruption of both permanent maxillary central incisors and persistenceof deciduous ones in crossbite. Patient was asymptomatic, and his past dental, medical and family history was non-contributory. Intraoral examination revealed that the patient was in mixed dentition; the central permanent incisors (11) and (12) had not erupted into the oral cavity, with persistence of central deciduous ones (51) and (61) and the lateral permanent incisors (12) and (22) were present. There was no sign of inflammation, pain or infection and surrounding mucosa was normal. Occlusally, he had a more pronounced canine and molar class III relationship on the right side than the left side (Figure 1).
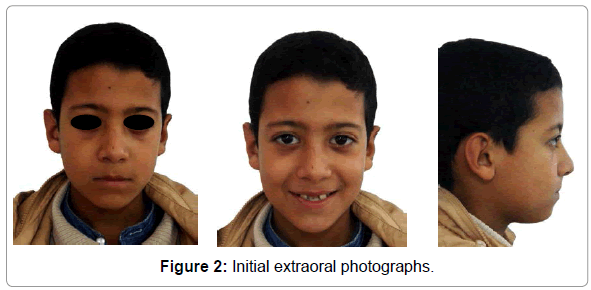
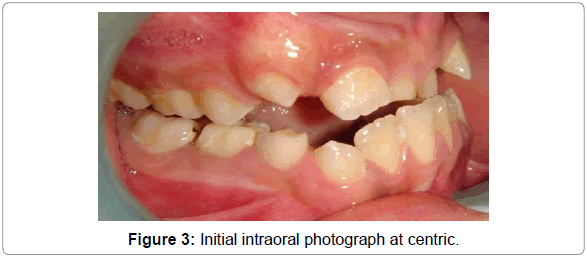
According to the exobuccal examination, frontal analysis showed a constantly tired-looking face, an upper lip with poor volume and inadequate lip vermilion. The profile analysis showed a Class III aspect consequent to maxillary and zygomatic deficiencies; the profile was flat, with an open nasolabial angle and a lower procheilie; however, the chin-neck line was good, and the chin appearance was satisfactory. The smile was effectively rendered unattractive by the absence of both maxillary central incisors (Figure 2). At centric relation, an edge-to-edge incisor relationship was observed, which improved the prognosis; the presence of the anterior crossbite is observed as a result of a mandibularforward displacement, due to abnormal occlusal contact (Figure 3).
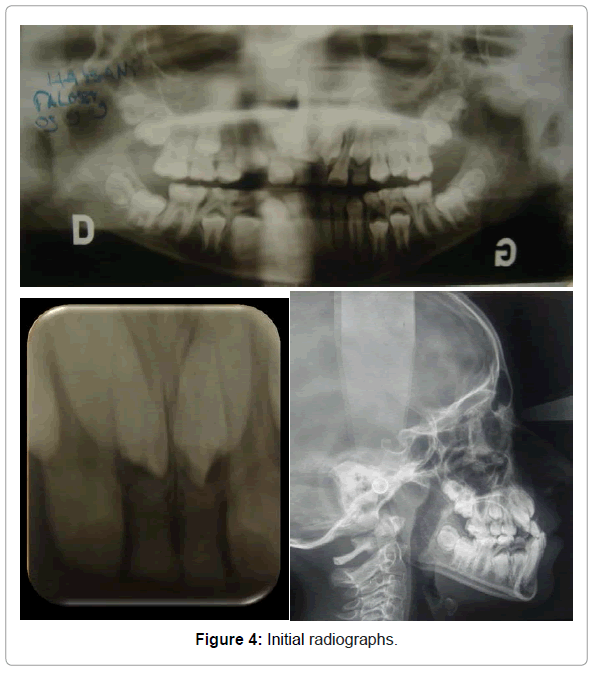
Radiographic examination, show the impaction of the maxillary central incisors on mesially inclined position, and the presence of two supernumerary teeth in their eruption path. It was founded that the supernumerary teeth were on palatal position relative to permanent incisors, panoramic radiograph showed also the presence of all permanent teeth either already erupted or at the several stages of formation, in mixed dentition (Figure 4).
The patient’s maxillomandibular relationship was deficient, with a maxillary retrusion, he was hyper divergent and had lower incisive protrusion (Table 1).
| SNA | 80 |
| SNB | 79,5 |
| ANB | 0,5 |
| I/to NA | -- |
| i/ to NB | 8mm/27° |
| Po to NB | -2 |
| GoGnSN | 40 |
| FMA | 29 |
| IMPA | 86 |
| AoBo | -3 |
Table 1: Cephalometric analysis before treatment.
The treatment objectives were positioning the maxillary central incisors in the maxillary arch by surgical repositioning and orthodontic traction and getting a normal overjet and overbite, to prevent the mandible proglissment and thereafter, to avoid worsening of the Class III skeletal relationship. Correcting the mandibular crowding and the Class III dental relationship. This would significantly improve the patient’s smile and soft-tissue profile; this was his chief goal.
In accordance with the patient’s parents, and in collaboration with the pediatric dentist, the treatment plan was established as follows:
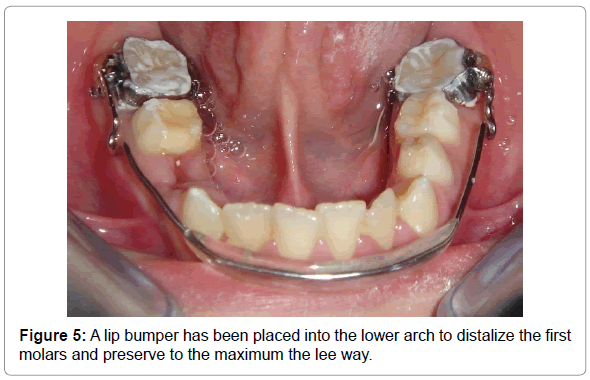
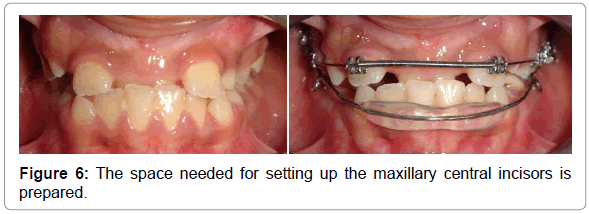
First we decided to set up a lip bumper into the lower arch to distalize the first molars and preserve to the maximum the lee way (Figure 5). At the same time, bonding the maxillary teeth and programming the surgical step once the arch alignment has been progressed to a stable arch wire, and the space needed for setting up the maxillary central incisors has been prepared (Figure 6).
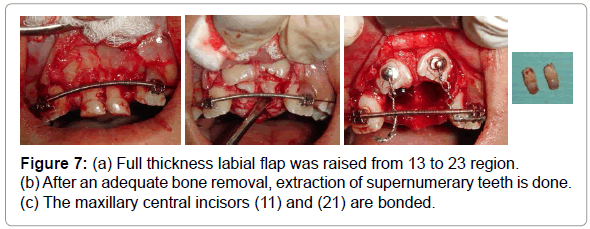
After proper local anesthesia, full thickness labial flap was raised from 13 to 23 region. The crown of 11 and 21 were seen under a thin cover of labial cortical bone, their respective supernumerary teeth were seen after extraction of deciduous incisors. After an adequate bone removal, extraction of supernumerary teeth were done and the incisors (11 and 21) were bonded (Figure 7). At-last the mucoperiosteal flap was repositioned apically, suture was placed and instructions were given to not disturb the surgical filed till healing.
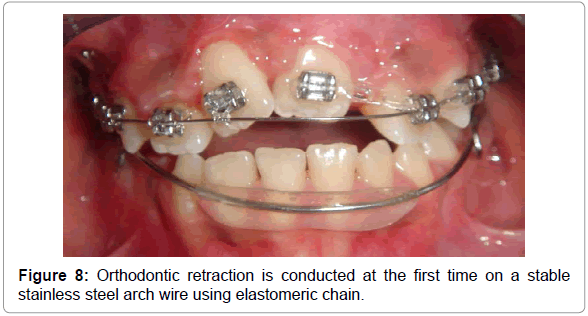
Orthodontic retraction was started the same day of surgery; it was conducted at the first time on a heavy stainless steel arch wire (17×25) using elastomeric chainlets (Figure 8). The stable arch wire helps maintain the integrity of the maxillary arch and prevent intrusion or canting of the maxillary teeth as the impacted incisor is erupted. The elastomeric chain lets has been tied from the arch wire to the bonded bracket, allowing the tooth to be erupted by the application of light forces (very light force at about 60-90 g), which avoids sequelae such as root resorption, ankylosis or devitalization.
Once the incisors have approached their sites of eruption, they were ligated directly into the arch wire and alignment was done with the help of a 0.014 mm NiTi arch wire (Figure 9).
The alignment and the leveling of the lower arch has completely depends on the lee-way associated with a slight stripping of the lower incisors. Occlusal Class III has been corrected using intermaxillary elastics of class III carried on heavy rectangular stainless steel arch wires (19×25).
The patient’s orthodontic treatment lasted 30 months, the central incisors respond positively on pulp testing. A canine to canine bonded retention in the mandible and a thermoformed splint in the maxilla have been placed.
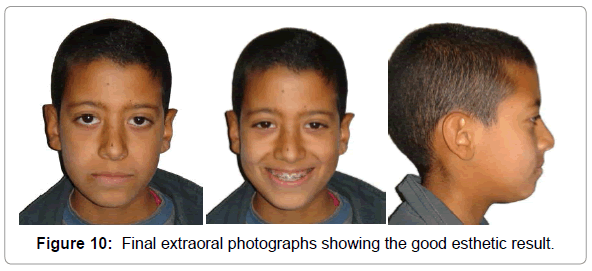
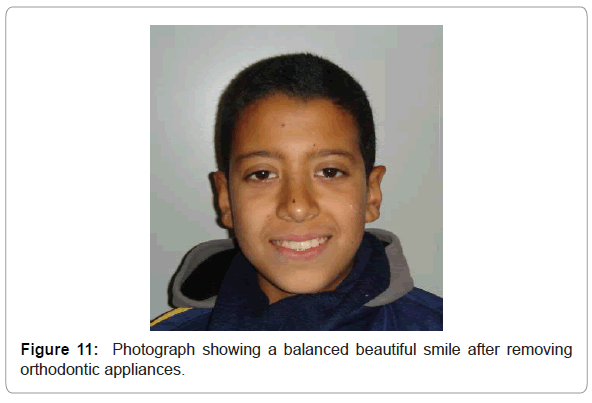
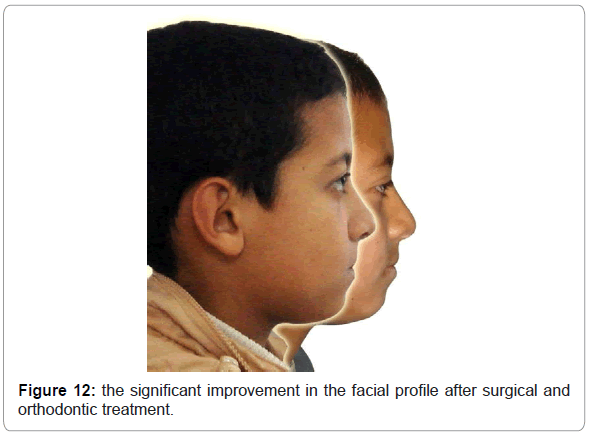
After the orthodontic correction, patient and his parents were very satisfied of the final esthetic result. The smile is made more harmoniousand balanced (Figures 10 and 11) and the most important treatment outcome, was the significant improvement in the facial profile (Figure 12).
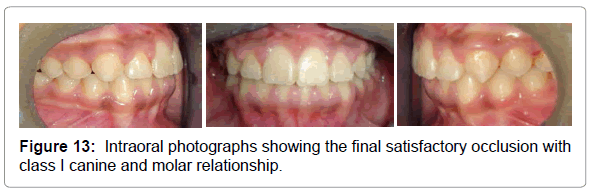
Final occlusion was adequate, with good alignment of the teeth and Class I canine and molar relationships on right and left sides. A positive overjet and overbite were also established, to ensure satisfactory, healthy and physiological functioning of the stomatognathic system and subsequently preserve a long-term stability (Figure 13).
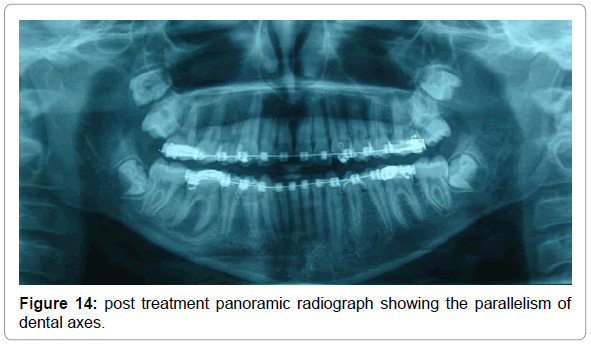
On post treatment panoramic radiograph, we notice the parallelism dental axes; persistent root proximities have been rectified before removal of the orthodontic appliances (Figure 14).
The patient was sent to the pediatric dentistry department for proper management of the 36 which presents a periapical lesion.
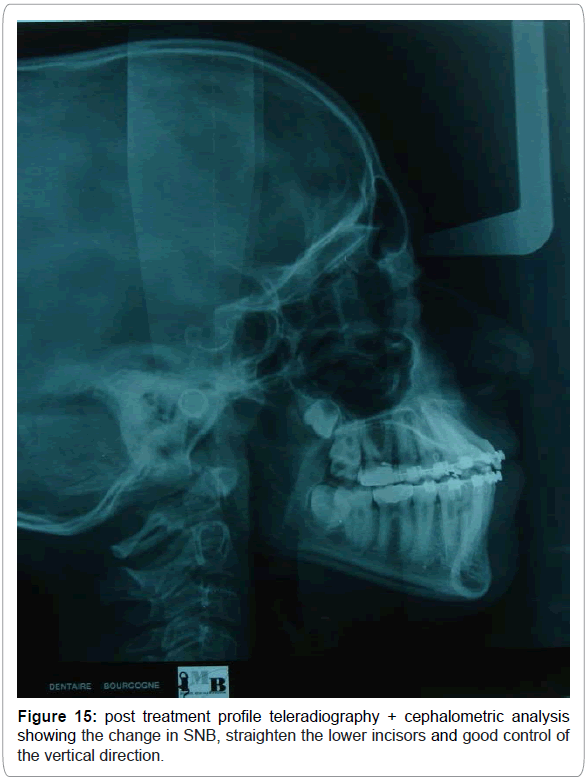
Cephalometric analysis showed a change in SNB ( from 79.5 ° to 78 ° ) which is due to repositioning of the mandible, straighten the lower incisors (from 8 mm, 27° to 4 mm, 24°), and good control of the vertical direction (Figure 15) (Table 2).
| SNA | 80 | 80 |
| SNB | 79,5 | 78 |
| ANB | 0,5 | 2 |
| I/to NA | -- | 7mm/30° |
| i/ to NB | 8mm/27° | 7mm/24° |
| Po to NB | -2 | -1 |
| GoGnSN | 40 | 40 |
| FMA | 29 | 29 |
| IMPA | 86 | 85 |
| AoBo | -3 | -1 |
Table 2: Post treatment profile teleradiography + cephalometric analysis showing the change in SNB, straighten the lower incisors and good control of the vertical direction.
Discussion
Impaction defines a tooth that cannot or will not erupt into its normal functional position in time [12,15]. The possible reasons for failure of eruption may be the lack of space, malformation due to early trauma, mechanical obstruction such as a supernumerary tooth, odontoma, other odontogenic tumors, cysts or scar tissue due to early loss of primary tooth [16]. In the presented case, supernumerary teeth were associated with unerupted maxillary central incisors. This has been described as the obvious causative factor of the skeletal deficiency at the maxillary region, which has been reflected in the facial soft tissues, causing an unfavorable esthetic impact that affected the patient’s selfesteem.
There was no syndrome or birth defect associated with this reported case. The probable causal factors were supernumerary teeth and angulations of teeth germs.
The literature reports that 80% to 90% of all supernumerary teeth occur in the maxilla [17-19]. Half are found in the anterior region [18,19]. Onethird of all patients with a mesiodens also have other supernumerary teeth; however, some patients present with mesiodentes in conjunction with congenitally missing teeth [20,21]. Mesiodentes are frequently associated with various craniofacial anomalies, including cleft lip and palate, Gardner’s syndrome and cleidocranial dysostosis [12,22].
Mesiodentes can be classified on the basis of their occurrence in the permanent dentition (rudimentary mesiodentes) or the primary dentition (supplementary mesiodentes) and according to their morphology (conical, tuberculate or molariform) [18,23]. Enamel pearls, although much smaller than and developmentally distinct from mesiodentes, may also be sufficient to impede eruption of the permanent teeth [24].
In this case report, supernumerary teeth showed characteristics of tuberculate mesiodentes, they were barrel-shaped, with several tubercles or cusps, and have incomplete or abnormal root formation. Tuberculate mesiodentes rarely erupt themselves but rather delay eruption of the permanent incisors [18,23]. They can develop unilaterally or bilaterally and usually occupy a more palatal position [12,19,25].
Methods of management of crowding or impaction due to supernumerary are; remove super-numeracy teeth or tooth only, remove supernumerary teeth and bone overlying impacted teeth, incision of fibrous tissue over the alveolar ridge to promote the eruption with or without orthodontic traction [9]. Surgical exposures of impacted incisors or surgical repositioning have been used to bring impacted teeth into occlusion [1,10,11].
We have decided on surgical exposures of impacted incisors and orthodontic extrusion for our patient, for lack of the eruptive forces, because the roots of both central incisors were almost completed at the time of surgery.
The disadvantage of the combined surgical and orthodontic therapy is required a longer treatment period and some complication including ankylosis, non-vital pulps and root resorptions may be encountered. When an extensive amount of bone is removed or an open approach method is used to expose the impacted teeth, surgically, periodontal complication can be occurred such as gingival recession, delay in periodontal healing, gingivitis, bone loss and decrease in the width of keratinized gingiva [1,10].
The patient was very cooperative, he was advised to not to disturbed the surgical filed very often until adequate soft tissue and bony healing occurs. The photos of the end of treatment show satisfactory periodontal result with sufficient bone and width of attached gingiva. The aligned maxillary incisors remained vital and responded normally to percussion and mobility and sensitivity testing.
All treatment objectives have been completed at an early age. The literature reports that a Class III malocclusion caused by maxillary deficiency should be treated as early as possible, mainly when dental and/or functional factors are involved, because it has an immediate positive esthetic impact and can redirect this unfavorable maxillary growth. On the other hand, if a young patient does not obtain a treatment at an early age, his or her skeletal discrepancy worsens with facial growth [26-28].
Orthodontic treatment should be directed to eliminating the patient’s complaint and achieving physiologic and functional occlusion with acceptable esthetics. In this patient, the functional aspect and the esthetic factor were so important, because of the poor smile and facial profile. Thus, the combined surgical and orthodontic therapy allowed complete esthetic and functional reestablishment of facial harmony.
Conclusion
Impacted maxillary permanent central incisors were successfully guided to designated place in the arch by closed-eruption technique and showed good stability. The presence of supernumerary teeth in such young children further justifies a routine radiological examination for early diagnosis and appropriate intervention to prevent any future complications.
When a skeletal Class III with maxillary retrusion and functional aspect is associated to impacted incisors, this should be treated as early as possible, since it allows a balanced growth of both jaws. However, even with early intervention, stability will depend on several factors (growth potential, age, genetic influence, etc.). Therefore, treatment overcorrection has been recommended to compensate the negative factors, and patients should be carefully followed until their growth is completed.
References
- Das D, Misra J (2012) Surgical management of impacted incisors in associate with supernumerary teeth: A combine case report of spontaneous eruption and orthodontic extrusion. Journal Of Indian Society Of Pedodontics And Preventive Dentistry 30: 329-332.
- Ramakrishna Y, Manjunath H, Sudhindra B, Autar KM (2012) Multiple supernumerary teeth associated with an impacted maxillary central incisor: Surgical and orthodontic management. Contemp. Clin. Dent 3: 219-222.
- Schmuckli R, Lipowsky C, Peltomaki T (2010) Prevalence and Morfology of Supranumerary Teeth in the population of Swiss Community. Schweiz Monatsschr Zahnmed 120: 987-993.
- De Oliveira GC, Drummond SN, Jham BC, Abdo EN, Mesquita RA, et al. (2008) A survey of 460 supernumerary teeth in Brazilian children and adolescents. Int J Paediatr Dent 18: 98-106.
- Bratu DC, Bratu E, Pacurar M, Popa G, Pop S, et al. (2011) The Prevalence of Supernumerary Teeth in a Group of Patients in Western Romania. Acta Medica Marisiensis 57: 581.
- Pels E, Mielnik-Blaszczak M, Szyszkowska AM, Krawczyk D, Prucia G, et al. (2006) Rare cases of supernumerary teeth. Ann Uni Mar Cur 2: 849-253.
- Mahabob MN, Anbuselvan GJ, Kumar BS, Raja S, Kothari S, et al. (2012) Prevalence rate of supernumerary teeth among non-syndromic South Indian population: An analysis. Journal of Pharmacy and Bioallied Sciences. Supernumerary teeth: Review of the literature and a survey of 152 cases. Int J Paediatr Dent 12: 244-54.
- Alling CA, Hellric JF, Alling R (1993). Impacted teeth. Philadelphia: WB. Saunders Co pp: 46-49.
- Kocadereli I, Turgut MD (2005) Surgical and orthodontic treatment of an impacted permanent incisor: Case report. Dent Traumatol 21: 234-239.
- Kamakura S, Matsui K, Katou F, Shirai N, Kochi S, et al. (2002) Surgical and orthodontic management of compound odontoma without removal of the impacted permanent tooth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94: 540-542.
- Kathleen AR, Folwarczna MA (2003) Mesiodens Diagnosis and Management of a Common Supernumerary Tooth. J Can Dent Assoc 69: 362-366.
- Di Biase DD (1971) The effects of variations in tooth morphology and position on eruption. Dent Pract Dent Rec 22: 95-108.
- Maity S, Kashyap RR, Naik V, Kini R, Begum N, et al. (2015) Multiple Permanent Impacted Supernumerary Teeth in a Non-Syndromic Patient- A Case Report with a Review of Literature. International Journal of Advanced Dental Science and Technology 2: 47-52.
- Sedano HO, Gorlin RJ (1969) Familial occurrence of mesiodens. Oral Surg Oral Med Oral Pathol 27: 360-361.
- Kulkarni VK, Vanka A, Shashikiran ND (2011) Compound Odontoma associated with an unerupted rotated and dilacerated maxillary central incisor. Contemp Clin Dent 2: 218-221.
- Bergstrom K (1977) An orthopantomographic study of hypodontia, supernumeraries and other anomalies in school children between the ages of 8-9 years. An epidemiological study. Swed Dent J 1: 145-157.
- Hüseyin K, Zuhal K, Aysegül S (2013) Characteristics of nonsyndromic supernumerary teeth in children and adolescents. Turk J Med Sci 43: 1013-1018.
- Hattab FN, Yassin OM, Rawashdeh MA (1994) Supernumerary teeth: report of three cases and review of the literature. ASDC J Dent Child 61: 382-393.
- Von AT (1992) Anterior maxillary supernumerary teeth: a clinical and radiographic study. Aust Dent J 37:189-195.
- Segura JJ, Jimenez-Rubio A (1998) Concomitant hypohyperdontia: simultaneous occurrence of a mesiodens and agenesis of a maxillary lateral incisor. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 86: 473-475.
- Ashu G, Priya N, Rakshit VSK, Deepti M, Harsimran SS, et al. (2015) Hyperactive Dental Lamina in a 24-Yearold Female - A Case Report and Review of Literature. Journal of Clinical and Diagnostic Research 9: ZE01-ZE04.
- Sreekanth KM, Tariq AA, Chitra C, Vinad KP (2014) Rare Association of Dens Invaginatus with Premolariform mesiodens: Radiographic and Histological Aspects. Smile Dental Journal 9: 24-26.
- Kupietzky A, Rozenfarb N (1993) Enamel pearls in the primary dentition: report of two cases. ASDC J Dent Child 60: 63-66.
- Indira MD, Kanika SD, Sujatha R, Praveen KPS, Gayatri DBM, et al. (2014) Molariform Mesiodens in Primary Dentition: A Case Report. Journal of Clinical and Diagnostic Research 8: ZD33-ZD35.
- Janson M, Janson G, Santana E, de Castro RCFR, de Freitas MR, et al. (2010) Orthodontic-urgical treatment of Class III malocclusion with extraction of an impacted canine. Am J Orthod Dentofacial Orthop 137: 840-849.
- Ljiljana SS, Ivan M, Budimir M, Tatjana ý (2013) Orthodontic-surgical treatment of the skeletal class III malocclusion: a case report. Vojnosanit Preg l 7: 215-220.
- Kapust A, Sinclair P, Turley P. Cephalometric effects of face mask expansion therapy in Class III children: a comparison of three age groups. Am J Orthod Dentofacial Orthop113: 204-212.
- Muthukumar K, Gobichettipalayam JA, Bhandari PK (2013) Early correction of class III malocclusion with rapid maxillary expansion and face mask therapy. Journal of Pharmacy and Bioallied Sciences 5: 169-172.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 13305
- [From(publication date):
December-2016 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 12523
- PDF downloads : 782