Research Article Open Access
Improvement in the Awareness of Palliative Care Nursing Using STAS-J in an Acute Care Hospital
Tsuyoshi Shirakawa1, Keiko Hikage2, Terumi Akino2, Tomoko Hirata2, Hiroko Shigematsu2, Tomoko Nagaie3, Shuji Arita1, Hiroshi Ariyama1, Hitoshi Kusaba1, Koichi Akashi1 and Eishi Baba4*1Department of Medicine and Biosystemic Science, Kyushu University Graduate School of Medical Sciences, Fukuoka, Japan
2Kyushu University Hospital, Fukuoka, Japan
3Fundamental Nursing, Department of Health Sciences, School of Medicine, Kyushu University, Fukuoka, Japan
4Department of Comprehensive Clinical Oncology, Faculty of Medical Sciences, Kyushu University, Fukuoka, Japan
- Corresponding Author:
- Eishi Baba, MD, PhD
Department of Comprehensive Clinical Oncology
Faculty of Medical Sciences, Kyushu University
3-1-1 Maidashi, Higashi-ku, Fukuoka 812-8582, Japan
Tel: +81-92-642-5228
Fax: +81-92-642-5247
E-mail: e-baba@c-oncology.med.kyushu-u.ac.jp
Received Date: March 23, 2015; Accepted Date: May 15, 2015; Published Date: May 18, 2015
Citation: Shirakawa T, Hikage K, Akino T, Hirata T, Shigematsu H, et al. (2015) Improvement in the Awareness of Palliative Care Nursing Using STAS-J in an Acute Care Hospital. J Palliat Care Med 5: 219. doi:10.4172/2165-7386.1000219
Copyright: ©2015 Shirakawa T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
The Japanese version of the Support Team Assessment Schedule (STAS-J) in palliative care units is reliable and widely used in Japan. However, there are few reports showing its impact on palliative care in acute care hospitals (ACHs) treating cancer patients. To verify the usefulness of STAS-J in ACHs, we evaluated changes in the awareness of care for patients among 48 nurses in a university hospital using a questionnaire administered before the introduction of STAS-J, after virtual case assessment, and after assessment of the first five inpatients. Statistical examination was performed by the Mann-Whitney U test. Most of the surveyed items, except noticing the anxiety of the patient’s family and information exchange with medical staff other than doctors, were significantly improved after the introduction of STAS-J (p<0.05). Approximately 60% of the nurses had affirmative opinions of STAS-J. The results suggested STAS-J is useful in improving the awareness of palliative care nursing in ACHs.
Keywords
STAS-J; Acute care hospital; Palliative care; Changing awareness of nurses
Introduction
In 2009 in Japan, the number of deaths from malignant neoplasms was 344,105, making it the most common cause of death [1]. The number of deaths due to malignant neoplasms has been increasing and this increase is predicted to continue. In the census-of-population report by the Ministry of Health, Labour and Welfare released in 2004, 3.4% of malignant neoplasm patients died in palliative care units (PCU) [2]. In addition, it was reported in 2007 that 89.9% of cancer patients died in hospitals, and most of them were ACHs [2].
The first PCU in Japan was established in 1981, and after that, the number of institutions providing palliative care has gradually increased. As of February 2014, there were 5,991 beds and 300 PCUs in Japan. Although PCUs have been increasing in response to the understanding of the importance of palliative care [3], the number of PCUs in Japan remains low and ACHs have to take over palliative care.
Kyushu University Hospital is an ACH with 1,275 beds that treats many malignant neoplasm patients. Our department mainly treats advanced and unrespectable malignant neoplasm patients with multidisciplinary treatment, such as chemotherapy or radiotherapy, and palliative care is also provided. Although the palliative care team of the hospital is functional, the main staff involved in caring for each patient are nurses and the doctor in charge. Therefore, nurses are required to have appropriate palliative care skills.
The purposes of hospice and palliative care are to offer suitable care to patients at the terminal stage as well as to their families, and to palliate not only physical cancer pain but also mental, social, and spiritual pain [4]. The need for quality standards in palliative care has been reported [5,6]. The Support Team Assessment Schedule (STAS) is an assessment scale used to evaluate hospice and palliative care. It was created as a clinical audit tool in Britain [7], but has spread all over the world, and its validity has been verified [7-9]. The Japanese version of the STAS (STAS-J) was created and its reliability and validity in PCUs have also been verified [10]. The validity of another scale to evaluate the quality of palliative care in Japan called the Care Evaluation Scale, which is an evaluation scale of hospice and palliative care by bereaved families, has also been reported [11]. Other standards evaluating the outcomes of palliative care have also been proposed such as the Good Death Inventory, an evaluation scale of quality of life of end stage cancer patients by bereaved families; however, it is not always a stable evaluation because it contains subjective survey items [12]. STAS evaluates the degree of achievement by grouping the main nine items (pain control, symptom control, patient’s anxiety, family’s anxiety, patient’s recognition, family’s recognition, communication between patient and family, communication between medical staff, and communication between medical staff and the patient and family) into four steps. STAS-J offers a stable evaluation of patients and can be used as a comprehensive scale measure of palliative care or as an audit tool [7].
Evaluation by STAS was reported to be useful for palliative care teams in ACHs [13]. STAS was also found to provide a reliable evaluation of palliative care performed by doctors and nurses in a university hospital in Japan [14]. However, to the best of our knowledge, there are no reports on introducing STAS-J to improve palliative care by changing the awareness of care among nurses treating advanced malignant tumor patients in ACHs. Therefore, the present study was conducted to verify the usefulness of STAS-J in an ACH for improving palliative care.
Methods
The present study was performed in the acute care ward of Kyushu University Hospital, Fukuoka, Japan, where around 30% of the patients suffer malignant tumors. Weekly joint conferences with doctors and nurses are held to discuss patient treatment. When doctors explain the patient’s condition to a patient and their family, nurses are present in about 75% of cases. STAS-J assessment was introduced in the ward in February 2009 and the present study period was from February 2009 to August 2009. Forty-eight nurses (25 in a general ward and 23 in an aseptic ward) agreed to participate in the study.
Nurses answered questions about their years of nursing experience, the number of times they had participated in STAS-J assessment (two or three times), and changes in their awareness after performing STAS-J assessment. The nurses completed a 22-item self-evaluation questionnaire with responses recorded on a four-point scale (1 indicating “I can do it well”, 2 indicating “I can do it moderately”, 3 indicating “I can seldom do it”, and 4 indicating “I cannot do it at all”). Questionnaire items related to awareness of care are listed in Table 1.The survey consisted of anonymous questionnaires, which were sealed and collected. The answers of nurses working in the aseptic ward were compared with those of nurses in the general ward who were in charge of solid tumour care. Nurses were also asked to write free description responses about their impression of STAS-J.
| Items | Significance level | p-value |
|---|---|---|
| Noticing pain | 775 | 0.011* |
| Dealing with pain | 677.5 | 0.001*** |
| Noticing physical symptoms other than pain | 770 | 0.006** |
| Dealing with physical symptoms other than pain | 664.5 | 0.001*** |
| Noticing anxiety | 778.5 | 0.011* |
| Dealing with anxiety | 741.5 | 0.009** |
| Noticing anxiety of the patient’s family | 826 | 0.068 |
| Dealing with anxiety of the patient’s family | 809.5 | 0.040* |
| Grasp of the patient’s recognition of the condition of their disease | 816 | 0.042* |
| Managing problems with the patient not fully recognizing the condition of their disease | 755 | 0.012 * |
| Grasp of the patient’s family’s recognition of the condition of the disease | 728 | 0.006 ** |
| Managing problems with the patient’s family’s recognition of the condition of the disease | 652 | 0.001*** |
| Grasp of communication with the patient and their family | 604 | 0.000*** |
| Managing problems with communication with the patient and their family | 781 | 0.025* |
| Information exchange with doctors | 313 | 0.000*** |
| Information exchange with dentists | 764 | 0.025* |
| Information exchange with pharmacists | 980.5 | 0.213 |
| Information exchange with physical therapists | 906 | 0.215 |
| Information exchange with nurse aids | 684.5 | 0.002 ** |
| Information exchange with clerks | 914 | 0.237 |
| Information exchange with dietitians | 715 | 0.004** |
| Providing information to the patient and their family | 648 | 0.000*** |
Table 1: Statistical significance test results of changes in awareness of care among nurses after STAS-J.
All nurses were required to perform STAS-J assessment of a virtual case before assessing actual patients. The nurses were surveyed with the same 22-item questionnaire regarding the awareness of care three times: before performing STAS-J assessment, after STAS-J assessment of a virtual case, and after assessment of the first five inpatients.
The reliability of the questionnaire was evaluated using the results of the latter two surveys. Responses for questions about years of nursing experience, the number of times participating in STAS-J assessment, and free descriptions of their impression of STAS-J were recorded after assessment of the first five inpatients. Comparison of the nurses’ responses by ward was based on the results of their questionnaire responses.
Statistical examination was performed using SPSS ver.13 (IBM Japan, Tokyo, Japan). The results of the third survey were compared with those of the first and the second surveys using the Mann-Whitney U test. P values of<0.05 were considered significant. This study complied with the ethical principles of the Declaration of Helsinki. Freedom of participation and protection of personal information were carefully considered in this study.
Results
Years of nursing experience and the number of times participating in STAS-J assessment
Among the 48 nurses who participated in this study, the number of years of nursing experience was 6.9 ± 5.4 years and the number of times participating in STAS-J assessment was 2.5 ± 1.4 times.
Changes in awareness of care of nurses after STAS-J
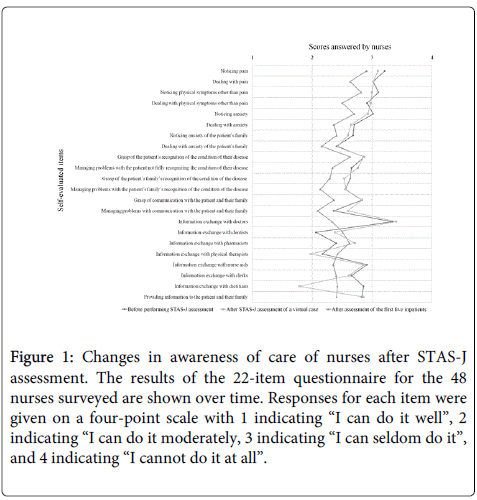
The nurses’ responses to the 22 self-evaluation questionnaire items were compared over time (Figure 1). For items other than information exchange with dentists, pharmacists, physical therapists, and dietitians, whenever the number of times of STAS-J assessment increased, the nurses’ self-evaluation responses improved. In particular, the items of dealing with pain, dealing with physical symptoms other than pain, or managing problems with the patient not fully recognizing the condition of their disease showed a larger improvement than items related to noticing how a patient or their family was handling the situation. Moreover, large improvements were also observed in the items about information exchange with doctors and nurse aids, and communication with the patient and their family. As shown in Figure 1, the results of the surveys performed after the virtual case assessment and after assessment of the first five inpatients exhibited almost equivalent values, suggesting that the reliability of the questionnaire was acceptable.
Figure 1: Changes in awareness of care of nurses after STAS-J assessment. The results of the 22-item questionnaire for the 48 nurses surveyed are shown over time. Responses for each item were given on a four-point scale with 1 indicating “I can do it well”, 2 indicating “I can do it moderately, 3 indicating “I can seldom do it”, and 4 indicating “I cannot do it at all”.
The results of the surveys administered before performing STAS-J assessment and after assessment of the first five inpatients were examined. Significant improvements were observed after the assessment of actual inpatients (p<0.001) in the items of dealing with pain, dealing with physical symptoms other than pain, managing problems with the patient’s family’s recognition of the condition of the disease, grasp of communication with the patient and their family, information exchange with doctors, and providing information to the patient and their family. Significant improvements were also observed in the items of noticing physical symptoms other than pain, dealing with anxiety, grasp of the patient’s family’s recognition of the condition of the disease, information exchange with nurse aids, and information exchange with dietitians (p<0.01), as well as in the items of noticing pain, noticing anxiety, dealing with anxiety of the patient’s family, grasp of the patient’s recognition of the condition of their disease, managing problems with the patient not fully recognizing the condition of their disease, managing problems with communication with the patient and their family, and information exchange with dentists (p<0.05). Comparison of the first and third surveys showed no significant improvement in the items of noticing anxiety of the patient’s family and information exchange with pharmacists, physical therapists, and clerks (p>0.05) (Table 1).
Comparison of wards
Nurses in the general ward treating patients mainly for solid tumors showed more significant changes in awareness of care than nurses in the aseptic ward. Significant improvements were observed in the items of dealing with anxiety of the patient’s family, grasp of the patient’s family’s recognition of the condition of the disease, managing problems with the patient’s family’s recognition of the condition of the disease, and information exchange with physical therapists, nurse aids, clerks, and dietitians (p<0.05) (Table 2).
| Items | Mann-Whitney U test | Wilcoxon W test | p-value |
|---|---|---|---|
| Years of experience as a nurse | 2097 | 4375 | 0.3426 |
| Number of times participating in STAS-J assessment | 241.5 | 517.5 | 0.4497 |
| Noticing pain | 1926 | 4204 | 0.0928 |
| Dealing with pain | 2033 | 4311 | 0.3119 |
| Noticing physical symptoms other than pain | 1909 | 4187 | 0.0822 |
| Dealing with physical symptoms other than pain | 1970 | 4248 | 0.1694 |
| Noticing anxiety | 1897.5 | 4108.5 | 0.0847 |
| Dealing with anxiety | 2123.5 | 4268.5 | 0.9106 |
| Noticing anxiety of the patient’s family | 1948.5 | 4226.5 | 0.1859 |
| Dealing with anxiety of the patient’s family | 1728.5 | 4006.5 | 0.0136* |
| Grasp of the patient’s recognition of the condition of their disease | 1914.5 | 4192.5 | 0.0957 |
| Managing problems with the patient not fully recognizing the condition of their disease | 1872 | 4150 | 0.0752 |
| Grasp of the patient’s family’s recognition of the condition of the disease | 1784.5 | 3995.5 | 0.0435* |
| Managing problems with the patient’s family’s recognition of the condition of the disease | 1625.5 | 3836.5 | 0.0046* |
| Grasp of communication with the patient and their family | 2092.5 | 4370.5 | 0.5218 |
| Managing problems with communication with the patient and their family | 1857 | 4135 | 0.0769 |
| Information exchange with doctors | 2021.5 | 4232.5 | 0.2871 |
| Information exchange with dentists | 2004.5 | 4149.5 | 0.3314 |
| Information exchange with pharmacists | 1887.5 | 4233.5 | 0.0854 |
| Information exchange with physical therapists | 1322 | 3668 | 0.0000* |
| Information exchange with nurse aids | 1446 | 3792 | 0.0001* |
| Information exchange with clerks | 1434.5 | 3780.5 | 0.0001* |
| Information exchange with dietitians | 357 | 1438 | 0.0000* |
| Providing information to the patient and their family | 2059 | 4270 | 0.5196 |
Table 2: Comparison of changes in awareness of care between nurses in the general ward and the aseptic ward.
Nurses’ impressions of STAS-J
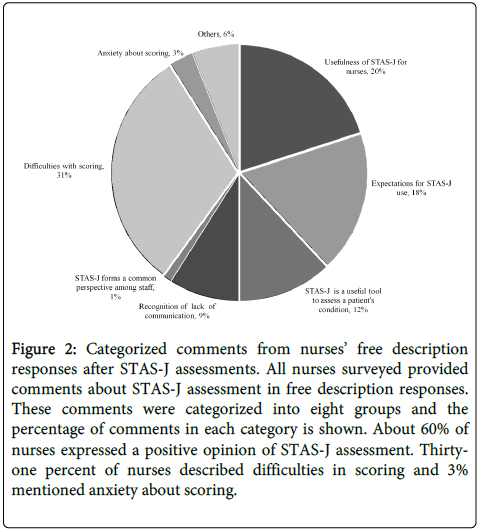
Twenty percent of nurses commented that STAS-J was useful for understanding palliative care and for reviewing their nursing skills. Eighteen percent commented that STAS-J met their expectations as a tool for connecting to other hospitals. Furthermore, 12% recognized STAS-J as an effective tool for allowing that them to grasp a patient’s pain and mental condition. Nine percent of nurses realized there was a lack of communication with medical staff other than doctors, and 1% commented that STAS-J enables establishment of a common perspective among medical staff. Although around 60% of nurses expressed positive impressions of STAS-J, some problems were also noted. For example, 31% mentioned that it was difficult to determine the appropriate score by themselves and 3% felt whether their scoring was correct (Figure 2). Some of the important comments from the nurses surveyed are listed in Table 3. .
| Category | Comment |
|---|---|
| Usefulness of STAS-J for nurses | Improved understanding of palliative care of cancer patients Good opportunity to review nursing skills |
| Expectations for STAS-J use | Possible application in other hospitals |
| STAS-J is a useful tool to assess apatient’s condition | Useful in understanding the patient’s pain Useful in understanding the patient’s mental condition |
| Recognition of lack of communication | Poor communication with medical staff other than doctors Poor communication with doctors |
| STAS-J forms a common perspective among staff | A common understanding of the patient was deepened |
| Difficulties with scoring | Scoring the patient’s objective symptoms is difficult Scoring the patient’s mental condition is difficult |
| Anxiety about scoring | Anxiety about the appropriateness of the nurses own scoring |
Table 3: Selected free description comments about STAS-J assessment from the nurses surveyed.
Figure 2: Categorized comments from nurses’ free description responses after STAS-J assessments. All nurses surveyed provided comments about STAS-J assessment in free description responses. These comments were categorized into eight groups and the percentage of comments in each category is shown. About 60% of nurses expressed a positive opinion of STAS-J assessment. Thirtyone percent of nurses described difficulties in scoring and 3% mentioned anxiety about scoring.
Correlation between years of experience and changes in awareness
No correlation in changes in awareness of care by years of nursing experience was observed in any items (data not shown).
Discussion
In order to provide high quality palliative care, the level of care must be evaluated with high validity. The reliability of STAS-J was already shown in PCUs [10] and in university hospitals [14]. In this study, we verified that STAS-J is useful for improving the quality of palliative care in ACHs by assessing changes in awareness of care among nurses.
One possible reason why the score for information exchange with doctors improved after the introduction of STAS-J might be that nurses had more chances to communicate with doctors in joint conferences. However, the score for information exchange with other medical staff did not improve, possibly because of limited chances to communicate with them in daily clinical work. Since direct information exchanges between nurses and other medical staff did not improve after STAS-J assessments in the present study, this may indicate an important issue for future research.
The evaluated score of physical symptoms was high after the introduction of STAS-J. Since patients tend to complain about their physical symptoms and nurses can easily assess such symptoms, changes in awareness among nurses after STAS-J assessment might have been induced by the daily care of patients [14]. We speculated that the reason the score for physical symptoms improved more than that of psychological symptoms was that medical staff can evaluate physical symptoms quantitatively, but psychological symptoms tend to be evaluated qualitatively. Therefore, in the future, we need to research how to effectively evaluate these two types of symptoms from the viewpoint of patients. Furthermore, good evaluation results were obtained over repeated STAS-J assessments and the results were closely related, suggesting that STAS-J is a useful tool to create adequate awareness of the important points of palliative care among nurses.
Significant changes in awareness of care were not observed for many items between nurses in the general ward and the aseptic ward. Interestingly, general ward nurses showed greater changes in awareness in items regarding care of the patient’s family, and in the items about information exchange with physical therapists, nurse aids, clerks, and dietitians. Since changes in awareness of care in general ward and aseptic ward nurses have yet to be clarified, it is still an important issue to be examined.
While many nurses pointed out the usefulness of STAS-J in their free description responses, difficulties with scoring and evaluation were also reported. STAS-J includes relatively difficult quantitative evaluation of the items that are not suitable for objective assessment, such as the patient’s recognition of the condition of their disease or communication. We should exercise caution in the face of such issues when STAS-J assessment is applied in acute wards of hospitals of various sizes and functions.
The present study had some limitations. First, the sample size was small, which may have limited interpretation of the data. We hope to conduct a subsequent study with a larger sample size in the future. Second, the questionnaire method was employed to examine changes in the awareness of care. Since the questionnaire method potentially possesses a limitation in terms of the reliability of measurements, we compared survey results obtained at two different times and found that the data were similar. There are few reports of the clinical usefulness of STAS-J, and methods of examining its usefulness of STAS-J, and methods of examining its usefulness are not firmly established. A recent study used the individual interview technique for assessing changes in awareness among nurses [15]. It may be important to continue to evaluate STAS-J using various methods.
The present study is the first to show the usefulness of STAS-J assessment in acute wards by inducing changes in the awareness of care of nurses with quantifiable and statistical analyses. Since STAS-J exhibited the potential to improve the quality of palliative care in a university hospital, further examination of the effectiveness of STAS-J assessment in various kinds of hospitals is required.
Conflict of Interest Statement
None of the authors has any conflict of interest.
References
- Vital Statistics (2009) Statistics and Information Department. Report, Ministry of Health,Labour and Welfare, Japan.
- Vital Statistics (2004) Statistics and Information Department. Report, Ministry of Health,Labour and Welfare, Japan.
- Akaza H, Saeki T, Kawai K, Keisuke A, Seiji I,et al. (2001) Comparison of management of advanced cancer in various organs. Gan To Kagaku Ryoho28(12):1845-1855.
- Cancer pain relief and palliative care (1990) Report of a WHO Expert Committee. World Health Organization Tech Rep Ser 804: 1-75.
- Higginson I (1993) Advanced cancer: aiming for the best in care. Qual Health Care 2:112-116.
- Ingleton C, Faulkner A (1995) Quality assurance in palliative care: some of the problems. Eur J Cancer Care 4:38-44.
- Higginson IJ, McCarthy M (1993) Validity of the support team assessment schedule: do staffs’ ratings reflect those made by patients or their families? Palliat Med 7:219-228.
- Lo RS, Ding A, Chung TK (1999) Prospective study of symptom control in 133 cases of palliative care inpatients in Shatin Hospital. Palliat Med 13:335-340.
- Carson MG, Fitch MI, Vachon ML (2000) Measuring patient outcomes in palliative care: a reliability and validity study of the Support Team Assessment Schedule.Palliat Med 14:25-36.
- Miyashita M, Matoba K, Sasahara T, Kizawa Y, Maruguchi M, et al. (2004) Reliability and validity of the Japanese version of the Support Team Assessment Schedule (STAS-J). Palliat Support Care2:379-385.
- Morita T, Hirai K, Sakaguchi Y, Maeyama E, Tsuneto S, et al. (2004) Measuring the quality of structure and process in end-of-life care from the bereaved family perspective. Journal of Pain and Symptom Management27: 492-501.
- Miyashita M, Morita T, Sato K (2008) Good death inventory: a measure for evaluating good death from the bereaved family member’s perspective. Journal of Pain and Symptom Management 35:486-498.
- Edmonds PM, Stuttaford JM, Penny J (1998) Do hospital palliative care teams improve symptom control? Use of a modified STAS as an evaluation tool. Palliat Med 12:345-351.
- Miyashita M, Yasuda M, Baba R (2010) Inter-rater reliability of proxy simple symptom assessment scale between physician and nurse: a hospital-based palliative care team setting. Eur J Cancer Care 19:124-130.
- Miyagi C,Kamizato M (2011) Core nurses’ perception of the introduction of STAS-J, a qualityassessment tool of palliative care in the palliative care unit. Journal of Okinawa Prefectural College of Nursing 12.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 14999
- [From(publication date):
May-2015 - Jul 06, 2025] - Breakdown by view type
- HTML page views : 10396
- PDF downloads : 4603