Case Report Open Access
Importance of Patient’s Narrative and Dialogue in Healthcare
Jan Sitvast*
Lecturer for Nursing Specialists, Hogeschool Utrecht, The Netherlands
- *Corresponding Author:
- Jan Sitvast
Lecturer for Nursing Specialists, Hogeschool Utrecht, The Netherlands
E-mail: jan.sitvast@hu.nl
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Introduction
There is a growing interest in the central role of the patient’s narrative in health care. How patients see themselves and how they assimilate their experiences with illness and recovery in their larger life story becomes more important when we see health as dynamic, where patients are coping with adversities in life, instead of a static state of idealized well-being and absence of disease (Huber et al., 2011). The self-image of a person is to a large degree transitory and determined by narratives about one’s everyday life, especially the meaningful ones about life events (McAdams, 1993; Miller et al., 1990). Our identity is shaped by the concepts that we use to label our experiences in the past and in the present. Personal stories sometimes serve to organize the otherwise raw and overwhelming sensations, disturbing feelings and thoughts that surround difficult life situations. What a person expresses and communicates need not always be ‘storied’ in linguistic formats. A person can also embody what he goes though or find expressive means other than language to ‘tell’ his story, for instance with photographs (Sitvast, 2012). The term ‘narrative’ encompasses all these formats of expression (Sandelowski, 1991). The case of Pieter will demonstrate how this looks like and how health professionals can respond to the narrative in such a way that it furthers better mutual understanding.
The Case
Pieter is a 40 year old man who has been diagnosed with schizophrenia in the past. Today he lives alone in an apartment in the centre of a medium-sized provincial town in the Netherlands. An outreach worker from the local community mental health centre is in regular contact with him.
Pieter has Indonesian heritage and identifies himself as part of the indigenous people of North-America. He dresses as one of them and he has transformed his apartment to reflect this heritage and that’s why it is adorned with totem poles, indigenous masks, bow and arrows, feathers, etc. He makes these objects himself and names them using native tribal convention. With all these small works of art there is a story that has been threaded into his self-made mythological world which incorporates his own personal experiences. Wearing the feathered attire at times makes him a colourful figure in the streets of the town where he lives.
Pieter has been an inpatient for many years and is known for longstanding traumatic history of violent incidents, in which he hurted himself and others (nurses on the ward). His life has now come into a more tranquil phase and six months ago he moved from the hospital to his own apartment. I visit him at his home in my role as his mentor nurse supporting him in his daily life and maintaining contact with the services. When I ring the bell and he opens the door, I see that I have woken him up from his afternoon nap. After welcoming me he makes me a cup of tea. He cleans the glass carefully before pouring out the tea, which I think is very considerate. I then admire his drawings and Pieter starts telling about the figures he has depicted. It turns out to be a magical worldview with mythical heroes, spirits and demons which are interwoven with his own life story. I listen to what he tells me with attention and then answer him that apparently, he has come upon deeper truths that he now tries to put into words. I name the longing for purity and cleanness in his story and how these seem to be related to the tribal peoples of North America in their intercourse with the environment and the harmony of nature. I suggest he wants that too and that that may be a good reason to tidy up his room and clean it. Pieter agrees and we set about to clean his house.
Narrative Individuation
How a person sees himself is to a large degree a function of their interaction with others. When the relationship between people changes then the image that people have of themselves also changes. Someone’s identity is not a segregate closed inner world in their head, but something that interplays with social functioning (Polkinghorne, 1998). Someone’s identity can even be the condensation of all stories that a person tells himself and others in social interaction. Every individual has the need to position himself in the social and cultural room (space) that he participates in and that he ‘inhabits’. This appropriation of one’s own place is sometimes called ‘narrative individuation’ (Kunneman, 1995). The individual wants to determine the coordinates of his position here and now. This is done in a narrative way (verbal and non-verbal) and it suggests that ‘co-habitants’ (the others) of the same social room hear the narrative, respond to it and can participate in it. The delimiting of one’s own place within the social space results from the others acknowledging the narrative, but also from others denouncing it or evading it. The individual constructs unremittingly and continuously his own identity in the diversity of many social rooms. In the case of Pieter for instance, we can see how the nurse is shown around in Pieter’s house and is invited- as it wereto share the meanings that Pieter gave to his life where identity then becomes co-constructed.
Role of the Nurse
Nurses can help people to lift their life out of the shackles of the disease (Grypdonck, 1999). Diseases and disorders, limitations and handicaps are threats or challenges to a meaningful life story. To be able to help patients to live a life beyond disease and experience life as meaningful the nurse must acknowledge that the patient’s narrative plays a central role in the communication between health care professionals and patients. The patient is a subject with whom the nurse relates to in a subject-subject relationship. This is a core aspect of person-centred care (McCormack et al., 2010): the perspective of the patient, his or her subjectivity, cannot be ignored and nurses should help the patient to voice his story. Nurses are in a unique position to support patients to express their knowledge and experience of the physical and social world they inhabit here-and-now (Benner, 2000). For instance, nurses can name the sorrow as they see it in patients and make it an issue that one can speak about. It is not necessarily rational knowledge already present in the mind but also experience and intuition that can be traced from body language. Sensations and experiences are often strongly influenced by emotions and sensorymotor observations and patterns of coping. People ‘live’ their story, they ‘are’ their narrative. The embodiment of experiential knowledge or intuition based on ‘events’ in the psychosocial domain can be ‘read’ by nurses. Putting in words what is only implicitly engrained in the body is what proficient nurses are good at. Communication with the patient about his story can be healing. The emotion to be understood, especially in the situation when the nurse mirrors a message that the patient before did not (fully) understand himself or could not face, liberates and opens up new horizons of meaning and sets free new energy (Benner, 2000; Wiltshire, cited in Aranda & Street, 2001).
Point of Impact
This is the point of impact where nurses connect. The nurse is the interlocutor, listener and audience at the same time, which means that he always plays a role in the patient’s story. The patient cannot but communicate, even when he keeps silent at times. The reactions of the nurse will feedback to the patient, including a possible nonresponse. Trying to make sense of the patient story is the first challenge. Sometimes the story is inaccessible at first sight and it might be hard to connect in an empathetic way, as may be the case with psychotic patients. Yet even then one can read a message in the deep structure of the story that does make sense, because in psychosis one also borrows meaning from the repertory of collectively shared images in our culture and these are never purely idiosyncratic.
Acknowledging this meaning to exist and validating it as an expression of a legitimate need, wishes or feelings is of enormous therapeutic importance. How to meet a person’s wishes and needs comes next. In Pieter’s case the nurse has validated his experience without passing a judgement about its reality. He did this by naming a deeper layer of meaning: Pieter’s longing for purity, cleanness and harmony. This deeper meaning can be empathetically shared by the nurse while the seemingly psychotic phrasing on the surface impressed as bizarre and incomprehensible. Pieter felt himself understood and accepted. The nurse found an entry to ground their contact on a shared understanding and to connect with him. On this ground the nurse can, when this may be helpful, suggest alternative turns to the story or stimulate the patient to take up another perspective (Clark & Standard, 1997). For instance in the case where a person imputes the role of victim to himself in the story he tells, the nurse may suggest that a more active role is also possible. The nurse may facilitate this shift in perspective by creating conditions for a social interaction in which the patient experiences how things can be different and in which he can have alternative roles. In an artsbased project for instance instigated by Sitvast (2012) people with severe mental illness organized and directed the exhibition of their photographs themselves. They entertained, informed and touched visitors emotionally with their photo stories. For one moment they had become actors in their own right and deliverers of an exhibition enjoyed by others instead of being mere consumers of care.
Summarizing the roles a nurse can play in a narrative, personcentred approach of care the nurse must:
• Try and understand the essence behind the surface structure of the patient narrative.
• Phrase the message and give it back to the person to check whether it is correctly understood.
• Validate the narrative’s essential message.
• Look for common grounds and starting-points within the room of the narrative.
• Base nursing interventions on these common grounds and shared starting-points (preferably in a shared decision making process).
Normative Professionalism
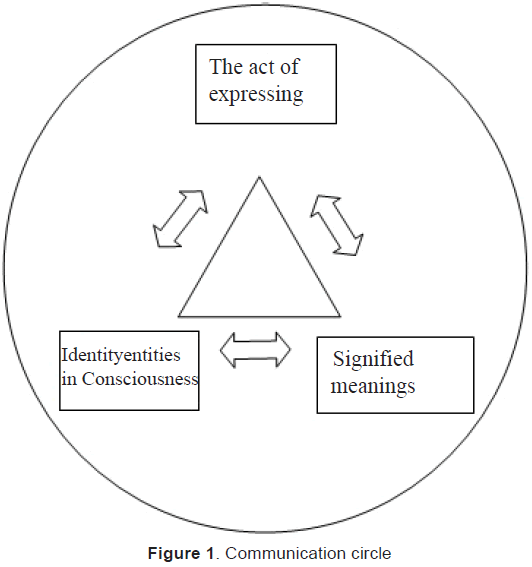
This dialogical narrative approach has been described in a literature review by Michael Bakhtin and was adopted in nursing practice (Bowers & Moore, 1997). Bakhtin assumed that in social interaction there is a constant and continuous interchange and reciprocal influence of consciousness and meaning making (Figure 1). The social and psychological entities in the conception of the self that arise from interactions of the person with others have a fluid character, because they are elements of a dialogue with an open end.
Nursing can also be perceived as a process of social interaction in which the nurse applies communicative strategies to mediate in what illness and handicaps mean for living one’s life. This can best be done in an open non-judgmental way of exchanging information where events and experiences get signified within the relationship and not on basis of a hierarchical difference in knowledge between an expert professional and an ‘ignorant’ patient. Of course, the expertise of the professional will come in at some point in time, for instance when the patient asks for a definition of his complaints in terms of health and disease (the diagnosis). The professional can draw on the universal (generalized) knowledge of therapeutic interventions, sometimes evidence-based, to meet individual care needs. Doing so he will make use of a technical medical and nursing jargon, diagnostic concepts, etc. This language often replaces the patient’s way of phrasing his complaints and needs. It is what the patient may also want when the professional language legitimizes his care needs better than his own formulations. But the other side of the coin is that a gap is created between the professional and the patient narrative which means that the patient can sometimes hardly recognizes him in a diagnosis and treatment and nursing plan. Of course, with the professionalization of nursing we have now got classifications and standard interventions that create its own jargon. However beneficial this has been for the development of nursing, it does not justify that the patient narrative serves no other aim than being a source of information for the ‘real’ narrative: the diagnostic description in a nursing or treatment plan. In order to avoid this pit fall we need a normative professionalism beside an expertise-based professionalism. While the expertise-based professionalism is related to the concept of ‘performance’ we connect normative professionalism with ‘reflectivity’ (Widdershoven, 1999; Sevenhuijzen, 1996), ‘responsiveness’ (Tronto, 1993) and ‘presencing’ (Baart, 2001; Kal, 2001).
Reflectivity is the ability to see things in a larger context. Professionals often give priority to what must be done and the action needed to solve problems. They run the risk that they develop a fixation on interventions, which they can defend very well from their professional expertise, but less from the point of view and the context of the patient. The why and to what aim questions are sometimes answered from a narrow framework of diagnostic thinking. However, diagnostic reasoning should always be an integral element of a broader clinical reasoning that considers a wide range of psychosocial issues. This is where responsiveness is important. Do we hear what deeper needs and wishes the patient voices with his narrative or do we interpret his expressions too easily as symptomatic and exemplary of the disease or illness? Does our response to the patient connect with his request for help and his life world? That takes a professional who can be present as a subject, someone who does not hide behind the mask of his formal professional identity, but who uses his own personal qualities as instruments to connect with the patient in an ‘authentic’ way. How did that look like in Pieter’s case Pieter? Here the nurse used a kind of stoic interest (that was natural to him) in his approach to Pieter. ‘Presencing’ has also everything to do with how accessible a professional is: the patient must be able to experience that he can approach a professional easily, meaning that an appeal can be made with the professional. With Pieter this could have meant that if there was a conflict with neighbours the nurse might step in to mediate between Pieter and his environment. This touches on ‘performance’.
Performance (‘prestatie’ in Dutch that comes from the Latin ‘preastare’ that has two meanings: excel in something and making oneself answerable for a person) stands for the capability, the expertise and the courage to act in situations where vulnerable sick people make an appeal to us. They need professionals to act adequately and be trustworthy in their performance. Performance is therefore related more to expertise-based professionalism (Jansen, 2005) and both (normative and expertise-based professionalism) are needed to realize good care.
Discussion and Conclusion
Of course, nursing encompasses more than supporting patients in meaning making from experiences related to health and illness. Beside the subjectivity of the experience there is the objectivity of the physical existence and the psychosocial existence as well (for example if Pieter was threatened with eviction for not paying his rent or for making a disturbance). Nursing care consists of the ‘technical’ procedures and actions to remedy physical needs and psychosocial needs. The narrative here is second to the skilled and trustable performance, even where the technical care almost always carries a meaning to the patient and is embedded in a certain context.
The interchange between the mind and the body is a complex one. We have focused here on the influence in one direction: from diseases and disorders by way of narrative to meaning making. However this path has multiple directions, for example, a path that runs from hope based on a newly found perspective in one’s story to recovery or mitigating the consequences of a disease. This may be the case when hope gives energy, motivates a person to change his life style and where it strengthens his immune system. Hope and a resurgence of vitality may be mediating factors here to find the strength (resilience) to become better or rather, coping better and in this way realize a higher quality of life (Huber et al., 2011). In the case of Pieter the newly found energy and the focus on purity and cleanness lend him coherence in his identity and his psychological make-up, but how to reconcile this with functioning in a society that tolerates only a certain degree of other-ness remains the challenge and the stake for a continuous dialogue between him and his mentor nurse. How Pieter and his family can achieve a mutual kind of understanding is another matter of concern. The nurse considered organizing a so-called open dialogue meeting with everyone involved (Seikkula et al., 2011). He knew that the open dialogue method, which has been developed in Finland, has been remarkably successful in striking an alliance between the patient and his social environment, reducing relapse figures as well as re-hospitalization figures.
References
- Aranda, S., & A. Street. (2001). From individual to group: use of narratives in a participatory research process. Journal of Advanced Nursing, 33(6): 791-797
- Baart, A. (2001). Een theorie van presentie. Utrecht: Lemma
- Benner, P. (2000). The roles of embodiment, emotion and lifeworld for rationality and agency in nursing practice. Nursing Philosophy, 1: 5-19
- Bowers, R., & K.N. Moore. (1997). Bakhtin, Nursing Narratives and Dialogical Consciousness. Advances in Nursing Science, 19(3): 70-77
- Clark, M., & P.L. Standard. (1997). The caregiving story: How the narrative approach informs caregiving burden. Issues in Mental Nursing, 18: 87-97
- Grypdonck, M. (1999). Het leven boven de ziekte uittillen. In: Pool, A. en J. Lambregts (red.). Verpleegkundige zorgverlening aan chronisch zieken. Utrecht: Lemma, Utrecht
- Huber, M., Knottnerus, J.A., Green, L., Van der Horst, H., Jadad, A.R., Kromhout, D., et al., (2011). How should we define health?. BMJ, 343: d4163.
- Jansen, M. (2005). Presentie., & Prestatie. Sleutelbegrippen in een verpleegethiek. Proefschrift. Utrecht: Universiteit van Humanistiek
- Kal, D. (2001). Kwartiermaken. Werken aan ruimte voor mensen met een psychiatrische achtergrond. Meppel: Boom
- Kunneman, H. (1995). Narratieve individualiteit en normatieve professionaliteit. In: Baars, J., & D. Kal (red.). Het uitzicht van Sisyphus. Maatschappelijke contexten van geestelijke (on)gezondheid. Wolters-Noordhoff, Groningen, 1995, p. 61-84
- McAdams, D.P. (1993). The stories we live by. Personal Myths and the Making of the Self. New York: The Guilford press
- McCormack, B., & McCance, T. (2010). Person-centred Nursing. Theory and Practice. Oxford: Wiley-Blackwell
- Miller, P.J, Potts, R., Fung, H., Hoogstra, L., Mintz, J. (1990). Narrative practices and the social construction of self in childhood. American Ethnologist, 17(2): 292-311
- Polkinghorne, D.E. (1998). Narrative Knowing and the Human Sciences, Albany NY: State University of New York Press
- Sandelowski, M. (1991). Telling Stories: Narrative approaches in qualitative research. Journal of Nursing Scholarship, 23(3): 161-166
- Sevenhuijsen, S. (1996). Oordelen met zorg: feministische beschouwingen over recht, moraal en politiek, Amsterdam/Meppel: Boom
- Seikkula, J., Alakare, B., & Aaltonen, J. (2011). The comprehensive open-dialogue approach (II). Long-term stability of acute psychosis outcomes in advanced community care: The Western Lapland Project. Psychosis, 3: 192-204
- Sitvast J.E., & Abma T.A. (2012). The photo-instrument as a Health Care Intervention. Health Care Analysis, 20: 177-195
- Widdershoven, G. (1999). Care, cure and interpersonal understanding. Journal of Advanced Nursing, 29(5), 1163-1169.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 4009
- [From(publication date):
June-2017 - Apr 16, 2025] - Breakdown by view type
- HTML page views : 3141
- PDF downloads : 868