Research Article Open Access
Implications of the SURE-P MCH National Village Health Worker Experience in Northern Nigeria for the Road Map for Village Health Workers in Nigeria
Findley SE1*, Afenyadu G2, Okoli U3, Baba H2, Bature R2, Mijinyawa S2, Bello-Malabu J3, and Mohammed Sidi A31Women for Health and Mailman School of Public Health, Columbia University, New York, USA
2Women for Health (W4H), Kano, Nigeria
3National Primary Health Care Development Agency – SURE P MCH, Abuja, Nigeria
- *Corresponding Author:
- Sally E Findley
Senior Technical Advisor
Women for Health and Professor, Mailman School of Public Health
Columbia University, New York, USA
E-mail: sef5@columbia.edu
Received date: Feb 21, 2016; Accepted date: Apr 28, 2016; Published date: Apr 30, 2016
Citation: Findley SE, Afenyadu G, Okoli U, Baba H, Bature R, et al. (2016) Implications of the SURE-P MCH National Village Health Worker Experience in Northern Nigeria for the Road Map for Village Health Workers in Nigeria. J Community Med Health 6:419. doi:10.4172/2161-0711.1000419
Copyright: © 2016 Findley SE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Community Health Workers (CHWs) can facilitate access to primary health care services among isolated rural communities. This study examines how Nigeria’s Subsidy Reinvestment and Empowerment Program on Maternal and Child Health (SURE-P MCH) Village Health Worker (VHW) programme provides a model for the Nigerian Road Map for VHWs.
Methods: We used pre-post with comparison model design, comparing two successive VHW cohorts, recruited in 2013 (n=109) and in 2014 (n=147) in Jigawa, Katsina and Zamfara states, northern Nigeria. We collected performance statistics and conducted interviews with the VHWs, and focus group discussions with the VHWs, their CHEW mentors, the in-charges at the facilities, and the village health/ ward development committees overseeing the recruitment and support of the VHWs. Significant differences between the 2013 and 2014 cohort were assessed using bi-variate statistics.
Results: All VHWs were female. The VHWs worked 20.8 hours/week, and averaged 34.3 home visits/month. After their training, 90% were comfortable with their primary tasks of encouraging antenatal care (ANC) visits and teaching about a healthy pregnancy. They identified 11.7 newly pregnant women per month, of whom 9.0 went to ANC. The pictorial guides were the most useful tools for encouraging ANC and facility deliveries. Compared to before the VHWs began work, clinics recorded 84.8% more women making 4+ ANC visits and 119.9% more skilled birth deliveries. Clinical consultations at the PHC referral sites for the VHWs increased significantly after the introduction of the VHWs and again from 2013 to 2014 (p < 0.010). Qualitative feedback identified the following factors supporting their effectiveness: linkage to support systems within and in the peripheral health facility, pictorial materials and a thank-you stipend for services.
Conclusion: The SURE-P MCH VHWs were associated with significant increases in maternal health service uptake at the rural PHCs to which they were affiliated. The factors associated with their effectiveness should be incorporated into the Nigerian Road Map for VHWs: training in coaching health promotion topics, pictorial guides to assist in coaching, mentoring and support from the CHEWs and the community, and a nominal stipend.
Keywords
Village health workers; Community health worker
Introduction
Community Health Workers (CHWs) have been successful in mobilizing rural populations to utilize health services. CHWs who work in their own communities are trusted, and they can share information about critical maternal and child health services in the community in ways that women understand and trust. In dozens of countries, they have been effective at helping women adopt improved health care practices and make use of life-saving services at the primary health center [1,2]. Importantly, in some countries, such as Pakistan [3] and Tanzania [4], the CHWs are all female.
Maternal mortality rates (MMR) in Nigeria are amongst the highest in sub-Saharan Africa and in the world, 1,549 and 1,025 per 100,000 live births in the North East and North West geopolitical zones, respectively [5]. There are evidence-based interventions which reduce maternal and new-born mortality [6], but in northern Nigeria, access to these interventions is limited. Many women have no ante-natal care, and only 10-16% of women are attended by a skilled attendant at delivery [5,7].
Achieving the sustainable development goals for maternal and newborn health will require accelerated and equitable expansion in access and utilization of these evidence-based interventions [3], most of which are associated with a greater utilization of quality maternal, and child health services, including both routine and emergency obstetrical services.
Because of their effectiveness at promoting an uptake of primary and obstetrical health services in isolated rural areas, when Nigeria began a re-examination of its strategy for promoting maternal and child health, the country focused on CHWs, and female CHWs, in particular. In Nigeria, and particularly in northern Nigeria, women will welcome a woman into their home to talk about their health concerns, but they will find it difficult to welcome a man [7].
The National Primary Health Care Development Agency was tasked to prepare a National Road Map for VHWs, and it became clear that particular attention was needed to ensure that women would be given priority for this cadre [8].
Promotion of maternal and child health has been a priority for the Subsidy Reinvestment and Empowerment Programme, Maternal and Child Health (SURE-P MCH) Programme [9]. Experience with the existing Federal Government Midwives Service Scheme (MSS) showed that providing midwives in rural clinics was not enough to encourage women to utilize services at PHC facilities [10,11].
The program recognized they needed female VHWs to reach out to other women in the communities, at their homes, place of work, social and religious gatherings to encourage them to come to the clinic. Accordingly, the SURE-P MCH VHW was established nationally as a paid female CHW, selected from the community and trained and supervised to mobilize women and provide a limited set of preventive health services, with the primary emphasis on promoting ante-natal care, birth preparations, and encouraging deliveries by a skilled birth attendant.
Women for Health, a UK-Aid funded program operating in northern Nigeria, was eager to learn how this cadre supported the overall efforts to expand female health care worker cadres in northern Nigeria. Therefore, Women for Health and SURE-P MCH collaborated in conducting an implementation research study aimed at identifying how well the SURE-P MCH VHW model worked, including implementation details that might be improved in successive expansion waves of the SURE-P MCH VHW program. Our collaborative study was designed to assess the impact of the training on skills learned, the support and integration of the VHWs into the community and primary health care facility, and assess how the VHWs affected use of maternal health services.
The SURE-P MCH VHW model
The SURE-P MCH VHWs are the link between the community and an integrated maternal health care service network at the rural PHC. Each of the designated PHC was provided with a trained midwife, supported by the SURE-P MCH program, and they in turn were supported by two Community Health Extension Workers (CHEWs). The CHEWs were trained to support the midwife in the provision of antenatal care and basic infant and child health services. Each CHEW was trained to mentor and supervise three Village Health Workers (VHWs), each of the VHWs working in a village within service area of the PHC. This integrated program of services was implemented in 1000 rural PHCs across the 36 States and Federal Capital territory of Nigeria. The VHWs were recruited and deployed in 2 phases, 3000 VHWs in January 2013 and an additional 3000 VHWs in January 2014.
The SURE-P MCH VHW is the first point of contact between primary health care services and the community. Their scope of work is:
• Conduct home visits and follow-ups
• Identify pregnant women in the community
•Educate pregnant women about maternal new-born and child health (MNCH) care
• Mobilize women to seek MNCH services at PHC facilities
• Provide basic first aid services [9]
The CHEW mentors provided the 6-day training for the VHWs, covering the following topics:
• VHW role in the community
• Community outreach and making home visits
• Antenatal care and birth preparations
• Pregnancy complications and danger signs
• Healthy foods for mothers and children
• Postnatal and newborn care
• Healthy child spacing
• First aid and wound management
• Record keeping and making referrals to the PHC
Each VHW was given a pictorial guide to help them explain MNCH practices, and a tool kit with first aid supplies, iron and folic acid tablets for pregnant women, soap, baby wipes, sanitary pads, and condoms. They were asked to keep a tally of the topics covered in their weekly visits, and the tally sheet used pictures to distinguish the specific activities of each visit.
One important clarification was to distinguish documentation of education about ANC or danger signs of a delivery from actual visits made to the PHC. They were expected to maintain regular contact with 30 women in their community, focusing on pregnant women or those with newborns. Each VHW established a bank account in her own name, and in accordance with the Global Health Workforce Alliance best practices for CHWs, she received a monthly deposit from SURE-P MCH of N10,000 (approx. $60 per month) [12].
The primary selection criterion for this work was to be female. The following additional selection criteria were expected to enhance her ability to promote MNCH in her community: resident in the community, age 25 and above, ever or currently married, basic literacy, high social standing in the village, willing to serve for at least two years. The Ward Development Committee (WDC) followed SURE-P MCH guidelines in soliciting, interviewing and selecting candidates to be sent for VHW training. Each WDC sent 12 candidates for training, from which six were selected for service.
Study Methods
The study was conducted in three states in northern Nigeria where Women for Health is a partner: Jigawa, Katsina and Zamfara. These are all states sharing a similar language (Hausa) and culture in terms of gender roles and expectations. Each State team constituted a VHW State Implementation team. The teams developed implementation research protocols and tools collaboratively at three workshops that involved the W4H state team leaders, Programme for the Re- Invigoration of Routine Immunization and Maternal, Newborn, and Child Health (PRRINN-MNCH) program officers for demand and for operations research, the SURE-P State focal points, and the SURE-P focal person for implementation of the VHW program.
The research protocols were reviewed and subsequently approved by each State’s ethics board. The key research data collection activities were carried out as follows:
• VHW feedback using rapid assessment surveys: Multiple choice surveys conducted December 2014 with a sample of VHWs at approximately 20 selected PHC sites in the State (n= 256, with 109 from the 2013 cohort VHWs and 147 from the 2014 cohort). Research assistants conducted the interviews with the VHWs in the local language (Hausa), and recorded their responses directly into the precoded English interview forms. The responses were then coded and analysed using simple cross-tabulations, descriptive statistics, t-tests and Chi-Square tests to assess significant differences.
• Documentation of VHW service delivery: On-site compilation of service statistics from monthly CHEW supervision logs and the VHW tally sheets, for the period January 2013 through April 2014, for all 283 VHWs who began in the three states in January 2013.
• Feedback on a remedial training in completion of the VHW tally sheets, conducted in sixteen communities across fourteen Local Government Areas (LGAs) of Jigawa State. The training was attended by 96 VHWS, 16 facility in-charges, 16 Village Development Committees (VDCs) and 31 CHEW Mentors in the 16 communities.
• Focus group discussions with 6 VHW at 2 selected PHC sites in each state. The PHC sites were selected based on review of the initial 6 months of CHEW mentor reports of 2013 VHW cohort activities and related consultations at the site. One site had outcomes in the upper quartile, while the other site had relatively low outcomes, in the lowest quartile. This selection allowed us to focus on what was working and what was not working as well.
• Clinical consultation data: The research team collected data on the following performance indicators from the national service logs from each PHC facility with VHWs in the three states:
• Number of Antenatal care (ANC) visits
• Number of 1st ANC visits (ANC 1)
• Number of 4+ ANC visits (ANC 4)
• Number of women having home deliveries
• Number of women having skilled birth attendants (SBA)
These were then used to calculate the average monthly performance ranking of the VHWs at each of the sites, ratio of ANC visits to pregnant women, ratio of ANC4 to ANC1, ratio of SBA to total deliveries. Because we wanted to learn from both the successes and failures in implementing the VHW program to date, we used the bestworst method to obtain detailed information and feedback at 4 sites performing above average and 4 PHCs performing below average according to the ratio of ANC4 to ANC1 and the ratio of SBA to total births.
These data were analysed using cross-tabulations and pair-wise t-tests to assess differences in consultation rates between 2012-2013 and 2013-2014.
All interviewers were trained using the Hausa versions of the questionnaires and in preparing complete transcripts of the in-depth interviews and group discussions. At the two selected sites in each state, the 6 VHWs were invited to participate in a focus group discussion about their experiences. These focus group discussions were led by the W4H state team leader, with co-leadership from the previously trained W4H local engagement consultant (LEC). There were 6 participants in each focus group.
Results
Characteristics of the village health workers (VHWs)
The average age of the VHWs was 36.7, with the 2014 significantly older with a mean age of 39.8 versus 36.4 for the 2013 cohort (Table 1). The VHW were married for an average of 9.5 years with an average of 4.6 children, with the 2014 cohort having on average almost one more child than the 2013 cohort. Only one-fourth had any secondary school education, with the 2013 cohort having higher secondary education completion compared to the 2014 cohort. Most (82%) had some source of cash income. Three-fourths (76%) had previously volunteered, such as serving as a volunteer mobilizer for child immunizations or other health-related events (Table 1).
| Characteristic | Total (n=256) | 2013 cohort (n=109) | 2014 cohort (n=147) |
t-test (p) |
|---|---|---|---|---|
| Age (mean) | 36.7 | 36.5 | 39.8 | 2.15 (0.033) |
| Years married (mean) | 9.8 | 10.2 | 9.5 | 0.43 (0.668) |
| Number of children | 4.6 | 4.7 | 5.4 | 1.78 (0.038) |
| Had secondary or higher education | 24% | 30% | 19% | 2.18 (0.030) |
| Other source of income | 82% | 83% | 79% | 1.04 (0.850) |
| Previously had been Community Volunteer for maternal health promotion | 11% | 7% | 13% | 0.77 (0.441) |
Table 1: Characteristics of the VHW by VHW recruitment cohort.
Feedback on the VHW training
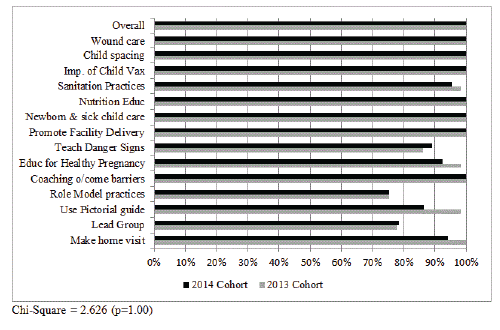
Each VHW was asked to rate how well the training prepared them for the specific daily tasks. As shown in Figure 1, 100% of both cohorts indicated that the training was useful or very useful overall. Across all skill-competencies, there were no significant differences in the proportions of VHWs feeling the training was useful (Chi-Square = 2.626, p=1.00). Almost all (90% or more) of both cohorts said that 10 of the 14 topics were useful.
The 2014 cohort received additional training on teaching about danger signs, and this is evident in the higher utility they gave this topic, but they found the modules on educating for a healthy pregnancy, using the pictorial guide, and making a home visit less useful than the 2013 cohort (Figure 1).
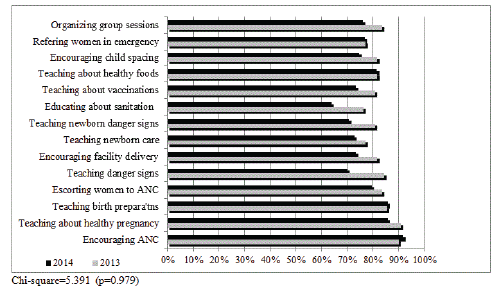
Figure 2 shows that by the end of 2014, 75-80% of the VHWs in both cohorts were comfortable performing 14 specific tasks (Chi square= 5.391, p=0.979). Ninety percent or more were comfortable encouraging ANC visits and teaching about a healthy pregnancy, and 80% or more were comfortable teaching about healthy foods during pregnancy and birth preparations. The 2013 cohort were somewhat more comfortable performing the other tasks, reflecting the additional year of experience they had, as compared to the 2014 cohort (Figure 2).
Feedback from the VHW on their activities
VHWs reported that they were expected to maintain contact with an average of 29 families, but in fact they saw many more, an average of 44 families. As shown in Table 2, the 2013 and 2014 cohorts differed in how they managed their work and in what they got out of mentoring and supervision (Table 2).
| 2013 Cohort | 2014 Cohort | ||
|---|---|---|---|
| Activity Feedback | (n=109) | (n=147) | t-test (p) |
| Home visits and educational activities | |||
| Hours per week | 22.1 | 19.8 | 0.829 (0.408) |
| Home visits per week | 14.4 | 10.7 | 1.419 (0.155) |
| Pictorial guide used a great deal | 83% | 77% | 1.300 (0.195) |
| Uses role plays and demonstrations to coach on health practices | 74% | 70% | 0.184 (0.854) |
| Organized well-attended group sessions | 78% | 69% | 1.460 (0.073) |
| Supervision and monitoring | |||
| Fill out and use the tally sheet to keep track of visits | 81% | 85% | 0.218 (0.828) |
| Met weekly with CHEW | 62% | 82% | 1.932 (0.054) |
| Mentoring has helped | 100% | 85% | 4.382 (<.001) |
| CHEW mentor is supportive | 89% | 83% | 1.651 (0.099) |
| Often meet as a team | 98% | 84% | 3.189 (0.016) |
| Supervised by in-charge or midwife monthly | 69% | 80% | 2.716 (0.007) |
| VHW can see how their own work helps the midwife | 91% | 80% | 2.497 (0.013) |
| VHW contributions are recognized by PHC team | 40% | 44% | 3.155 (0.002) |
| VHW Feedback on Work | |||
| Chi-square (p) | |||
| Most rewarding part of the work | 5.30 (0.623) | ||
| Seeing more women going for ANC | 17% | 23% | |
| More women delivering at the facility | 26% | 23% | |
| Men supporting wives to go to the clinic | 14% | 15% | |
| Support from the community for health improvements | 10% | 13% | |
| Chi-square (p) | |||
| Most difficult part of the work | 10.44(0.165) | ||
| Delays in paying stipend | 27% | 26% | |
| Facility not up to standard | 15% | 12% | |
| Transport and getting around | 16% | 9% | |
| Making time for visits | 11% | 13% | |
| Overall Feedback | |||
| Community thanks me for my work | 100% | 100% | NA |
| Would continue as VHW | 100% | 100% | NA |
| Nigeria should continue to have VHWs | 100% | 98% | 1.332 (0.184) |
Table 2: Feedback on activities by recruitment cohort.
Home visits: Although both cohorts worked around 20-22 hours per week, the more experienced VHWs (2013 cohort) managed to make 14.4 home visits per week, compared to 10.7 for the 2014 cohort (t=1.42, p=0.155). While not quite a significant difference, the pattern suggests that with experience they learned how to use their time more effectively. In addition, they had already built a rapport with many of the women, so visits could be shorter and more focused. Regardless of their recruitment year, they knew how to build a trusting relation with women. Most (77%) knew they were welcome when greeted upon arrival and/or the client shows that she likes talking to the VHW (70%). The greatest difficulties in making home visits were difficulties getting to the homes (with roads, mud or rain) (51%) and families not being home (36%). No one reported not being welcomed, and only 3 VHWs experienced disapproval from the husband.
Maternal health promotion: As shown in Table 2, the majority of both cohorts used the pictorial guide a great deal (t=1.30, p=0.195) The slightly higher usage rate among the 2013 cohort could reflect their greater experience and familiarity with the pictorial guide. In the focus groups, the VHW observed that the guide made it easier to explain things to women. For instance, one VHW remarked that the pictures of well-nourished children drew comments from the mothers, which enabled them to start a conversation about nutrition. Most VHWs reported that the pictures of danger signs were usually very important in teaching the women, particularly the pictures of maternal complications for getting the message across about serious complications.
One VHW remarked that the pictures of a woman with premature rupture of membranes and bleeding always drew out comments from the mothers, and this made it easy for the VHW to start a conversation about delivery in the facility. Indeed, 64% of the VHWs said that the pictorial guide was the most useful technique for encouraging women to go for ANC and deliveries at the PHC, followed by role modelling, sharing the VHW’s own experience (55%) and talking about difficulties other women in the village faced that might have been prevented (45%). Three-fourths of the VHWs, regardless of cohort (t=0.184), reported using role plays and demonstrations to teach about nutrition or sanitation practices such as hand washing. Significantly more (78%) of 2013 cohort reported being able to organize and mobilize good attendance for group education sessions, which also may reflect their greater experience and familiarity with the community. Only 69% of the newer cohort of VHWs were able to organize well-attended group education sessions (t=1.46, p=0.073).
Feedback on mentoring by the CHEW
Although the VHW were expected to meet with their CHEW mentor weekly, more of the 82% of the 2014 cohort managed weekly meeting than the 2013 cohort, among whom only 62% had weekly supervision (t=1.93, p=.054) (Table 2). The failure to meet weekly was not for lack of benefit, but primarily because these were not possible or very difficult in terms of cost or time (67% and 61% of the 2013 and 2014 cohorts, respectively). Despite the difficulties of making weekly supervision visits, more of the 2013 than 2014 cohort (100% vs. 85%, t=4.38, p<.001) found mentoring to be helpful, and more of the 2013 cohort than the 2014 cohort that their CHEW mentor was supportive, 89% vs. 83% (t=1.65, p=0.99). In the focus groups, the VHWs said they welcomed the opportunities to meet as a group, because then they could support each other to learn how to work better. The VHWs’ suggestions for the mentor were to be more practical in their teaching and mentoring, less formal and more patient, friendly, and empathic. Twelve percent of the VHWs wanted mentoring to be more educational and less about the number of visits. They liked when the CHEW mentor came to the community, as this demonstrated how the facility was supporting them and contributed to building respect for them in the community.
The VHW were particularly appreciative of the opportunity to meet with the PHC team, as this provided an opportunity for the VHW to be supervised by the in-charge and midwife. The team meetings and supervision by midwives varied between the two cohorts. The 2013 cohort reported more frequent team meetings, 98% vs. 84% (t=3.19, p=0.016).
This may be related to the differences between the cohorts in the proportion reporting that they can see how their work helps the midwife, 91% for the 2013 cohort compared to 80% for the 2014 cohort of VHWs (t=2.72, p=0.007). While the VHW can see how they help the midwife, the appreciation does not appear to go both directions, as fewer than half of the VHWs reported being thanked by the PHC team for their contributions.
The CHEW feedback on the mentoring process also was very positive about their visits to the community to meet with the VHW in their homes. They felt this was an important part of getting to know the VHW and see how they were working. They also pointed out that it was important that they were women themselves, as this enabled them to be welcomed into the VHWs’ homes and by women’s groups. The VHWs suggested that if the CHEW were from their own LGA or state, they would understand better the local customs and context for the VHW’s work.
Feedback on support from the community
As shown in the bottom section of Table 2, 100% of the VHWs were thanked by the community for their work. The focus groups provided additional insight to how the community welcomes them. One VHW said that when she makes visits, women “put their house in order, and leave their work to talk with me as soon as I come.” Half (47%) reported that people came to them with questions and asking for help. A majority (61%) said they felt respected. They also received thanks, though less frequently, from the Ward Development Community (WDC) (29%) and the PHC facility committee (12%). They reported that the WDC thanked them for their contribution to improving the community’s health.
Rewarding and challenging aspects of their work
One-fourth of the VHWs said that the most rewarding part of their work was seeing more women going for ANC and delivering at the facility, and the next most rewarding part of the work was seeing men supporting their wives to go to the clinic for care for themselves or their children.
About one in ten VHWs also said that it was rewarding to receive support from the community for their contributions to health improvements. There were no significant differences between the 2013 and 2014 cohorts in the aspects they found rewarding.
One-fourth of the VHWs also reported that the most difficult part of their work was delay in payment of their stipend. About one in twelve were bothered by making referrals for care to facilities that were not up to standard, and others found it difficult to make time for home visits. Paying for transport was a problem for 16% of the 2013 cohort and 9% of the 2014 cohort.
The WDC, the CHEWs and the In-Charges echoed this concern in their interviews, suggesting that the stipends should be higher in order to cover costs the VHW incurred in paying for transport to make visits to families located at some distance or to come to the PHC for supervision/mentoring. As for the most rewarding parts of their work, there were no significant differences in the overall pattern of aspects they found most difficult.
Despite these challenges all the VHWs said they wanted to continue to be a VHW, and were unanimous in their support for Nigeria to continue to have VHWs like themselves.
Monthly activities of the VHWs
The VHW tally sheets collected by the CHEW mentors for the 2013 cohort of VHWs for May 2013 to April 2014 showed that the VHWs worked an average of 20.8 hours per week. They averaged 34.3 home visits per month, of which 18.3 were educational, where they used the pictorial guide to talk about maternal and child health care practices and the balance referrals or quick checks on the family.
They identified 11.7 newly pregnant women per month, and documented 9.0 visits made for ANC based on their referrals or escorts. During repeat visits to women, they encouraged 7.3 women to go for their fourth ante-natal care visit. The VHWs reported helping 4.8 women per month proceed to the health facility for their delivery, and they also visited with women after a home delivery, averaging 6.3 post-partum visits.
Regardless of where the infant was born, the VHW averaged 8.8 post-natal visits per month. Their effectiveness at promoting facility deliveries increased over time. In the second six months of their work, the VHW facilitated 4.3 for every 10 deliveries at the facility, up from 3.2 per 10 deliveries in the first six months of their work, a 35% increase.
Impact of VHW activities on PHC consultations
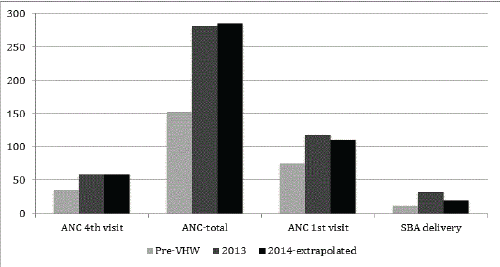
Comparing 2012 before the VHW began their home visits to 2013 after they began making visits, maternal and child health consultations increased significantly by 50% or more, with the percentage increase from 2012 to 2013 ranging from 56% for all antenatal care visits to 173.8% for skilled birth attendance of deliveries. (Table 3, all paired sample t-tests significant at <.10 level).
We do not have data for the entire period of 2014, but based on an extrapolation by 1.5 times to the consultations reported for the first six months of 2014, the increases in consultations at the PHC being supported by the first cohort of VHWs continued through 2014, with additional significant increases in all four measures of clinical consultations at the primary health center (Table 3).
Discussion
As Nigeria prepares its national VHW strategy, it is critical to recommend a strategy that has been proven effective and feasible for scale-up at a national level in Nigeria. The SURE-P MCH VHW program provided an excellent opportunity for such a pilot, with its national roll-out of 6000 VHWs in 2013 - 2014. We looked at the question of feasibility from the bottom-up, namely whether this national program was working at the local level in three northern states. We began by getting feedback from the VHWs on their training and activities, then went up the ladder to document how the VHWs were working from their supervisor/mentor’s and community’s perspective, and finally whether the home visits and meetings held by the VHWs actually contributed to improved utilization of maternal health services at the PHC to which the VHW were affiliated.
| 1st ANC | ANC 4th visit | ANC-total | Skilled birth attendant SBA | |
|---|---|---|---|---|
| 2012 Pre VHW | ||||
| Jigawa | 11,237 | 4,096 | 23,646 | 1,878 |
| Katsina | 6,498 | 5,610 | 14,468 | 1,313 |
| Zamfara | 4,047 | 567 | 5,999 | 309 |
| Total | 21,782 | 10,273 | 44,113 | 3,500 |
| 2013 VHW | ||||
| Jigawa | 15,194 | 6,245 | 35,127 | 4,327 |
| Katsina | 9,387 | 8,211 | 27,171 | 3,199 |
| Zamfara | 9,396 | 2,467 | 18,624 | 2,058 |
| Total | 33,977 | 16,923 | 80,922 | 9,584 |
| % Change | 64.7% | 83.40% | 56.00% | 173.80% |
| t-test (p) | 2.11 (0.079) | 2.13 (0.077) | 2.14 (0.076) | 2.13 (0.077) |
| 2014 VHW- 6 months | ||||
| Jigawa | 7,841 | 3,607 | 21,490 | 1,609 |
| Katsina | 5,984 | 5,265 | 17,953 | 1,327 |
| Zamfara | 7,524 | 2,448 | 15,286 | 938 |
| Total | 21,349 | 11,320 | 54,729 | 3,874 |
| 2014 VHW est @ 1.5X first 6 months | ||||
| Jigawa | 11,762 | 5,411 | 32,235 | 2,414 |
| Katsina | 8,976 | 7,898 | 26,930 | 1,991 |
| Zamfara | 11,286 | 3,672 | 22,929 | 1,407 |
| Total | 32,024 | 16,980 | 82,094 | 5,811 |
| % Change 2012-14 (2013 vs. 2014x) |
65.30% | 86.10% | 47.00% | 66.00% |
| 2.01 (0.091) | 1.94 (0.100) | 2.04 (0.088) | 2.09 (0.082) | |
| t-test (p) | ||||
Table 3: Annual consultations to the PHC associated with the VHW by year of recruitment.
At all these levels, there was strong evidence that the program was working: the Ward Development Committees recruited women who were respected and welcomed in the community, the training provided by the CHEW mentors prepared the VHW for the 14 specific tasks included in their scope of work, the mentoring by the CHEWs was well received and helped the VHWs improve their work, and the community’s women responded to their visits with an over 50% increase in maternal care visits and deliveries taken at the facility.
The style and selection of topics for the 6-day training were well received, particularly after additional material on coaching about danger signs, healthy pregnancies and birth preparations was incorporated into the 2014 training. They reported learning the most from role plays, practice home visit, and the training on using the pictorial guides.
The pictorial guides were considered the most important material they received. Across both training cohorts, there is still a need to improve the training on using role plays to coach on health promotion topics and on leading group education sessions. Even without these improvements, this study suggests that the same basic training be maintained as Nigeria transitions to a national VHW program.
The success of the training is demonstrated by the confidence that the VHWs express about performing their tasks. By the end of 2014, over three-fourths of the VHWs had become comfortable performing the wide range of tasks involved in their home visits and group sessions with women in the community.
The 2013 VHWs cohort were somewhat more comfortable than 2014 cohort in performing the various tasks for which they are responsible. We believe this reflects the importance of experience gained in the year that they have been serving as VHWs. In addition, the increased comfort level reported by the 2013 cohort may reflect the positive feedback that the community’s women were bringing back about the positive experiences they had at the PHC.
Thus, a key recommendation is to maintain the expected service period of two years, and to maintain support to the VHWs so that they are motivated to complete two years of service as a VHW. This recommendation is further underscored by the greater efficiencies achieved by the more experienced VHWs.
While they worked approximately the same amount of time, the more experienced cohort (2013) made more home visits than the newer cohort, 14.4 versus 10.7 per week. This suggests that over time the VHW become more proficient at organizing their time and/or they are making more repeat visits to women who they know already, so that the visits are shorter.
Figure 3 plots the increases in annual consultation per VHW. Each VHW was associated with an increase from 155 to 285 ANC visits per year and from 12 to 34 deliveries attended by skilled birth attendants at the facility. The extrapolation of the first six months of data for 2014 suggests that these contributions to increased consultations were maintained throughout the second year of the VHW’s service (Figure 3).
This study also documented the high level of activity of these VHWs, averaging 21 hours per week. The VHW tally sheet specifically differentiates between education about maternal health and support in terms of a specific referral and/or escort of the woman to the clinic, and it appears that this is an important distinction that emphasizes the need to turn education into action. For every two educational visits, the VHW have documented one visit to the PHC. The VHWs reported a high level of interaction with women in the community, with each VHW identifying approximately 140 pregnancies per year, for which she made 108 ANC referrals, and later helped 60 women per year to proceed to the facility for their deliveries. The VHWs did not find the scope of work too great, and the tally sheets show that they are comfortable with the mix of outreach, coaching or health promotion, and referral/escort activities. This level of work and expectations should be retained in the national VHW program going forward.
The pictorial guide was used a great deal in their coaching, and they particularly liked using the pictorial guides to explain about danger signs and nutrition, but they also used role plays and demonstrations to teach about nutrition or sanitation practices. Both coaching methods should be retained in the VHW program, and the VHWs specifically asked for more training on role plays and communication techniques, such as using songs, which were introduced for the 2014 cohort. The more experienced cohort (2013) demonstrated more confidence in organizing group education sessions. To help the VHW with group education sessions from the start of their work, more training on leading group discussions could be included.
The CHEW mentor model for supervision appears to be working, as almost all the VHWs report that the mentoring has helped them and that their CHEW mentor is supportive. Several features of this system may have been the key to its success. The following characteristics of the CHEW mentors contributed to the establishment of a good rapport with the female VHWs: that the CHEW mentor was also female, lived in or near the VHW’s community, had training in providing supportive supervision and, importantly, showed her respect for the VHW. CHEW mentor visits to the WDC, especially with the midwife, legitimise the work of the VHW. Such joint meetings should be encouraged, as this is how the community gains perspective on the work of the VHW, as well as how they can provide support to her.
The feedback from the VHWs on the CHEW mentoring suggests that there is a need to consider how the mentoring can evolve over time. The VHWs want less monitoring focused on the numbers and more interactive and educational mentoring. Part of what appears to be working is for the VHW to meet with midwife and the entire PHC team. The 2013 cohort reported frequent meeting as a team, and this may also be linked to a greater understanding of how their own work supports the midwife. Direct interactions with the midwife and in-charge also are welcomed. The VHWs would like more of a two-way interaction, with more recognition of their work. They feel that they receive great recognition from the community, but not from the members of the PHC team.
The impact of the VHW home visits is apparent in the 50% or greater increase in ANC consultations and facility-based skilled deliveries after the VHW commenced their work. While their education and reminders are very important to prompting behaviour change, being from the same community as where she is working enhances trust in the VHW, and this undoubtedly contributes to the rapid response to her visits and messages. The VHW had a high social standing when selected, and were nominated by the WDC. Most already had experience working as volunteers in the community, thus they were already respected. Their training and remuneration not only increased their skill level but also the level of respect they were likely to receive in the community. This is consistent with other studies showing a high degree of responsiveness to CHWs working in their own communities [13].
The VHW activities were associated with increases in maternal health consultations at the PHCs with which they were affiliated. Facility consultations for ANC visits (first, fourth, and total), and skilled birth attendance all increased by at least 50% compared to the period before the VHW began working. Skilled birth attendance increased by 173% from 2012 to 2013. While the increases in facility consultation rates could be associated with other changes besides the VHW visits, the VHW tally sheets reflect a level of referrals for ANC visits and facility deliveries consistent with the observed changes in facility consultations. These results are consistent with other studies in rural Ethiopia, Brazil, Pakistan and elsewhere showing an increase in facility consultations after VHWs began making home visits [3,13]. Indeed, it appears that the Nigerian VHW program may have been associated with larger increases in skilled birth attendance, perhaps because the SURE-P MCH Village Health Worker program also provided supervision and referral linkages with CHEWs and midwives posted to the rural PHC facilities.
This study has several limitations. It only included VHWs in three States in the Northern region. Although these States were thought to be representative of the Northern region of Nigeria, the analysis of data from all 36 states and the Federal Capital Territory (FCT) may reveal a different picture of the factors that enhance the work of the VHWs, as for example in other parts of Nigeria with different cultural compositions. Other limitations may include reliance on data summary tools from the states and assumptions that VHW records were accurate. Any errors in the VHW tally sheets could introduce bias, e.g. by under-reporting or over-reporting of certain types of activities, or by misclassification of visit types. Another limitation was the lack of supervisory data for the 2014 cohort of VHWs. The PHC consultation data show an increase in impact at the facility level, but we cannot conclude that a higher level of VHW visits is a cause, let alone the only cause, for this difference. Future studies may benefit from inclusion of more states from different geopolitical zones. However, findings from this study are valid given various methods used to collect information as part of the research process, the training received by the field researchers, quality of data collection and analysis and similarities of findings to other related studies.
While the study was only conducted in three of thirty-six states, we believe that the findings have great applicability for the national VHW road map. The SURE-P MCH VHW program is already a national program, and this focused study shows that it is working at the local level. Many of the design features incorporated into the SURE-P MCH VHW program incorporate evidence-based recommendations for reducing maternal mortality. Our study has focused on the critical contribution of the VHWs in mobilizing women to seek out antenatal care and, more importantly, to plan for a facility-based delivery with a skilled birth attendant. Our results show that communities can nominate, train, and support the VHWs. The selective allocation of tasks to the VHW complemented by the CHEW mentoring and midwife support in the facility is feasible and well-accepted by the women, communities, and the PHC. When implemented with this balanced team approach, they hold promise for helping communities across the nation to reduce the burdens of maternal mortality.
Acknowledgements
The Women for Health Programme is funded & supported by UKAid from the UK Government, which we thank for its support. The program me is managed by Health Partners International (HPI), Save the Children International and GRID Consulting, Nigeria. The authors thank the SURE-P MCH program for its in-kind support to the study, including assistance in obtaining the consultation data, and also the many VHWs, CHEWS, and others who gave freely of their time to participate in this study.
References
- (2011) One Million Community Health Workers: Technical Task Force Report.
- Bhutta Z, Lassi ZS, Pariyo G, Huicho L (2010) Global experience of community health workers for delivery of health-related millennium development goals: A systematic review, country case studies, and recommendations for integration into national health systems. Global Health Workforce Alliance.
- Perry H, Zulliger R, Scott K, Javadi D, Gergen J (2013) Case Studies of Large-Scale Community Health Worker Programs: Examples from Bangladesh, Brazil, Ethiopia, India, Iran, Nepal and Pakistan.
- Ramsey K, Hingora A, Kante M, Jackson E, Exavery A, et al. (2013) The Tanzania Connect Project: a cluster-randomized trial of the child survival impact of adding paid community health workers to an existing facility-focused health system. BMC Health Serv Res 13: S6.
- Nigeria Demographic Health Survey 2013 (2014) National Population Commission Federal Republic of Nigeria Abuja, Nigeria.
- Campbell OM, Graham WJ (2006) Strategies for reducing maternal mortality: Getting on with what works.The Lancet 368: 1284-1299.
- Fapohunda BM, Orobatan NG (2013) When women deliver with no one present in Nigeria: Who, What, Where and So What? PLoS One 8.
- National Primary Health Care Development Agency (2012). The National Village Health Worker Program.
- Subsidy Reinvestment and Empowerment Program on Maternal and Child Health (SURE-P MCH) (2012) Programme Implementation Manual 2012-2015.
- Ambibola S, Okoli U, Olubajo O, Mohammed J. Abdullahi, et al. (2012) The Midwives Service Scheme in Nigeria. PLoS Med 9: e1001211.
- Okeke EN, Gilick P, Abubakar IS, Chari AV, Pitchforth E, et al. (2015) The Better Obstetrics in Rural Nigeria (BORN) Study: An Impact Evaluation of the Nigerian Midwives Service Scheme. Rand Corporation Publication, CA.
- Bamisaiye A, Olukoya A, Ekunwe EO, Abosede OA (1989) A Village Health Worker Programme in Nigeria. World Health Forum 10: 386-392.
- Bigirwa P (2009) Effectiveness of Community Health Workers (CHWs) in the provision of basic preventive and curative maternal, newborn and child health (MNCH) interventions: A systematic review. Health Policy and Development 7: 162-172
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 12752
- [From(publication date):
April-2016 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 11797
- PDF downloads : 955