Research Article Open Access
Implementing CenteringParenting in Well Child Clinics: Mothers’ Nurses’ and Decision Makers’ Perspectives
Deborah Ann McNeil*, J Cyne Johnston, Germaeline Van der Lee and Nicole Wallace
Alberta Health Services, Population Public and Aboriginal Health, Calgary, Canada
- *Corresponding Author:
- Deborah Ann McNeil
Scientific Director
Alberta Health Services Population Public and Aboriginal Health Calgary,
Alberta T2W 3N2, Canada
Tel: 1-403 616-2040
Fax: 1-403-955-0850
E-mail: debbie.mcneil@ahs.ca
Received date: July 28, 2016; Accepted date: August 22, 2016; Published date: August 29, 2016
Citation: McNeil DA, Johnston JC, der Lee GV, Wallace N (2016) Implementing CenteringParenting in Well Child Clinics: Mothers’ Nurses’ and Decision Makers’ Perspectives. J Comm Pub Health Nurs 2:134. doi:10.4172/2471-9846.1000134
Copyright: © 2016 McNeil DA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community & Public Health Nursing
Abstract
Objective: The purpose of this study was to explore perceptions of mothers, nurses and decision-makers involved in implemening CenteringParenting (CP) in two Public Health (PH) clinics.
Design: Families participated in Public Health Nurse (PHN) facilitated health assessments, parent-led discussions, and vaccination within a group space at six timepoints in their children’s first year of life. Following completion of the program, mothers, nurses, and decision-makers participated in focus groups or individual interviews to discuss their experiences in CP. Qualitative data, collected via open-ended questions, were recorded, transcribed, and analyzed. Themes and sub-themes were identified.
Results: Thirteen mothers, five nurses and four decision makers were interviewed. Mothers found the program valuable in meeting their need for peer and personal support, information, and skill development. Nurses, although enjoying the opportunity to participate in the CP model, experienced challenges with the group model. Decisionmakers identified the need for new ways of thinking.
Conclusion: The CP program provided benefits to new mothers beyond what they expected. PHN facilitators experienced conflicts with standard practice, but were committed to making it work. Addressing logistical challenges will be required prior to expansion.
Keywords
Women's health; Public health systems; Patient perspective; Postpartum; Qualitative research; Vaccination
Introduction
Background
The future health of a nation relies on the health of its children; and families have a key responsibility in providing for the health and wellbeing of their children [1]. Health professionals contribute to the health of children and their families by providing expert guidance and assistance [1]. The CenteringParenting (CP) model is a vehicle to support maternal and infant health in the first year of life [2]. The model offers well-baby and mother care in a group situation during a child’s first year of life. The purpose of this study was to explore the perceptions of mothers, nurses, and administrators following implementation of the CP group care model and to inform planning for expansion of the model.
The current PH model of service provision in Calgary Alberta includes 1:1 consultations, combining health counselling with mother and infant health assessments, and childhood vaccination. Recently, with an increase in number of childhood vaccinations, the time available for activities other than vaccination has decreased. Approximately 91% of Calgary children are seen annually at well-child clinics for their childhood immunizations in the first year, while historically fewer than 65% of new mothers report attending childbirth education and parenting classes in Alberta [3]. The CenteringPregnancy model through well child clinics may provide an important opportunity to reach more families and provide more early parenting learning and support when parents are already present for a health clinic appointment.
The Centering Health Care model, originally developed in the United States, has spread around the world including Alberta. The model includes three facilitated care components: health assessment, education and support within a group environment [4]. CenteringPregnancy, the first Centering model developed, has been extensively studied and outcomes include reduction in preterm birth [5]; very low birth weight [6]; low birth weight plus preterm birth [7-10]; higher rates of breastfeeding initiation [11,12] and duration [13]; improved parenting knowledge [7,14] and psychosocial outcomes [15]. In addition, there was reported higher satisfaction in attendees compared to usual prenatal care [8,16,17]. In contrast to CenteringPregnancy, we are aware of only one publication available on the CenteringParenting model, which describes the implementation challenges and successes from interviews with program leaders conducted with 15 programs across multiple sites [2]. However, a systematic review and meta-analysis of group parent training programs found that there were short-term decreases in maternal depression, stress, anxiety, anger, parenting confidence and partner satisfaction with parenting stress remaining low and confidence remaining high six months after the program [18]. A Cochrane review, that examined group parenting programs and their impact on infant and toddler outcomes, reported that these programs have potential to improve emotional and behavioural development [19]. While group parenting programs provide novel ways of improving the health of mothers and infants, more research is needed prior to advocating for specific parenting interventions to improve child and parent health [18-20].
Intervention
A team, consisting of Alberta Health Services (AHS) researchers, maternal child PH experts and administrators modified and pilot tested a new CP well child care delivery model at two PH clinics; one clinic situated in a metropolitan setting and the other situated in a suburban/rural setting. Families attended two hour CP group sessions at the approximately one, two, four, six, nine, and twelve month infant birthdays (six times), with up to seven other families instead of the traditional four, 1:1 sessions at two, four, six and twelve months. Sessions, within a group space, included a short 1:1 infant and maternal assessment, a parent-led group conversation, and vaccination. The group discussions, often called circle time, were facilitated by two PHNs and provided an opportunity for peer support, education, health promotion and referral to resources as needed. There was stable group composition throughout the sessions.
Research Question and Methods
Design
This study is the qualitative component of a quasi-experimental pilot study to examine implementation and outcomes of the CP program. The methods and results of the quantitative component can be found in a companion paper previously published [21]. The research question that guided the qualitative interviews and analysis was: What were mothers’, facilitators/nurses’, and decision-makers’ experiences of the CP program as implemented in a well-child PH clinic setting?
Perceptions of participants were explored to gain an in depth understanding of their experience and their perceptions of successes and areas for improvement. Focus groups and individual interviews were used to collect data from mothers, nurse facilitators (PHNs) and decision makers/administrators. Interview questions, specifically developed for this study, were open-ended and general to allow for further probing of participant responses; for example, questions such as, “What did you like the best?” and “What stands out the most?” were questions included in all interviews. The University of Calgary Conjoint Health Research Ethics Board Ethics ID # REB13-0413 provided ethics approval.
Sample
All 22 mothers who participated in the CP programs at either site were invited to participate in interviews. Focus groups were scheduled at program sites and by phone or in person for individual interviews. Focus groups ranged from 90 to 120 min, while individual interviews ranged from 45 to 60 min.
Five PHNs, with experience ranging from 7 to 24 years and who worked at one of the two PH clinics, facilitated the CP group sessions. All PHNs received two days of CP-specific training. All five were recruited to take part in individual interviews. Four administrators, who participated in adpating and implementing CP, were also invited to participate in individual interviews.
Analytic strategy
Conventional qualitative content analysis was used to examine the audio recorded, and transcribed data from the interviews and focus groups. Data collection and analysis occurred simultaneously to permit follow-up of ideas that emerged from the data. Inductive analysis occurred in three phases: coding, categorizing and developing themes [22]. One of three qualitative investigators each led the analysis for a particular group (mothers, facilitators, or decision-makers) and then met together to verify themes and their descriptors for each group of participants. Themes were presented to facilitators, decision-makers and the remaining investigative team for verification.
Results
Parent interviews
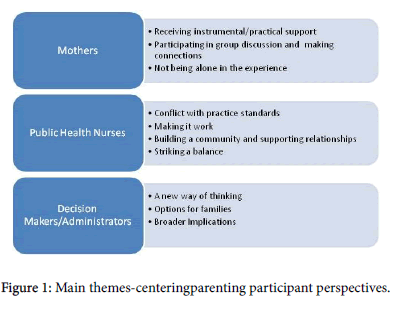
Thirteen first time mothers took part in one of three focus groups or three individual interviews. The sample for the qualitative study was similar to the full sample who participated in CP. The majority of women were between the ages of 24 and 34 years, all had a partner and most had some education beyond high school. Three major themes emerged: receiving instrumental support; participating in group discussions and making connections; and not being alone in the experience (Figure 1). Demographic information of the full and focus group sample of CP participants is available in Table 1.
Receiving instrumental support was expected and welcomed. Personal practical support, such as the convenience of having prescheduled vaccination times, made the program attractive as well as provided a diversion from being at home alone. Having a set appointment and schedule for the entire year, so as to just have to “… show up and not worry” contributed to participation. Attending group sessions also contributed to gaining of skills, knowledge, and information. Content specifically focused on their children’s growth and development as well as postpartum depression was important and valuable. A finding that was surprising was that CP reinforced decisions to vaccinate in an environment where the value of vaccination in childhood is questioned: “…you hear so much negative that you don’t really know if what you are doing is right….but seeing other mothers doing it as well made me feel a lot more comfortable.” Women enjoyed weighing and measuring their infants and this contributed to an understanding not available in other models of well child care as one mother stated, “I wanted to do it myself…rather than somebody telling you ‘ok, it’s like the 60th percentile’, didn’t mean anything to me before I was actually able to chart it myself…being able to interpret that information on your own is really helpful.” Women particularly valued the information and knowledge gained from each other: “to hear what other mothers were doing and what worked and what did not work…to have four or five different opinions was nice.”
| Characteristic | Full Sample | Focus Group Participants |
|---|---|---|
| n (%) | n (%) | |
| Maternal Age at Delivery | ||
| 19-24 | 5 (21) | 3 (23) |
| 25-34 | 14 (58) | 8 (62) |
| 35+ | 5 (21) | 2 (15) |
| Total | 24 | 13 |
| Marital Status | ||
| Married/Common law | 24(100) | 13 (100) |
| Total | 24 | 13 |
| Education | ||
| High school or less | 6 (25) | 4 (30) |
| Some or completed university/college | 15 (63) | 8 (62) |
| Some or completed grad school | 3 (12) | 1 (8) |
| Total | 24 | 13 |
| Ethinicity | ||
| Caucasian | 19 (79) | 12 (92) |
| Non-Caucasian | 5 (21) | 1 (8) |
| Total | 24 | 13 |
| Born in Canada | ||
| Yes | 21 (88) | 12 (92) |
| No | 3 (12) | 1 (8) |
| Total | 24 | 13 |
| Household Income | ||
| $40,000 - $69,000 | 5 (23) | 2 (18) |
| $70,000-$99,000 | 10 (48) | 5 (46) |
| $100,000 or more | 6 (29) | 4 (36) |
| Total | 21 | 11 |
Table 1: Demographic information of the full CenteringParenting sample and focus group participants.
Participating in the group discussion and making connections with each other and the PHNs was an identified need and CP sessions were highly anticipated, for both sharing “So it was nice to sit down with ladies that really do know where you’re coming from and can give you input and advice as well.” and the “expertise” and “insight” the nurses provided. The group sessions were “invaluable” where “… the group allowed us to sort of address how we were feeling” and as one mother said “What stood out the most was the support I received.” In the end, it was “about creating connections with new moms right?” A key element was the sharing and discussions, where mothers felt their participation was not only for their children but also for themselves: “Yeah it’s just like everybody is here for each other… such a good experience.” “Like sitting around and chatting about how everything was happening in your life and just reflecting on it and sharing the experience, that was more valuable to me than just the vaccination part of it.” The group sessions were thought to reduce the symptoms for post-partum depression for one mother: “I think if I didn’t have this group to come to and talk about everything and get it out I might have slipped more into the depressive side of things.” Becoming a mother in the 21st Century may place added pressure and burdens that are challenging compared to other eras; the benefits of participating in group models of care has the potential to mitigate some of these challenges of the current context of new motherhood. A perspective of this burden or pressure can be seen in the following: “…I think as moms we always have to present ourselves as like everything is great. But this is an opportunity to be honest and say, okay, like it’s not. Or like, it’s okay, I get emotional when I think about it. But I think we just go off and we just have to fake it a little.” The mothers participating in CP were able to be genuine in group and could be open and know that others in the group would understand, as one mother emphasized: “… [other] people just don’t want to hear that” when she described being up all night and the anxiety she experienced in taking care of her newborn and being a new mother.
Having mothers participate with infants at about the same age was considered important and contributed to feeling not alone in the experience: “For me it was anything that I was struggling with, that I was just talking to these ladies, okay, it is not just myself alone that I am facing with that problem.” The CP experience was ‘more’ in many ways as this mother stated: “I ended up getting so much more than what I was expecting.”
Nurse Facilitator Interviews
Five nurses were facilitators in the CP sessions and each participated in individual interviews. Four key themes emerged: Experiencing conflicts with standard practice; making it work; community and relationship building; and striking a balance.
Nurses experienced conflict with practice standards developed for individual care experiences while still valuing the intent of the program. Consideration of the model requirements with organizational practice standards was overwhelming for nurses: “it was stressful to try to fit everything in, in such a short time and safe manner and to make sure that we were meeting all of our standards of practice”. Nurses experienced challenges in following up with their other clients and felt this was hampered because of the additional adjunct activities required for CP such as planning group sessions and re-structuring the setting to facilitate interaction and maintain infant safety.
Despite feeling overwhelmed, the nurse facilitators were committed to making it work. The need to continuously plan, adjust and try to improve while always learning was a common perspective in all interviews, as nurses shared how they worked creatively to maximize the benefits mothers received from the program: “we just decided we were going to be creative and do what worked, what we had to, to do what worked for us and for our clients”. Nurses re-arranged the physical space, flow of the sessions and tailored group discussions to accomplish this objective. In addition, the nurses became immersed in the milieu of new motherhood and enjoyed the opportunity to be part of building a community and supporting relationships among the group. Attachments were formed among the mothers and also between the PHNs and mothers. Nurses enjoyed the opportunity to work more closely with each other and interacting with mothers in new ways: “we were chatting with our friends. It didn’t feel like work to me”.
Finally, striking a balance between immunization requirements, occasional inaccurate advice from mothers to their contemporaries, with group facilitation was a recurring theme throughout the interviews. Nurses felt obliged to provide accurate and meaningful information while at the same time addressing safety and administrative responsibilities; and also supporting mothers to share their experiential knowledge and their need to support and be supported by each other: “we want that socialization, but we needed some seriousness when it comes to child vaccination.”
Decision Maker Interviews
Four administrators, who participated in adpating and implementing CP, were interviewed upon its completion. These decision makers took a broader perspective of the program and model in the context of the health system and identified key factors to consider for future uptake and spread. Three themes that aligned with and complemented both the nurses’ and mothers’ perspectives were: A new way of thinking, options for families, and broader implications.
Decision-makers’ experience in the pilot provided them with an opportunity to reconsider programming and service delivery for maternal child health; and generated a new way of thinking, as one administrator said: “It really changed the way [we] look at how we support families, looking at things from a different approach, and recognizing that there aren’t always right and wrong answers, that there are always different ways of looking at things…”. The pilot also stimulated some to query current practices and standards: “[We need to] look at some standardized practices and [ask] truly are they best practice? Are they mandatory?” This reflection contributed to further exploration of assumption about the way care and service delivery were provided. The administrators recognized that their organization could contribute to rigid interpretation of standards. The flexibility needed to provide this group care model was not consistent with their current reality.
The pilot provided an opportunity for decision-makers to contemplate multiple options for families and to better understand the limiting features of the present 1:1 well-child service delivery model. A new reality was contemplated where there was “potential of meeting the needs of clients in a different way”. The opportunity to offer CP was seen as an important option particularly for families with high needs or who have socially vulnerabilities. CP could potentially have a stronger impact by providing the peer and professional support these groups need.
As decision-makers translated key lessons from their experience with the pilot into future implementation planning, considering the broader implications was a prominent theme. Costs and efficiency was central to their deliberations. The program requirements for material and human resources were considered at odds with their present economic situation. Further exploration of the short and long term maternal and child outcomes of this model of care were considered important to more specifically identify the value and impact from a programmatic and service delivery perspective: “….At some point you need to look at it and say this might be a really absolutely excellent and beneficial model for the parents but is there value from a systems perspective in terms of the cost”; “…[we] need someone to say that this is a valued program.”
There was surprising consistency across the mothers, PHNs, and administrators/decision makers in recommendations arising from analysis of the interviews. The recommendations fall into five broad categories and include considering the broader implications, the need to develop partnerships, supporting facilitator further education and support, further adapting program structure and addressing challenging logistics. See Table 2 for details.
| Consider the broader implications | Costs need to be acceptable. Executive support will be harder to garner if the intervention is more resource intensive than usual care. |
|---|---|
| Consider merging with other perinatal and postpartum programs to increase opportunities to build relationships and enhance efficiencies. | |
| Health impact measurement and demonstration will be crucial for buy–in and should include parenting impacts as well as maternal and child health outcomes. | |
| Partnerships | Build and maintain partnerships with external agencies (physician group practices and volunteer organizations) and nurture internal champions to ensure long-term success. |
| Closely involve nurses and frontline workers in further program planning and organization to ensure the program will be consistent with guidelines and expectations. | |
| Facilitator education and support | Maintain the program within the scope of nursing, while ensuring that nurses receive ongoing facilitation support and training in managing group sessions. |
| Program structure | Add additional group sessions (i.e. non vaccination) to allow mothers more time for connecting; especially in the early stages of parenthood. |
| Extend the program to 18 months or implement some other form of follow-up to improve vaccination uptake in subsequent years and follow-up of developmental milestones. | |
| Consider more structured discussions (tailored to individual group needs) and alternative options for participating (e.g. written or emailed questions/follow-up that arise in between sessions). | |
| Reassess parent handbook and other resources to ensure utility. | |
| Logistics | Allocate more time per session to ensure vaccinations and discussion times are not rushed. |
| Consider having a dedicated space for running the program, possibly with a separate room for vaccination and/or private consultation; and safer space for children to explore. | |
| Implement a recording/charting system that is flexible and accessible to all. | |
| Ensure enough PHNs are trained and that two are available at all times to facilitate sessions. Continue to schedule the same nurses for each group to ensure consistency. |
Table 2: Feedback and recommendations garnered from the parents’, nurses’ and decision-makers’ interviews.
Discussion
The evidence generated from this qualitative analysis of the perspectives of mothers PHNs and administrators indicates that the CP program was valuable in meeting the instrumental and social support needs of new mothers in the 21st century. Mothers made connections that contributed to their not feeling alone and were beyond what they expected. At the same time the PHNs who facilitated the program were committed to making the program work while balancing their own and the mothers’ needs. The PHNs enjoyed their experience with the program while encountering some challenges but were able to build a community and support relationships in the group. Much like the administrators involved in the pilot, the nurses also felt that logistical issues encountered will need to be addressed before the model is recommended for expansion. Decision makers, who were stimulated to consider new ways of thinking, identified the program as an important option for families but also felt the need to consider the broader implications particularly related to human and financial resource needs. The recommendations proposed focus on the logistical challenges identified that would need to be addressed prior to broader implementation of the CP program in their context.
The findings of this study are consistent with previous implementation recommendations for CenteringParenting that noted implementation of the model calls for significant system changes and substantial team relationship building across providers [2]. Although our program did not include physicians providing medical care and was delivered by the same category of health professionals, relationship building among those health professionals and with administrators was considered valuable. Addressing the logistical issues was a prominent implementation recommendation for CenteringPregnancy from recent review of CenteringPregnancy outcomes [23], which aligns with the findings from the present study.
Findings for participants were also consistent with many of the themes identified in qualitative studies of CenteringPregnancy. Giving and receiving support is a consistent finding across studies [17,24-26]. Not being/feeling alone was a prominent finding in three qualitative studies of CenteringPregnancy [25-27]. The learning, knowledge, and skills gained described by the participants in this study has been verified in other studies [7,14,24-27]. Women experiencing more than they thought they would receive was the core theme from a phenomenological qualitative study of CenteringPregnancy [25] and this was also identified in the present study.
The experiences of the facilitators were not uncommon when considering the phases of change [28]. Although we interviewed the facilitators following completion of the study, their descriptions of their experiences were not dissimilar to those described in a study of midwives implementing CenteringPregnancy where they believed in the model and were hopeful, but also experienced more work and stress compared to providing traditional care [29]. Similar to the midwives, the PHN facilitators enjoyed the experience and became more relaxed over time as the groups took shape and solved the logistical issues they faced. Similar logistical challenges were identified in a study of barriers and facilitators of implementing group prenatal care across six urban sites in the United States [30]. The importance of a champion was prominent in that study and is a recommendation in our study.
Conclusion
There were many benefits to mothers from participating in the CP program including gaining knowledge, skills and support Facilitator PHNs experienced conflicts with standard practice, but were committed to making it work. Decision-makers identified that a new way of thinking will be required in the future in order to provide options for families while considering the broader implications of uptake, sustainability and spread.
Acknowledgment
We would like to acknowledge the financial support provided by the Alberta centre for Child Family and Community Research.
References
- American Academy of Pediatrics (2016) Bright Futures.
- Bloomfield J, Rising SS (2013) CenteringParenting: an innovative dyad model for group mother-infant care.J Midwifery Womens Health 58: 683-689.
- Alberta Reproductive Health: Pregnancies and Births (2004) Alberta Health and Wellness. Reproductive Health Report Working Group.
- Reid J (2007) CenteringPregnancy: a model for group prenatal care.NursWomens Health 11: 382-388.
- Tandon SD, Colon L, Vega P, Murphy J, Alonso A (2012) Birth outcomes associated with receipt of group prenatal care among low-income Hispanic women.J Midwifery Womens Health 57: 476-481.
- Tanner-Smith EE, Steinka-Fry KT, Lipsey MV (2014) The effect of CenteringPregnancy group prenatal care on gestational weight gain, birth weight and fetal demise. Maternal Child Health Journal18: 801-809.
- Ickovics JR, Kershaw TS, Westdahl C, Magriples U, Massey Z, et al. (2007) Group prenatal care and perinatal outcomes: a randomized controlled trial.ObstetGynecol 110: 330-339.
- Massey Z, Rising SS, Ickovics J, (2006) CenteringPregnancy group prenatal care: Promoting relationship-centered care. Journal of Obstetric, Gynecologic, & Neonatal Nursing 35:286-294.
- Picklesimer AH, Billings D, Hale N,Blackhurst D, Covington-Kolb S (2012) The effect of CenteringPregnancy group prenatal care on preterm birth in a low-income population. American Journal of Obstetrics &Gynecology 206:415-417.
- Jafari F, Eftekhar H, Fotouhi A, Mohammad K, Hantoushzadeh S (2010) Comparison of maternal and neonatal outcomes of group versus individual prenatal care: a new experience in Iran.Health Care Women Int 31: 571-584.
- Klima C, Norr K, Vonderheid S, Handler A (2009) Introduction of CenteringPregnancy in a public health clinic.J Midwifery Womens Health 54: 27-34.
- Trotman G, Chhatre G, Darolia R, Tefera E, Damle L, et al. (2015) The effect of centeringpregnancy versus traditional care models on improved adolescent health behaviors in the perinatal period. Journal of Pediatric Adolescent Gynecology 28:395-401.
- Ruiz-Mirazo E, Lopez-Yarto M, McDonald SD (2012) Group prenatal care versus individual prenatal care: a systematic review and meta-analyses.J ObstetGynaecol Can 34: 223-229.
- Baldwin KA (2006) Comparison of selected outcomes of CenteringPregnancy versus traditional prenatal care. Journal of Midwifery and Women’s Health 51: 266-272.
- Ickovics JR, Reed E, Magriples U, Westdahl C, Schindler Rising S, et al. (2011) Effects of group prenatal care on psychosocial risk in pregnancy: results from a randomised controlled trial.Psychol Health 26: 235-250.
- Robertson B, Aycock DM, Darnell LA (2009) Comparison of CenteringPregnancy to traditional care in Hispanic mothers. Maternal Child Health Journal 13: 407-414.
- Teate A, Leap N, Rising SS, Homer CS (2011) Women's experiences of group antenatal care in Australia--the CenteringPregnancy Pilot Study.Midwifery 27: 138-145.
- Barlow J, Smailagic N, Huband N, Roloff V, Bennett C (2014) Group-based parent training programmes for improving parental psychosocial health. Cochrane Database of Systematic Reviews.
- Barlow J, Smailagic N, Ferriter M, Bennett C, Jones H (2010) Group-based parent-training programmes for improving emotional and behavioural adjustment in children from birth to three years old. Cochrane Database of Systematic Reviews.
- Bryanton J, Beck CT (2010) Postnatal parental education for optimizing infant general health and parent-infant relationships. Cochrane Database of Systematic Reviews.
- Johnston JC, McNeil D, van der Lee G, Macleod C, Uyanwune Y, et al. (2016) Piloting CenteringParenting in two Alberta Public Health well-child clinics. Public Health Nursing 33: 9.
- Miles M.B, Huberman AM (1994) Qualitative Data Analysis. Sage Publications Inc., California.
- Tilden EL, Hersh SR, Emeis CL, Weinstein SR, Caughey AB (2014) Group prenatal care: review of outcomes and recommendations for model implementation.ObstetGynecolSurv 69: 46-55.
- Herrman JW, Rogers S, Ehrenthal DB (2012) Women's perceptions of centeringpregnancy: a focus group study.MCN Am J Matern Child Nurs 37: 19-26.
- McNeil DA, Vekved M, Dolan SM, Siever J, Horn S, et al., (2012) Getting more than they realized they needed: A qualitative study of women's experience of group prenatal care. BMC Pregnancy Childbirth12:17.
- Novick G, Sadler LS, Kennedy HP, Cohen SS, Groce NE, et al. (2011) Women's experience of group prenatal care.Qual Health Res 21: 97-116.
- Kennedy HP, Farrell T, Paden R, Hill S, Jolivet R, et al. (2009) "I wasn't alone"--a study of group prenatal care in the military.J Midwifery Womens Health 54: 176-183.
- Prochaska JO, DiClemente CC (1983) Stages and processes of self-change of smoking: toward an integrative model of change.J Consult ClinPsychol 51: 390-395.
- Baldwin K, Phillips G (2011) Voices Along the Journey: Midwives' Perceptions of Implementing the CenteringPregnancy Model of Prenatal Care.J PerinatEduc 20: 210-217.
- Novick G, Womack JA, Lewis J, StaskoEC, Schindler Rising, S et al. (2015) Perceptions of barriers and facilitators during implementation of a complex model of group prenatal care in six urban sites. Research in Nursing and Health 38:462-474.
--
Relevant Topics
- Chronic Disease Management
- Community Based Nursing
- Community Health Assessment
- Community Health Nursing Care
- Community Nursing
- Community Nursing Care
- Community Nursing Diagnosis
- Community Nursing Intervention
- Core Functions Of Public Health Nursing
- Epidemiology
- Epidemiology in community nursing
- Health education
- Health Equity
- Health Promotion
- History Of Public Health Nursing
- Nursing Public Health
- Public Health Nursing
- Risk Factors And Burnout And Public Health Nursing
- Risk Factors and Burnout and Public Health Nursing
Recommended Journals
- Epidemiology journal
- Global Journal of Nursing & Forensic Studies
- Global Nursing & Forensic Studies Journal
- global journal of nursing & forensic studies
- journal of community medicine& health education
- journal of community medicine& health education
- Palliative Care & Medicine journal
- journal of pregnancy and child health
Article Tools
Article Usage
- Total views: 11594
- [From(publication date):
August-2016 - Jul 11, 2025] - Breakdown by view type
- HTML page views : 10649
- PDF downloads : 945