Research Article Open Access
Implant Stability Measure: Critical Review of Various Methods
Saurabh G* and Rubina K
Axiss Dental Pvt. Ltd, Whitefield, Bengaluru, Karnataka, India.
- *Corresponding Author:
- Saurabh G
Axiss Dental Pvt. Ltd
Whitefield, Bengaluru
Karnataka, India
Tel: +91 9916203455
E-mail: saurabh.ravzz@gmail.com
Received Date: February 26, 2016; Accepted Date: July 18, 2016; Published Date: July 20, 2016
Citation: Saurabh G, Rubina K (2016) Implant Stability Measure: Critical Review of Various Methods. Dent Implants Dentures 1:110. doi:10.4172/2572-4835.1000110
Copyright: © 2016 Saurabh G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Dental Science and Medicine
Abstract
The prerequisites of a successful dental implant are the achievement and maintenance of implant stability. Implant stability may be well-defined as the lack of clinical mobility that is also described as osseo integration. As a mechanical phenomenon, primary implant at placement is associated with quantity and quality of the local bone, the kind of implant method and placement used. Secondary implant stability is related to the increased instability attributable to the formation of bone and to remodel it at the implant tissue interface and in the neighboring bone. Several ways are there to evaluate the implant stability like the periotest, cutting resistance’s clinical measurement throughout implant placement and reverse torque test. The aim of this article is to bring to light the different techniques of determining implant stability.
Keywords
Implant stability; Dental Implant; Periotest
Introduction
For functional implants, osseo integration is essential, and for successful osseo integration primary implant stability is essential. Implant stability refers to lack of clinical mobility. Implant instability might lead to fibrous encapsulation having resulting failure [1,2]. Being a mechanical phenomenon Primary implant stability is connected to local bone quantity and quality, the kind of implant and its placement method used. Secondary implant stability means the increased stability resultant of bone formation and restoration at the implant/tissue crossing point and in the adjacent bone. In well-defined situations, initial and instant loading protocols were recognized to be feasible substitutions to the traditional 1-or 2-state late loading methods. Consequently, the clinician requires supportive and dependable objective guiding principles for determining on an individual basis the diagnosis of a certain implant, in case loaded instantly, initially loaded within six to eight weeks or traditionally left to heal for a period of three to six months. Factually, the gold standard technique used for evaluating osseo integration’s degree was histologic or microscopic analysis [3,4]. Conversely, because of the insensitivity of such technique and associated ethical problems, numerous other techniques of analysis were suggested; resonance frequency analysis, using blunt ended instruments for clinically checking mobility, reverse torque, radiographs and cutting torque resistance. Assessing implant stability is supportive to taking good decisions regarding when to load, permits beneficial protocol selection on a patient-to-patient basis, and is indicative of situations wherein unloading is best, supportive to good communication and enhanced trust and offers better case records. The techniques of determining implant stability clinically are Periotest RFA, clinical perception, cutting torque resistance analysis, percussion test and reverse torque test [3-7].
Clinical perception
The clinical view of the primary Implant stability is often based on the mobility as identified by blunt ended instruments. This happens to be very unpredictable and non-objective technique. This may also be checked by observing implant’s cutting resistance while inserting it. The sensation of “good” stability can be stressed in case of sensing an abrupt stop at the implant’s seating. Tapered implants’ root forms repeatedly have a geometry which will offer a firm stop and probably a false sensitivity of high stability [7,8].
Percussion test
The percussion test may include a mirror handle’s tapping against implant carrier and is designed for causing a ringing sound from the implant as a sign of osseo integration or good stability. Percussion tests possibly offer more information regarding the tapping instrument, and at best merely produce poor qualitative information.
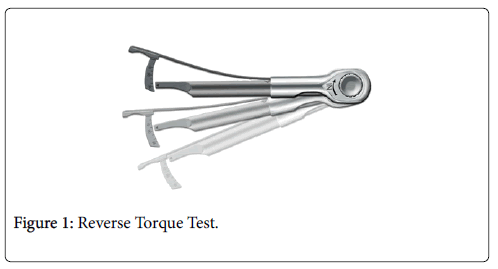
Reverse torque test
Applying an unscrewing or reverse torque test was also recommended for the evaluation of implant stability during abutment connection. Implants rotating under the applied torque are regarded as failures and therefore they are removed [9-11]. Conversely, in the process of osseo integration, the implant surface although gradually, can fracture because of the applied torque stress. Furthermore, as demonstrated by animal experiments the re-integration of rotationally mobile and loosened implants, the reverse torque test is disregarded (Figures 1 and 2).
Cutting torque resistance analysis
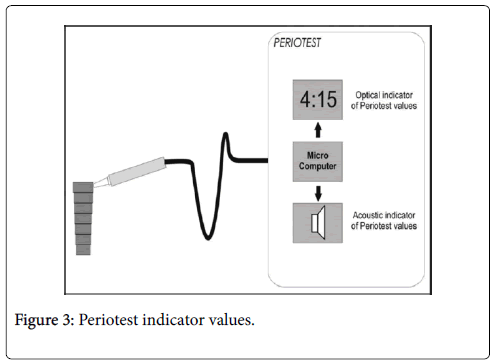
The energy needed for a current-fed electric motor to cut off a unit volume of bone in measuring implant surgery. The energy is correlated to density of bone that is one of the factors determining decisive in implant stability. Conversely, the value of lower limit is not established, that may indicative of the implant’s possible failure. Besides, only during surgery, it may be used as an analytic aid, and it cannot evaluate secondary stability by formation of new bone and restoration around the implant. Periotest is an electrically driven device and electronically supervised tapping head which percusses the implant for totally 16 times. The whole evaluation procedure requires about 4 s (Figure 3). The instrument comprises a tapping rod which impacts the implant/ abutment assembly. A Propulsion coil draws the rod towards the surface of impacting and fundamentally moves at a continuous velocity from the moment of its leaving the hand piece till the surface is impacted by it. It implies that at a given distance, the tapping rod that moves at the same velocity and is devised for impacting the surface any time in this travel of continuous velocity. The rod’s end inside the hand piece is strictly joined to an accelerometer, producing an output proportionate to its acceleration. The readings extracted are from -8 to +50 and are inferred as in Table 1. The issues influencing the periotest value are the hard tissue’s quality in the area of the implant, so that no particular values may be deemed as suitable to lower or higher degrees of integration. It is dependent on the spacing between implant flange and the point where the rod affects the abutment. Such variations propose that for implants, no absolute value is there which can be considered as acceptable; instead variation occurring in course of time can be more meaningful. In vitro assessments showed that no essential difference existed in evaluating periotest values from operator to operator, and repeatability of high level between various periotest units. Dental implants, integrated successfully have produced an extensive range of stability readings with the periotest. Such range in values is supposed to reproduce density of bone at the implant interface and is associated with implant location. The measurements are essentially affected by conditions of excitation like position and direction. The measurements should be made in the region of mid buccal and should perpendicular to axes of implant [10-14]. Taking into consideration the intra oral environment, it is substantially easy for making measurements on anterior implants while it is not likely for molars owing to the buccal mucosa. “An implant in the process of osseo integration” or a “borderline” case cannot be diagnosed by periotest. The level of peri-implant bone is not reflected by it and hence cannot be replaced for radiography.
| Reading | Interpretation |
|---|---|
| -8 to 0 | Osseo integration is good, loading of implant can be done |
| +1 to 9 | Examination is required, loading is not possible in many cases |
| +10 to +50 | Osseo integration is not completed, implant cannot be loaded |
Table 1: The readings extracted are from -8 to +50 and are inferred.
Resonance Frequency Analysis
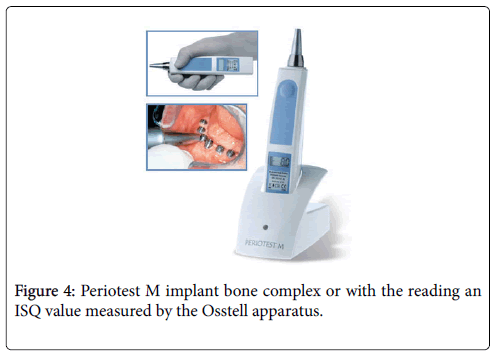
This is a non-invasive diagnostic technique which measures bone density and implant stability at different time points using structural and vibration principle study. For evaluation of implant stability two commercial devices were developed. The original technique makes use of a direct connection between the resonance frequency analyzer and the transducer. In the second technique, magnetic frequencies are used between the resonance frequency analyzer and transducer. In the electronic tool, an L shaped cantilever beam is the transducer connecting to the implant through a screw attachment. A piezoelectric crystal on the L beam’s vertical portion is used for stimulating the transducer complex/implant; second piezoelectric crystal on the beam’s opposite side is used as a receiving component for detecting the beam’s response. In the new magnetic RFA device, there is a sensor, a metallic rod having a magnet on top that is screwed on to an abutment or implant [12,13]. A magnetic pulse excites the magnet from a wireless probe. Duration of the pulse is approximately 1 ms. The peg freely vibrates after excitation and an electric voltage in the probe coil is induced by the magnet. That voltage is signal of measurement which is sampled by the resonance frequency analyzer. The magnetic device and the electronic device are able to measure similar changes; but the magnetic device leads to higher implant stability quotient value while measuring non-submerged dental implant’s stability. Implant stability is measured with this technique either by deciding resonance frequency of Figures 4 and 5.
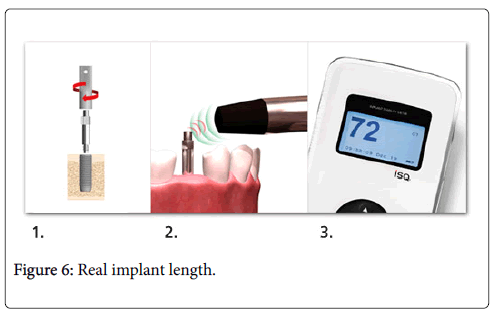
Figure 4 shows the periotest M implant bone complex or with the reading an ISQ value measured by the Osstell apparatus. Classically, the ISQ was seen varying between 40 and 80, the higher the ISQ, the higher implant stability. A considerable decrease or increase in implant stability might be detected with the help of this technique which otherwise might not be perceived clinically. The factors which affect the readings are efficient implant length, quantity and quality of bone, shape diameter and length of implant. Real implant length is the exposed threads’ length and height of abutment. Inversely, it is proportionate to the resonance frequency. Implant stability may be decided for implants having an ISQ of 47. All implants having an ISQ more than forty nine osseo integrated when left for healing for a period of three months. All implants with an ISQ more than fifty four osseo integrated while loaded immediately. For implants having low ISQ values, implant stability’s decrease must alert the practitioner for submitting such implants to a tighter follow-up agenda and to take extra protective measurements about unloading till implant stability is recovered or if non-loaded for checking for infection and/or mechanical trauma. In case of implants having high ISQ values, implant stability’s reduction in initial twelve weeks of healing must be regarded as common incident which must not need alteration in the routine follow-up. The disadvantages of this technology are that the transducer is restricted to a set of sixty measurements, therefore making the technique quite costly. A transducer is fixed to the implant to perform the RFA (Figure 6). This eliminates monitoring all implants which support a cemented renovation [14,15].
Conclusion
Though different methods are there that helps in determining implant stability, the number variable influencing the outcomes makes it difficult to arrive at a critical value that may determine an implant’s failure, success or long-standing prognosis. Therefore, further research is needed for devising a precise instrument is helpful in gauging the implant stability.
References
- Meredith N (1998) Assessment of implant stability as a prognostic determinant. Int J Prosthodont 11: 491-501.
- Brunski JB (1992) Biomechanical factors affecting the bone-dental implant interface. Clin Mater 10: 153-201.
- Nedir R, Bischof M, Szmukler-Moncler S, Bernard JP, Samson J, et al. (2004) Predicting osseointegration by means of implant primary stability. Clin Oral Implants Res 15: 520-528.
- Atsumi M, Park SH, Wang HL (2007) Methods used to assess implant stability: Current status. Int J Oral Maxillofac Implants 22: 743-754.
- The Implant Stability Quotient Whitebook: The Relationship between Reliable Diagnostics and Safe, Successful Dental Implant Procedures. (1stedn).
- Sennerby L, Meredith N (2008) Implant stability measurements using resonance frequency analysis: Biological and biomechanical aspects and clinical implications. Periodontol 2000 47: 51-66.
- Sullivan DY, Sherwood RL, Collins TA, Krogh PH (1996) The reverse-torque test: A clinical report. Int J Oral Maxillofac Implants 11: 179-185.
- Ivanoff CJ, Sennerby L, Lekholm U (1997) Reintegration of mobilized titanium implants. An experimental study in rabbit tibia. Int J Oral Maxillofac Surg 26: 310-315.
- Friberg B, Sennerby L, Roos J, Johansson P, Strid CG, et al. (1995) Evaluation of bone density using cutting resistance measurements and microradiography: An in vitro study in pig ribs. Clin Oral Implants Res 6: 164-171.
- Friberg B, Sennerby L, Meredith N, Lekholm U (1999) A comparison between cutting torque and resonance frequency measurements of maxillary implants. A 20-month clinical study. Int J Oral Maxillofac Surg 28: 297-303.
- Friberg B, Sennerby L, Gröndahl K, Bergström C, Bäck T, et al. (1999) On cutting torque measurements during implant placement: A 3-year clinical prospective study. Clin Implant Dent Relat Res 1: 75-83.
- Teerlinck J, Quirynen M, Darius P, van Steenberghe D, et al. (1991) Periotest: an objective clinical diagnosis of bone apposition toward implants. Int J Oral Maxillofac Implants 6: 55-61.
- Hürzeler MB, Quiñones CR, Schüpbach P, Vlassis JM, Strub JR, et al. (1995) Influence of the suprastructure on the peri-implant tissues in beagle dogs. Clin Oral Implants Res 6: 139-148.
- Valderrama P, Oates TW, Jones AA, Simpson J, Schoolfi eld JD, et al. (2007) Evaluation of two different resonance frequency devices to detect implant stability: A clinical trial. J Periodontol 78: 262-272.
- Meredith N, Alleyne D, Cawley P (1996) Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin Oral Implants Res 7: 261-26 7.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 15996
- [From(publication date):
December-2016 - Dec 22, 2024] - Breakdown by view type
- HTML page views : 14860
- PDF downloads : 1136