Case Report Open Access
Imperforate Hymen as Cause of Acute Urinary Retention
Carla Duarte1*, Inês Falcão Reis2, Rita Caldas2, Carla Pina2, Luísa Sousa2 and Humberto S Machado3*1Hospital of Senhora da Oliveira Guimarães, EPE, Gynecology and Obstetrics Service, Portugal
2Hospital Center between the Douro and Vouga, Gynaecology and Obstetrics Service, Portugal
3Porto Hospital Center, Anaesthesiology Service, Portugal
- *Corresponding Author:
- Humberto S Machado
Porto Hospital Center
Anaesthesiology Service
Portugal
Tel: 351935848475
E-mail: hjs.machado@gmail.com
Received date: May 03, 2017; Accepted date: May 16, 2017; Published date: May 20, 2017
Citation: Duarte C, Reis IF, Caldas R, Pina C, Sousa L, et al. (2017) Imperforate Hymen as Cause of Acute Urinary Retention. J Preg Child Health 4:324. doi:10.4172/2376-127X.1000324
Copyright: ©2017 Duarte C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
The imperforate hymen is one of the most frequent malformations of the female genital tract. The clinical presentation varies from the asymptomatic form to symptoms caused by the obstructive effect of the hematocolpometra such as primary amenorrhea, abdominal and lumbar pain, constipation, dysuria and urinary retention. We report the case of an adolescent whose only symptoms were acute urinary retention associated with severe pelvic pain.
Keywords
Imperforate hymen, Hematocolpos, Hematometra, Urinary retention
Introduction
The imperforate hymen is an obstructive anomaly of the female genital tract. The formation of the female genital tract begins at three weeks of gestation and continues throughout the second trimester of pregnancy. The hymenial membrane separates the vaginal lumen from the urogenital sinus.
Usually before birth, the epithelial cells of the central area of the hymenial membrane start the process of degeneration, with a thin border of the membrane consisting of fibrous connective tissue persisting around the vaginal opening [1]. An incomplete degeneration process can cause hymenial anomalies such as: imperforate, microperforated, cribiform or septate hymen. These morphological variants can be identified during gynecological examination. The estimated incidence of imperforate hymen is 0.014-0.1% [2]. Urinary retention is an uncommon symptom in children and adolescents and may result from urinary tract infection, neurologic conditions or mechanical obstructions such as renal lithiasis, urethral constrictions, external genitalia trauma and imperforate hymen.
In the presence of symptoms such as abdominal and/or cyclic lumbar pain, pelvic swelling, urinary retention or constipation in a premenarchal adolescent with a discrepant Tanner stage pubertal development, the diagnosis of imperforate hymen should be considered [3].
Case Report
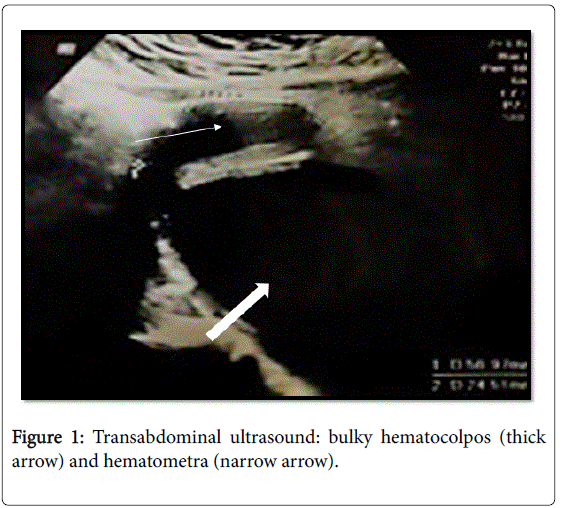
A 12 year old girl was taken to the emergency department with acute urinary retention associated with constant and intense pelvic pain within 12 h of evolution. There was not nausea, vomiting, change in bowel habits, fever or medication in progresso and her menarche had yet not occurred. At the physical examination, there was painful suprapubic pelvic swelling upon palpation. The secondary sexual characters were present and according to stage 4 of Tanner. The external genitals were inspected, showing an imperforate, bulging and translucent hymen. Bladder catheterization was performed and 1300 ml urine of suis generis characteristics was drained, with immediate symptomatic relief. On ultrasound, the vagina was distended by anechoic content, which was also filling the whole uterine cavity corresponding to bulky hematocolpos and hematometra (Figure 1).
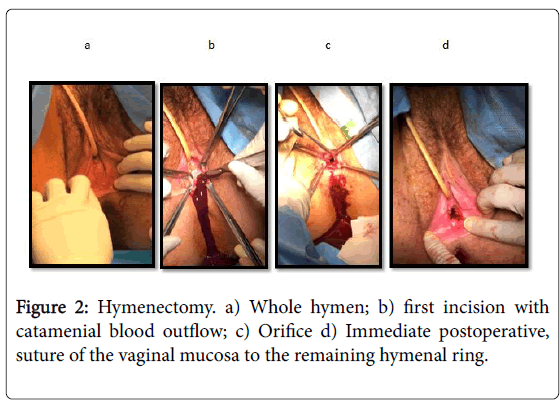
Blood tests showed no alterations, namely normal renal function. The treatment consisted of X-hymenotomy, with drainage of approximately 600 ml of collected catamenial blood (Figure 2). Excess hymenial tissue was excised and the vaginal mucosa was discontinuously sutured to the hymenial ring with vicryl® 3/0 in order to create an orifice allowing the passage of a finger to prevent recurrence and obstruction. The postoperative period was uneventful and she was discharged the day after the procedure. At the follow-up visit at 30 postoperative days she reported normal catamenium with 5 days duration and 26 days interlunion. At physical examination the remaining hymen was permeable. Informed consent was obtained for the publication of this clinical case and corresponding images.
Discussion
The imperforate hymen is a clinical entity of undetermined etiology, being the most frequent cause of hydrometrocolpos.
It is due to the absence of partial resorption of the hymenial membrane during the embryonic development and failure of its rupture in the perinatal period, the majority occurring sporadically [4]. Familial cases are reported, however, when they occur in isolation, no mutations or genetic markers were identified [5,6].
The American Society for Reproductive Medicine classifies Mullerian anomalies into six groups based on the clinical presentation and prognosis of a successful pregnancy after treatment. This classification excludes extra uterine anomalies and although it allows additional descriptions of vaginal, tubal or urinary abnormalities, it becomes complex. In order to overcome this limitation the classification of the ESHRE/ESGE was updated, allowing to classify this anomaly as U0C0V3 (U0 - normal uterus, C0 - normal cervix and V3 - vagina with transverse septum / imperforate hymen) [7,8].
Described as one of the most frequent obstructive lesions of the vagina, the hymen should be evaluated at birth, at which time the newborn may have salient hymenial membrane due to the presence of mucocolpos. When undiagnosed at this stage of life, the child usually remains asymptomatic until the age of menarche. At this time, the adolescent may have a history of pelvic or cyclic abdominal pain and hematocolpos. The distention caused by the retained catamenial blood may result in compression of the contiguous pelvic structures causing pain in the defecation, low back pain and urinary difficulty, being rare the occurrence of urinary retention. Presentation on the form of urinary retention is not frequent [9,10].
Prenatal diagnosis using obstetric ultrasound rarely occurs in the presence of fetal mucocolpos, hydrocolpos or hydrometrocols. Usually the ultrasound suspicion is confirmed with fetal magnetic resonance imaging [11].
The formation of the female reproductive system is strictly related to the development of the urinary system, which is why the presence of abnormalities of the genital tract usually imposes the exclusion of urinary pathology. However, due to distinct embryological origins, isolated anomalies of the hymen are not associated with renal abnormalities [4].
It should be noted that some anatomical abnormalities might reproduce the appearance of an imperforate hymen on physical examination. Thus the entities that make differential diagnosis with imperforate hymen are: obstructive or partially obstructive longitudinal or transverse vaginal septum, hymenial or vaginal cyst, hymen variants such as septate, in band or navicular hymen, vaginal agenesis, acquired adhesion of the lips and the syndrome of complete insensitivity to androgens [12]. The entities that cause obstruction to the catamenial blood exit are followed by urinary retention by the same mechanism.
Once the diagnosis is established, symptomatic treatment implies bladder drainage with immediate resolution of associated pelvic pain. The definitive treatment is surgical consisting of excision of the hymenial membrane tissue in order to create a normal-sized orifice (allowing the passage of a finger without resistance). The type of incision depends on the preference of the surgeon since they present the same risk of stenosis [13]. Suturing of the vaginal mucosa to the hymen ring using absorbable suture yarn at separate points is also dependent on the preference of the surgeon and the patient's desire to maintain intact hymen ring [14]. In order to prevent the formation of adhesions, some authors recommend the use of Foley balloon in the postoperative period for 2 weeks, however this technique it has not been widely used for both the discomfort provoked and the lack of evidence of its effectiveness [4].
Treatment can be performed at any age at the time of diagnosis, however it is considered that healing is optimized in tissues under estrogenic stimulation, thus reducing the risk of recurrence. In the absence of complications and hymenial bulging, when the diagnosis is made in the prenatal period, in the new-born or in the pre-pubertal child, it is recommended to delay the treatment until puberty, one year after the development of the mammary glands (Tanner stage 3 or 4), with hormonal environment favorable to healing [3].
Conclusion
In conclusion, the authors described a clinical case of acute urinary retention in adolescents with imperforate hymen complicated with voluminous colpometra and hematometra. Underline the inspection of the external genitalia of new-borns and infants should be an integral part of the routine physical examination. Faced with a urinary retention in premenarcheous girls it should be excluded the presence of imperforate hymen as an obstructive cause. Due to anatomical proximity, the accumulation of catamenial blood in the vagina causes progressive stretching or obstruction of the urethra. The degree of stretching up to the obstruction can lead to cyclic urinary symptoms, such as polaquiuria or acute symptoms such as urinary retention in the case presented.
References
- Lankford JC, Mancuso P, Appel R (2013) Congenital reproductive abnormalities. J Mid Womens Health, pp: 58-65.
- Nagai K, Murakami Y, Nagatani K, Nakahashi N, Hayashi M, et al. (2012) Life threatening acute renal failure due to imperforate hymen in an infant. Paediatrics Int, pp: 280-282.
- Marshall WA, Tanner JM (1969) Variations in pattern of pubertal changes in girls. Arch Dis Childh, pp: 244-291.
- Dietrich JE, Millar D Quint E. (2014) Obstrutive reprodutive tract anomalies. J Pediatric Adolec Gynaecol, pp: 396-402.
- Connell MT, Owen CM, Segars JH (2013) Genetic syndromes and genes involved in the development of the female reproductive tract: A possible role for gene therapy. J Genet Syndr Gene Ther 4: 127.
- Grimbizis GF, Gordts S, Sardo ADS, Brucker S, Angelis CD, et al. (2013) The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod 28: 2032-2044.
- Sardo DSA, Campo R, Gordts S, Spinelli M, Cosimato C, et al. (2015) The comprehensiveness of the ESHRE/ESGE classification of female genital tract congenital anomalies: A systematic review of cases not classified by the AFS system. Hum Reprod 30: 1046-1058.
- Salhan B, Omisore O, Kumar P, Potter J (2013) A rare presentation of imperforate hymen: A case report. Case Rep Urol.
- Sakalkale R, Samarakkody U (2005) Familial occurrence of imperfurate hymen. J Pediatric Gynecol 18: 427-429.
- Rabani SM (2013) A rare non urologic cause for urinary retention report of 2 cases. Nephro Urol Mon, p: 5.
- Nakajima E, Ishigouoka T, Yoshida T, Sato T, Miyamoto T, et al. (2015) Prenatal diagnosis of congenital imperforate hymen with hydrocolpos. Obstetric Case Reports. J Obstet Gynecol 35: 3.
- Miller RJ, Breech LL. (2008) Surgical correction of vaginal anomalies. Clin Obstet Gynecol 51: 223-236.
- Temizkan O, Kucur SK, Agar S, Gözükara I, Akyol A, et al. (2012) Virginity sparing surgery for imperforate hymen: Report of two cases and review of literature. J Turkish German Gynecol Assoc 13: 278-280.
- Karasahin E, Ercan CM, Alanbay I, Baser A (2011) Hymen-sparing surgery for imperforate hymen: Case reports and review of literature. J Pediatr Adolesc Gynecol 24: 54.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 10508
- [From(publication date):
June-2017 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 9622
- PDF downloads : 886