Research Article Open Access
Impaired Thinking in Patients with Breast Cancer and Depression
Jehn CF*, Flath B, Nogai H, Vuong L, Schmid P and Lüftner DDepartment of Hematology, Oncology and Tumorimmunology, Charité - Universitätsmedizin Berlin, Berlin, Germany
- *Corresponding Author:
- Christian Jehn
Department of Hematology
Oncology and Tumorimmunology
Charité - Universitätsmedizin Berlin, Berlin, Germany
Tel: +49-30-450-613259
Fax: +49-30-450-513919
E-mail: Christian.Jehn@charite.de
Received date: July 27, 2015; Accepted date: January 22, 2016; Published date: January 25, 2016
Citation: Jehn CF, Flath B, Nogai H, Vuong L, Schmid P, et al. (2016) Impaired Thinking in Patients with Breast Cancer and Depression. J Palliat Care Med 6:248. doi:10.4172/2165-7386.1000248
Copyright: © 2016 Jehn CF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Background: Brain-derived neurotrophic factor (BDNF) levels have been implicated in cognitive function and in the regulation of mood disorders, like depression. The aim of this study was to investigate the cognitive deficits of advanced cancer patients with depression and to assess the influence of various clinical factors on depression and cognition. Methods: Serum BDNF and plasma IL-6 were measured in patients treated for metastatic breast cancer diagnosed with depression according to DSM IV criteria. Cognitive function was assessed by the Piaget tasks and Verbal Learning and Memory Test, as a measure of short-term memory (STM) and long-term memory (LTM). Results: 29 patients with depression were compared to 27 matched controls without depression in this study. Even though both patient groups were of similar age, patients with clinical depression presented with a reduced Karnofsky performance status 66%. The presence of clinical depression was dependant on higher IL-6 levels (29.3 vs. 7.1 pg/ml; p=0.001) and cancer activity (p=0.002, χ2-test). BDNF had no direct association with depression. However, IL-6 level was an independent predictor of BDNF (b=-0.41, p=0.005). Patients with depression showed impairment of their ability to perform the Piaget tasks and a reduction in STM (4.0 vs. 6.8; p<0.001 and 18.9 vs. 32.3; p=0.003, respectively). Piaget tasks performance and STM were associated with lower BDNF levels (b=0.46, p=0.001 and b=0.23, p=0.043). Conclusions: Unlike IL-6, BDNF showed no association with depression in this population. Patients with low BDNF-levels and depression however, achieved lower scores in STM and Piaget tasks. The inability to perform the Piaget tasks adequately in this situation, demonstrates substantial difficulties in reasoning.
Keywords
Breast cancer; Piaget tasks; Depression; Impaired thinking; HADS; BDNF; IL-6; AVLT
Introduction
Brain-derived neurotropic factor (BDNF) has been shown to play a key role in neuronal plasticity, especially in brain regions pertinent to cognition and regulation of mood [1-3]. Depression is the most common mood disorder in the advanced cancer setting and often associated with an impaired cognitive function [4]. Depression and cognitive dysfunction increase functional impairment, compliance with therapy and reduce quality of life [5]. Like cancer, various diseases associated with significant inflammation show high prevalence rates of depression [6,7]. Thus, inflammatory cytokines, i.e. IL-6, have been implicated in the pathophysiology of depression [8,9].
It is a common observation that sick patients, although appearing to display normal mental capacity, might have difficulty thinking clearly when presented with complex clinical choices. Patients with advanced cancer are often forced to make important medical and financial decisions, for which they don’t seem fit at that point in time. In the presence of clinical depression these patients can face cognitive deficits that make sound reasoning difficult.
Multiple studies have described a decline in cognitive function of the following cognitive domains: learning and memory, processing speed and executive function [10]. Most studies measured the cognitive function in post-chemotherapy healthy breast cancer survivors and patients receiving adjuvant chemotherapy [11-14]. A variety of neuropsychological assessment tools has been used. To increase the homogeneity of studies the International Cognition and Cancer Task Force (ICCTF) has recommended 3 tests, which measure learning and memory, processing speed and executive function: The Hopkins Verbal Learning Test (HVLT-R), the Trail Making Test (TMT) and the Controlled Word Association (COWA) of the Aphasia Examination [15]. To explore the memory function capabilities of our patients we applied the Verbal Learning and Memory Test (VLMT). Since the proposed test for measuring the executive function capabilities overwhelmed most of our advanced cancer patients, specifically in terms of their limited attention span we chose to apply the Piagetian tasks in an unusual manner in this situation.
The Piagetian tasks were developed to measure the cognitive development of children [16]. They evaluate the mental abilities necessary to take transitions of information into account and process them correctly. For example, when fluid is poured from one container into another container of different shape, the change in water level is not indicative of change in quantity, a transition an adult brain can perform.
This also applies to the logical reversibility of such a transition, such as the remodeling of a ball of clay into a sausage and back into the original shape of a ball, does not include the loss of substance or mass. Children learn to master these transitional tasks at the age of 6-10 years [17]. According to the classical models of cognitive development, early stages before age 6 are characterized by such a cognitive and perceptual bias, leading to this incorrect performance. This bias should to be overcome when higher executive networks in the anterior cingulate cortex and the prefrontal cortex develop at the age of 6-10 [18-20].
We conducted this cross-sectional study to examine cognitive dysfunction in breast cancer patients with depression, by employing a validated cognition test for short-term (STM) and long-term memory (LTM) and applying the Piaget tasks in an unusual way. In addition, we investigated the influence of various factors like BDNF, IL-6 and demographic factors on depression and cognition in this metastatic setting.
Patients and Methods
Patients with advanced metastatic breast cancer were evaluated at bedside for symptoms of depression. All patients were receiving their current course of chemotherapy at time of evaluation. The same investigator collected the blood samples and performed the cognition tests like the MMSE, VLMT and the Piaget tasks. In addition, demographic data like age, Karnofsky Performance Status (KPS), hormone receptor status, location and number of metastasis, prior adjuvant treatments, prior number of chemotherapy line was collected.
This study was approved by the institutional ethics committee, all patients gave their informed consent.
All subjects presented themselves with a Mini-Mental state Examination (MMSE) score of at least 24 [21]. Exclusion criteria were: radiation therapy within the last 3 months, untreated endocrine diseases, renal insufficiency requiring dialysis or any form of neurological malfunction, i.e. meningeosis carcinomatosa, brain metastasis or known diagnosis of affective disorders (even if treated). None of the patients were receiving medication for treatment of affective disorders, anticonvulsants or long-term steroid use (>8 weeks).
All participants completed the Hospital Depression Scale (HADSD) and underwent cognition testing (VLMT, Piaget tasks) on the same day as the blood draw, before receiving chemotherapy. The HADS was specifically developed for the assessment of depressive symptoms in patients with somatic disease [22-24]. All patients with a probable caseness of clinical depression (HADS-D scores ≥11) were further examined with a structured clinical interview (SCID) according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) [25].
Blood samples for the measurement of IL-6 and BDNF concentrations were collected at 09:00 AM, before administration of chemotherapy [26]. Plasma IL-6 and serum BDNF levels were measured with commercially available ELISA kits [Immulite/Immulite 1000 IL-6, DPC Biermann Germany; Quantikine Human BDNF, R&D Systems, Minneapolis, MN, USA] according to the manufacturer’s instructions. Each essay was performed in duplicate. All samples were assayed by personnel, who were blind to the identity of the study subjects.
Learning and memory
The Verbal Learning and Memory Test (VLMT) is an advanced version of the Rey Auditory-Verbal Learning Test (AVLT) and a validated measure of verbal learning and memory in German language [27-29]. The following two scores were used: total learning ΣDg1-5 (consisting of a 15-item word list (List A) practiced over 5 learning trials) and the delayed recall ΣDg5-7 (the number of correct responses from delayed recall of List A, after an intrusion List B).
The total learning process (ΣDg1-5) is a function of short-term memory (STM) and represented by the acquisition and encoding of information, whereas the delayed recall score (ΣDg5-7) reflects the retrieval of items from memory, as a function of long-term memory (LTM) [30,31].
Piaget tasks
The following 7 Piaget tasks were administered in the same order to each patient:
Conservation of number: The patient is presented with two parallel laid rows of marbles, each consisting of 4 marbles. Then the 4 marbles in the one row are spread apart to double the length of the row. The patient is asked if the two rows of marbles still have the same amount of marbles.
Conservation of length: The patient was asked to pick two sticks of equal length among a choice of three. The two equal sticks were placed side by side and the patient was asked if the two stick were sill equal in length. This procedure was repeated with the stick displaced both up and to the left.
Conservation of volume: The patient is shown 2 identical containers (such as urine collection cups) that contained an equal amount of water. The patient was first asked to confirm their equivalence, than the content of one container was poured into a different tall and narrow container (i.e. test tube). Now the patient was asked if the two liquid filled containers had an equal amount of water.
Conservation of substance: The patient was presented with two equal balls of clay and asked to confirm the equal amount of clay between the balls. One ball then was formed into a long sausage thin rode. The patient was then asked if the two pieces of clay still were of equal amount.
Conservation of area: Two same size pieces of paper (20 cm × 10 cm) were shown to the patient. One of the pieces of paper was cut into 5 stripes and laid end to end. The patient was then asked if the strips were equal in area to the uncut paper.
Preservation of the horizon: An upright water glass picture, with the water level drawn parallel to the bottom of the glass was shown to the patient. Then a picture of the same water glass in a 45% tilted position was shown and the patient was asked to draw in the water line.
Ability to classify: The patient is shown pictures of animals, featuring ducks, non-duck birds, or non-bird other animals. The patient is first asked to sort the pictures into 3 groups: A=ducks, B=birds (non-duck birds), C=other animals (non-bird animals), then to put each picture into the accordingly labeled envelope (A: ducks, B: birds, or C: animals). Patients where then asked if envelope A could retain its label if envelope B was placed inside it. The same was done with B and C.
Statistical Methods
Descriptive analysis included absolute and relative frequencies for categorical variables, as well as mean, standard deviation, median and range for numerical measurements. For univariate group comparisons between categorical variables and patients groups (depression vs. no depression), the Chi square test, for small sample sizes, the Fisher’s Exact test were applied, as appropriate.
The Wilcoxon-Test for independent samples was used to assess the degree of variance of continuous variables between the two patient groups (depression vs. no depression). Correlations were evaluated using the Spearman’s correlation coefficient. All results were considered significant at p<0.05 (two-tailed).
A multiple logistic regression analysis was performed to identify independent predictors (IL-6, BDNF, age, KPS, Tumor activity) for depression. In addition, linear regression was applied to determine the independent influence of various variables on BDNF and the ability to perform the Piaget tasks. The resulting models were obtained after forward and backward selection. For comparability, standardized regression coefficients are presented as well.
Results
Twenty-nine patients were diagnosed with clinical depression and 27 matched cancer patients with no history of depression were recruited for comparison. All 29 patients identified in the HADS probable caseness of clinical depression satisfied the diagnostic criteria for depression according to DSM IV. The 56 female participants evaluated, had a mean age of 60 years and presented themselves with a reduced KPS of 66%. 95% of the women had visceral metastasis, with metastasis of the liver being in 75% most frequent. All patients were being treated with chemotherapy starting either on a new regime due to progression (64%) or continuing with the next cycle if patients were classified as stable disease (36%) (Table 1).
| Variable | All Patients (n=56) |
|---|---|
| Mean age (SD) | 60 years (±12.1) |
| Karnofsky Performance Status (SD) | 66% (±10.2) |
| Previous adjuvant treatment n (% of patients) | |
| Chemotherapy | 39 (69%) |
| Endocrine therapy | 17 (231%) |
| Number of metastatic sites | |
| 1 | 5 (6%) |
| 2 | 20 (39.3%) |
| >3 | 31 (54.7%) |
| Metastatic sites n (% of patients) | |
| Visceral metastases | 53 (95%) |
| Lung | 21(39.1%) |
| Liver | 42 (75%) |
| Bone | 38 (67.9%) |
| Hormone receptor status (%) | |
| Positive | 35 (62%) |
| Negative | 21 (38%) |
Table 1: Characteristics of patients with metastatic breast cancer.
Table 2 shows a comparison of the characteristics of patients with and without depression. Patients with depression showed a lower performance status (63% vs. 70.4%; p=0.03). In addition, depression was associated with higher levels of inflammation, expressed by elevated plasma IL-6 concentration (29.3 vs. 7.1 pg/ml; p=0.001). Symptoms of depression were strongly correlated with levels of IL-6 and reciprocal with KPS (r2=0.56, p<0.001 and r2=-0.35, p=0.011, respectively). The presence of depression was also dependent on cancer activity (i.e. progressive disease (Chi-square: 8.5; degrees of freedom (df): 1; p=0.002). Depression was not influenced by age, hormone receptor status (p=0.48, χ2-test) or prior number of chemotherapy lines (p=0.13, χ2-test). (Depression vs. no Depression). Variables are presented as mean values and standard deviations. For univariate group comparison, the X2-test and the t test or, in case the normal distribution assumption being violated, the Mann-Whitney’s test was performed.
| Characteristic | Depression(n=29) | No Depression (n=27) | P value |
|---|---|---|---|
| HADS-D-Score (0-21) | 13.7 ± 2.7 | 4.5 ± 2.2 | p<0.001 |
| Age (years) | 61 ± 10.9 | 59 ± 9.5 | p=0.52 |
| p=0.03 | |||
| KPS1 (%) | 63 ± 10.7 | 70.4 ± 12.7 | |
| Number of prior chemotherapy lines% | |||
| 1 | 11 | 13 | |
| 2 | 57 | 46 | |
| 3 | 20 | 25 | p=0.71 |
| 4 | 12 | 16 | |
| Hormone receptor status | |||
| Positive | 19 | 16 | p=0.49 |
| Negative | 10 | 11 | |
| Tumor-status | |||
| SD2 | 8 | 12 | p=0.002 |
| PD3 | 21 | 15 | |
| IL-6 (pg/ml) | 29.3 ± 30.1 | 7.1 ±10.8 | p=0.001 |
| BDNF (pg/ml) | 25.1 ± 24.1 | 33.1 ± 24.2 | p=0.26 |
| Cognition | |||
| STM4: Dg1-5 | 18.9 ± 6.9 | 32.3 ± 10.5 | p=0.003 |
| LTM5: Dg5-7 | 4.2 ± 2.0 | 3.1 ± 1.8 | p=0.1 |
| Piaget Score (1-7) | 4.0 ± 1.2 | 6.8 ± 0.8 | p<0.001 |
1Karnofsky Performance Status; 2Stable Disease; 3Progressive Disease;4Short-term memory; 5Long-term memory
Table 2: Comparison of demographics between both patients groups (depression vs. no depression).
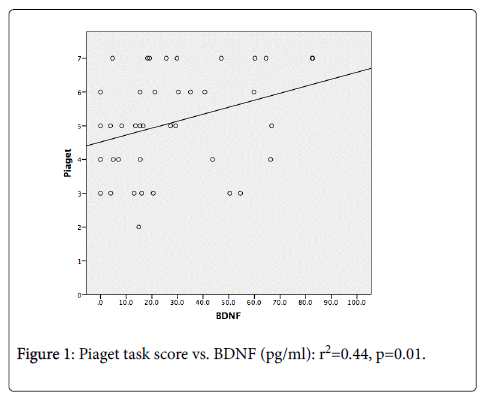
After multiple logistic regression analysis with depression as the dependent variable and age, KPS, Tumor activity IL-6 and BDNF as the independent variables, only IL-6 was an independent predictor for depression (odds ratio (OR)=1.5; 95%CI, 1.0-1.9 (p=0.02). BDNF showed no association with clinical depression or depressive symptoms (p=0.26). BDNF, on the other hand, showed a strong correlation with IL-6 (r2=0.52, p<0.001). In linear regression analysis, only IL-6 was independently associated with BDNF negatively (b=-0.41, p=0.005). BDNF also was positively correlated with parameters of cognition (short-term memory: r2=0.50, p=0.02; Piaget-Score: r2=0.44, p=0.01) (Figure 1).
Patients with clinical depression showed significant impairment of their ability to perform the Piaget tasks (4 vs. 6.8; p<0.001). In addition, short-term memory was also reduced in depression (VLMT Dg1-5) (18.9 vs. 32.3; p=0.003). The ability to perform the Piaget tasks was directly correlated with the level of depression (r2=-0.65, p<0.001) (Figure 2), IL-6 (r2=-0.59, p<0.001), BDNF (r2=0.44, p=0.01) and short-term memory (r2=0.77, p<0.001).
Linear regression analysis showed that performance of the Piaget tasks was predicted in-dependently only by BDNF level and short-term memory (b=0.23, p=0.043 and b=0.46, p=0.001, respectively). The prior number of chemotherapy lines (b=-1.1; p=0.42), KPS (b=1.4; p=0.51) or age (b=-1.8; p=0.12), had no influence on the ability to perform the Piaget tasks. Only LTM was reduced by a poor KPS (b=-0.31; p=0.03).
Discussion
The aim of this study was to investigate the cognitive deficits of advanced cancer patients with depression and to highlight the influence of various clinical factors associated with such an advanced stage on depression and cognition in a hospital setting.
29 patients were diagnosed with clinical depression while receiving chemotherapy at an oncology unit. Unsurprisingly patients with depression showed a lower performance status, compared to patients without depression, however in a similar cancer setting. Patients with depression expressed higher levels of IL-6, indicating more inflammation. This finding is further supported, by the strong association of depression with cancer activity, i.e. progressive disease. Cancer progression is characterized by a marked increase in inflammatory markers, like IL-6 [32,33]. The influence of IL-6 on depression has been shown extensively in somatic healthy patients and patients with metastatic cancer [34,35].
In search of further depression markers, we examined the role of BDNF, a driving force of neuroplasticity and neurogenesis in the hippocampus. The hippocampus is a crucial brain structure implicated in cognitive function and in the regulation of mood disorders, like depression [36,37].
BDNF however, showed no association with depression in patients with advanced metastatic cancer. Studies evaluating somatic healthy patients suggest BDNF to play a pivotal role in neuroplasticity and depression [38]. However, there seem many unknown confounding factors surrounding the evaluation of BDNF, which have also resulted in negative trials. Besides factors such as age, sex, the optimal method for assessment of BDNF in the blood (serum vs. plasma) and the actual potential of BDNF to cross blood-brain barrier, the release of BDNF stored in platelets is serious confounding factor in this assessment we didn’t account for in this cancer patient population [39,40].
Of the three parameters of cognition (STM, LTM and Piaget tasks), only STM and Piaget tasks were impaired when associated with depression.
BDNF implicated to be a driving force of neuroplasticity and neurogenesis in the hippocampus was interestingly independently negatively influenced by IL-6. This finding supports the hypothesis that inflammation reduces neuroplasticity by down-regulation of BDNF as the underlying pathophysiology of depression [3]. BDNF emerged as strong positive determinant of short-term memory and Piaget tasks.
Very few studies have investigated the cognitive deficits in advanced cancer patients receiving chemotherapy and being burdened by depression. The ICCTF neuropsychological test recommendations were made in the context of data pertaining to healthy postchemotherapy breast cancer survivors and in the adjuvant setting. We would therefore argue that the validity of this formal neuropsychological test in the advanced cancer setting can be challenged. Especially measuring the domain executive function requires a reasonable attention span, not always given in this advanced cancer situation. We decided therefore to apply the Piaget tasks, as a descriptive measure of visual-spatial judgment and reasoning, as functions of executive function. The Piaget tasks can be performed easily at the bedside, are short in duration (10 min) and proved to be feasible in the context of a reduced attention span. The relevance of the Piaget tasks as a measure of cognitive ability has not been validated in adults with cancer either. Its results can therefore only be thought as hypothesis generating, and were not meant to substitute for comprehensive neuropsychological assessment.
A current discussion in developmental psychology exists, whether such cognitive and perceptual biases of early childhood still remain as relicts in adults [41,42]. To succeed at the Piaget task, children have to inhibit a misleading strategy, the visual-spatial bias, by activating a higher executive network of the anterior and frontal cortex [43,44]. In our study, performance in the Piaget test was positively associated with the level of BDNF and negatively by the presence of depression. This leaves room for speculation, that the higher executive network in the anterior and frontal cortex, which is necessary to overcome the cognitive and perceptual bias, is possibly inhibited in the state of depression. BDNF on the other hand could strengthen this mechanism.
Due to the cross-sectional study design and possible confounding factors unaccounted for, like the BMI, education level, smoking and influence of the pain medication (i.e. Opiates), the results can only be seen as hypothesis generating.
However, some interesting observations could be made. All patients past the MMSE and did not suggest impaired cognition. The findings of especially the Piaget task test however, seem troubling, since these same patients are forced to make serious decisions that require reasoned consideration. Even though the patients exhibited reasoning abilities similar to those of children between the ages of 6-10 years, they should by no means be seen as childish. They are confronted with a flood of information concerning treatment implications, giving informed consistent to treatment, study participation and possibly other financial issues. Not always are decisions made in the best interest on behalf of the patient. A prior knowledge of this state of reasoning could facilitate faster support.
References
- Castren E, Rantamaki T (2010) The role of BDNF and its receptors in depression and antidepressant drug action: Reactivation of developmental plasticity. DevNeurobiol 70: 289-297.
- Deng W, Aimone JB, Gage FH (2010) New neurons and new memories: how does adult hippocampal neurogenesis affect learning and memory? Nat Rev Neurosis 11:339-350.
- Eisch A, Petrik D (2012) Depression and hippocampal neurogenesis: a road to remission? Science 338:72-75.
- Massie MJ (2004) Prevalence of depression in patientswith cancer. J Natl CancerInstMonogr 32:57-71.
- McIntyre RS, Cha DS, Socynska JK, Woldeyohannes HO, Gallaugher LA, et al. (2013) Cognitive deficits and functional outcomes in major depressive disorder: determinants, substrates, and treatmant interventions. Depress Anxiety 30:515-527.
- Katon W, Sullivan MD (1990) Depression and chronic medical illness. J Clin Psychiatry51 Suppl:3-11.
- Iwata M, Ota Kt, Duman RS (2013) The inflammasome: pathways linking psychological stress, depression, and systemic illness. Brain BehavImmun31:105-114.
- Sluzewska A, Rybakowski J, Bosmans E, Sobieska M, Berghmans R, et al. (1996) Indicators of immune activation in major depression. Psychiatry Res 64:161-167.
- Valkanova V, Ebmeier KP, Allan CL (2013) CRP, IL-6 and depression: a systematic review and meta-analysis of longitudinal studies. J Affect Disord 150:736-744.
- Jansen CE, MiaskowskiC, Dodd M, Dowling G, Kramer J (2005) A metaanalysis of studies of the effects of cancer chemotherapy on various domains of cognitive function. Cancer 104: 2222-2233.
- Hermelink K, Untch M, Lux MP (2007) Cognitive function during neoadjuvant chemotherapy for breast cancer: results of a prospective, multicenter, longitudinal study. Cancer 109: 1905-1913.
- Falleti MG, SanfilippoA, Maruff P, Weih L, Philips KA (2005) The nature and severity of cognitive impairment associated with adjuvant chemotherapy in women with breast cancer: a meta-analysis of the current literature. Brain Cogn 59:60-70.
- Ahles TA, Root JC, Ryan El (2012) Cancer-and cancer treatment associated cognitivechange: an update on the state of the science. J Clin Oncol 30:3675-3686.
- Cruzado JA, Lopez-Santiago S, Martinez-Marin V, Jose-Moreno G, Custodio AB, et al. (2014) Longitudinal study of cognitive dysfunctions induced be adjuvant chemotherapy in colon cancer patients. Support Care Cancer 22:1815-1823.
- Werfel IS, Vardy J, Ahles T, Schagen SB (2011) International cognition and cancertask force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncol 12:703-708.
- Piaget J (1950) The Psychology of Intellegence. New York: International Univ Press.
- Piaget J (1984) Piaget’s theory. In P Mussen (Ed.), Handbook of child psychology New York: Wiley 103-128.
- Epley N, Morewedge CK, Keysar B (2004) Perspective taking in children and adults: equivalent egocentrism but differential correction. Journal of Experimental Social Psychology 40: 760-768.
- Casey BJ, Trainor R, Orendi JL (1997b) A developmental functional MRI study of prefrontal activation during performance of a Go-NO-Go task. Journal of Cognitive Neuroscience 9: 835-847.
- Durston S, Thomas KM, Yang Y, Ulug AM, Zimmerman RD, et al. (2002) A neural basis for the development of inhibitory control. Developmental Science 5: 9-16
- Folstein MF, Folstein SE, McHugh PR (1975) Mini-Mental State (a practical method for grading the state of patients fort he clinician). Journal of Psychiatric Research 12: 189-198.
- Zigmond AS, Snaith RP (1983) The Hospital anxiety and depression scale. ActaPsychiatrScand 67:361-370.
- Herrman C (1997) International experiences with the hospital anxiety and depression scale- a review of validation data and clinical results. J Psychosom Res 42: 17-41.
- Morrey S, Greer S, Watson M (1991) The factor structure and factor stability of the hospital anxiety and depression scale in patients with cancer. Br J Psychiatr 158:255-259.
- American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders. American Psychiatric Association, Washington.
- Fowers L, Humphries SE, Mohamed-Ali V (2000) Effects of sample handling on the stability of interleukin-6, tumor necrosis factor-a and leptin. Cytokine12:1712-1716.
- Helmstaedter C, Durwen HF (1990) VLMT (VerbalerLern-und Merkfähig-keitstest). Einpraktikables und differenziertesInstrumentariumzurPrüfung der verbalenGedächnisleistungen. SchweizerArchivfür Psychiatry 141: 21-30.
- Crawford JR, Steward LE and Moor JW (1989) Demonstration of savings on the AVLT and development of a parallel form. Journal of Clinical and Experimental Neuropsychology 11: 975-981.
- Mueller H, Hasse Sander I, Horn R, Helmstaedter C, Elger CE (1997) Rey- Auditory-VerbalLearning Test: Structure of a modifiedGerman version. Journal of Clinical Psychology 53: 663-671.
- Helmstaedter C, Grunwald T, Lehnertz K, Gleissner U, Elger CE (1997). Differential involvement of left temporolateral and temporomesial structures in verbal declarative learning and memory: evidence from temporal lobe epilepsy. Brain and Cognition 35: 110-131.
- Vakil E, Blachstein H (1993) A Rey Auditory-Verbal Learning Test: structure analysis. Journal of Clinical Psycholog49: 883-890.
- Pierce BL, Ballard-Barbash R, Bernstein L, Baumgartner RN, Neuhouser ML, et al. (2009) Elevated biomarkers of inflammation are associated with reduced survival among breast cancer patients. J Clin Oncol 27: 3437-3444.
- Zhang GJ, Adachi I (1999) Serum interleukin-6 levels correlate to tumor progression and prognosis in metastatic breast carcinoma. Anticancer Res 19: 1427-1432.
- Dentino AN, Pieper CF, Rao MK, Currie MS, Harris T, et al. (1999) Association of interleukin-6 and other biologic variables with depression in older people living in the community. J Am GeriatrSoc 47:6-11.
- Lutgendorf SK, Weinrib AZ, Penedo F, Russell D (2008). Interleukin-6, cortisol, and depressive symptoms in ovarian cancer patients. J Clin Oncol 26:4820-4827.
- Duman R, Monteggia LM (2006) A neurotrophic model for stress-related mood disorders. Biol Psychiatry 59:1116-1127.
- Deng W, Aimone JB, Gage FH (2010) New neurons and new memories: how does adult hippocampal neurogenesis affect learning and memory? Nat Rev Neurosci11:339-350.
- Krishnan V, Nestler EJ (2008) The molecular neurobiology of depression. Nature 455:894-902.
- Pan W, Banks WA, Fasold MB, Bluth J, Kastin AJ (1998) Transport of brain-derived neurotrophic factor across the blood-brain barrier. Neuroparmacology37:1553-1561.
- Karege F, Bondolfi G, Gervasoni N, Schwald M, Aubry JM, et al. (2005) Low brain-derived neurotrophic factor (BDNF) levels in serum of depressed patients probably results from lowered platelet BDNF release unrelated to platelet reactivity. Biological Psychiatry 57: 1068-1072.
- Durston S, Davidson MC, Tottenham N, Galvan A, Spicer J, et al. (2006) A shift from diffuse to focal cortical activity with development. Developmental Science 9: 1-9.
- Bekker EM, Kenemans JL, Verbaten MN (2005) Source analysis of the N2 in a cued go/nogo Task. Brain Res CognBrain Res 22:221-231.
- Leroux G, Spiess J, Zago L (2009) Adult brains don’t fully overcomebiases that lead to incorrect performance during cognitive development: an fMRI study in young adults completing a Piaget task. Developmental Science 12: 326 -338.
- Diamond A, Kirkham N (2005) Not quite as grown-up as we like to think: parallels between cognition in childhood and adulthood. Psychological Science 16: 291-297.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 10484
- [From(publication date):
January-2016 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 9648
- PDF downloads : 836