Research Article Open Access
Impact of Total Mesorectal Excision on Bladder and Sexual Function in Rectal Cancer
Mohammad Sultan Dar, Fazl Qadir Parray*, Arif Hamid Bhat, Nisar Ahmed Chowdri and Mohd Lateef WaniColorectal Division, Department of General and Minimal Invasive Surgery and Urology, Sher-i-Kashmir Institute of Medical Sciences, Soura, Srinagar, J&K, India
- *Corresponding Author:
- Fazl Qadir Parray
Colorectal Division
Department of General and Minimal Invasive Surgery and Urology
Sher-i-Kashmir Institute of Medical Sciences
Soura, Srinagar-190011, J&K, India
Tel: +919419008550
E-mail: fazlparray@rediffmail.com; fazlparray@gmail.com
Received Date: November 30, 2016; Accepted Date: December 12, 2016; Published Date: December 19, 2016
Citation: Dar MS, Parray FQ, Bhat AH, Chowdri NA, Wani ML (2016) Impact of Total Mesorectal Excision on Bladder and Sexual Function in Rectal Cancer. Cancer Surg 2: 110.
Copyright: © 2016 Dar MS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Cancer Surgery
Abstract
Background: In this prospective study we evaluated bladder, sexual function and frequency of identification of pelvic autonomic nerve preservation (PANP) after open total mesorectal excision in males with operable carcinoma rectum below 12 cm.
Patients and Methods: prospective study of 47 male patients of carcinoma rectum 4-12 centimetres from anal verge. The preoperative status was used for comparison with the post-operative and follow up status of same patient. Sexual function was assessed by international index of erectile function questionnaires (IIEF) and bladder function was assessed by uroflowmetry, transcutaneous ultrasound and international prostate symptom score (IPSS).
Results: IIEF score decreased at 1month post operation with significant change in p-value and at 3 month with an insignificant change in P-value. After 3 months sexual dysfunction was reported in 30% patients. Erectile function was also significantly decreased at 1 month and at 3 months it was seen in 37% of patients. Change in IPSS was significant at 1month and resultant bladder function was present in 90% of patients and at 3 months present in 28% of patients. Resultant bladder dysfunction with USG was 82% and 30% after 1 and 3 months of surgery respectively. With urodynamics resultant bladder dysfunction was present in 77% and 29% of patients respectively after 1 and 3 months of surgery. Pelvic autonomic nerves were identified in 96% patients and complete preservation of nerves was achieved in 89% patients and partial preservation was achieved 6% and in 4% pelvic autonomic nerves could not be identified.
Conclusion: Bladder and sexual dysfunction can be decreased after an meticulous nerve sparing total mesorectal excision. IIEF and IPSS are all well suited to evaluate bladder and sexual dysfunction after rectal surgery.
Keywords
Bladder; Sexual function; Total mesorectal excision
Introduction
Cancer burden continues to be one of the most important challenges in our country India. As per the estimates India has 2-2.5 million cases of cancer at any given point of time. The estimates show that 7-9 lakh new cases are detected each year and 50% of them die each year [1]. In 2026 the cancer burden is expected to double in number [2]. However, the greener part of it is that advanced investigative tools and modern treatments have increased the 5 year survival of most of the cancers [3].
Cancer is a universal disease but shows geographical, ethnical and environmental variations from place to place. It is recognized as the second killer disease in humans [4].
Our valley of Kashmir is situated in north of India, landlocked geographically by mighty Himalayas with cold weather like most of the European countries. The inhabitants of this region are more fond of non-vegetarian diet especially red meat and salt tea which makes them more prone to gastrointestinal cancers as compared to rest of the population in the country. The valley of Kashmir has a population of approximately 10 million and has a single tertiary care medical institute named Sher-I-Kashmir Institute of Medical Sciences (SKIMS). There is no any independent cancer hospital in J&K and regional cancer centre (RCC) SKIMS is the only centre in Kashmir which is an integral part of this tertiary care institute. RCC (SKIMS) was established under national cancer control program with the objective to provide cancer treatment facilities in addition to prevention activities across the state [5].
A hospital cancer registry (HCR) under national cancer 137 registry program is well maintained by the department of medical records which provides statistical and surveillance support to researchers.
The leading sites of cancer in Kashmir during the study period were esophagus and gastroesophageal (GE) junction (19.95%), lung (16.54%), stomach (11.60%), colorectal (7.36%), lymphomas (5.40%), skin (3.46%), laryngopharynx (3.0%), acute leukemias (2.62%), prostate (1.7%) and brain (1.54%).
Females
The leading sites among females were breast (16.83%), oesophagus and GE junction (12.85%), ovary (7.45%), colorectal (6.68%), stomach (6.60%), lungs (4.56%), gall bladder (3.9%) lymphomas (3.30%), acute leukemias (2.45%) and brain (1.95%) [6].
In a separate prospective study on colorectal cancer spread over a period of one year, it was found that the truncated age adjusted incidence rates in age group 35-64 years was 8.31/100,000; while that for colorectal carcinoma was 8.77/100,000 in males and 7.66/100,000 in females. This is a hospital based incidence and doesn’t depict the community based incidence [7].
Since, we are working in the colorectal division of this tertiary care institute; it exposes us (3 full time consultants) to a large volume of colorectal cancer operative exposure. The volume is showing steadily an upward trend and at present it is in the range of 225-250 cases/year. Since, our department is performing a good quality Total mesorectal excision for rectal cancer so it was thought worthwhile to focus further on nerve preservation by indirectly auditing the bladder function, sexual function and trying to identify and preserve autonomic nerves in each and every case.
The techniques for excision of rectum used in 1970’s of extended rectal dissection were associated with severe urinary and sexual dysfunction. With the introduction of neoadjuvant treatment, total mesorectal excision with preservation of pelvic autonomic nerves, functional outcome and survival markedly improved [8].
It was Bill Heald who popularized the concept of “Zone of downward spread” and gave the concept of total mesorectal resection in 1982, which includes mesorectum in resection specimen; indeed a complex operation because of difficult pelvic anatomy. Total mesorectal excision (TME) has resulted in good functional outcomes with better survival rate of 50-70%, a decrease in total recurrence rate from 50-30% and a decrease in incontinence and bladder dysfunction from 85-15%. The concept of TME was further popularized by Enker [9,10].
Sir William Ernest Miles in 1908 performed first Abdominoperineal Resection (APR) and in 1950 Anterior Resection (AR) replaced APR. But both were associated with high incidence of post-operative bladder and sexual dysfunction [11]. TME with pelvic autonomic nerve preservation has been reported to be an ideal surgery for rectal carcinoma, as it minimizes local recurrence, sexual and bladder dysfunction. These changes evolved to include deliberate autonomic nerve preservation that was ultimately labelled as pelvic autonomic nerve preservation (PANP) [12-14].
TME with Pelvic Autonomic Nerve Preservation (TME-PANP) is now a gold standard treatment for lower and middle third of carcinoma rectum [15-17]. The high quality of TME should fulfil two clinical measurements: absence of impotence or incontinence and at least single digit i.e., less than 10%, 5-year cumulative recurrence rate regardless of adjuvant therapy [18].
Complications like voiding dysfunction grossly decreased after TME-PANP, but the significant number of sexual dysfunctions persisted despite TME-PANP. These complications should be discussed with patient and his attendants in detail before surgery to avoid any unwanted litigations [19].
Material and Methods
This prospective study was conducted in the Colorectal division of Department of General Surgery and Urology at Sher-I-Kashmir Institute of Medical Sciences; Srinagar, India. This study included all male patients of cancer rectum below 12 centimeters. Patients were subjected to low anterior resection or ultralow resection ± J-pouch or Coloplasty reconstruction with total or partial mesorectal excision as per the indication, type, and distance from anal verge and type of the growth and pelvic anatomy. In patients with stage C and stage B (bad) neoadjuvant was given to downstage the disease. All patients were preoperatively optimized for surgery and baseline and specific investigations like CEA were done. Patients in whom a sphincter saving procedure plan couldn’t be executed were excluded from the study and in whom protective loop ileostomy was added were also excluded from the study. In patients of study group the workup was done as per a standard proforma described as under:
1. Detailed history and presenting complaints with emphasis on a) Bleeding per rectum, b) Bowel habits and Stool character.
2. General physical examination with emphasis on lymphadenopathy, anemia, edema, ascites or organomegaly and Local Examination-Digital Rectal Examination (DRE), proctoscopic examination (PE), Sigmoidoscopy or Colonoscopy.
3. Preoperative staging of carcinoma by TNM, Multi slice CT scan/ Transrectal ultrasound or Endocoil or surface MRI was also done.
4. Preoperative bladder function was assessed by spontaneous flowmetry, residual volume of urine measurement and urodynamics examination including urinary flow recording, “International Prostrate Symptom Score” and transcutaneous ultrsonographic method after admission in ward and after 1 and 3 months after curative rectal excision (sphincter preserving) and was statistically analyzed.
5. Preoperative sexual function was assessed by “International Index of Erectile function” (IIEF) questionnaires after admission and 1 and 3 months after curative excision, with special emphasis on erectile function.
6. Frequency of bladder and sexual dysfunction was compared in pre-operative and follow-up period and statistically analysed (each patient acting as a control for him).
7. Details of intra-operative findings like TNM staging, status of liver, ascites, blummer’s shelf, any synchronous lesion was noted in case records and details about autonomic nerve identification was entered in case records in order to the assess the frequency of identification and subsequent preservation of these nerves.
8. Statistical methods employed in our study were one way measure of variance We used Kruskall-Wallis test and Friedmans test to calculate mean, standard deviation and normality test KS (Kolmogrov and Smirnov). The software used was Annova. Based on above tests pvalue was calculated and it was compared to normality test i.e., passed normality yes or not.
Observations
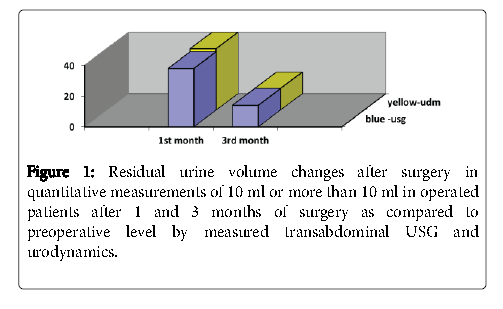
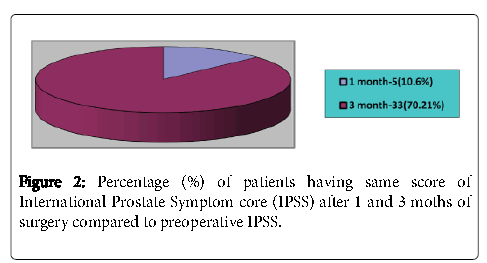
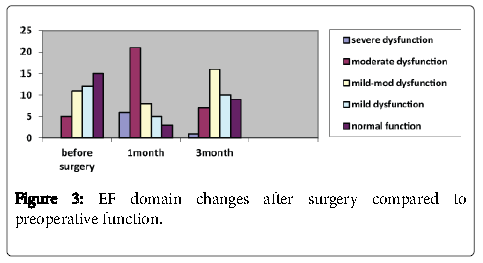
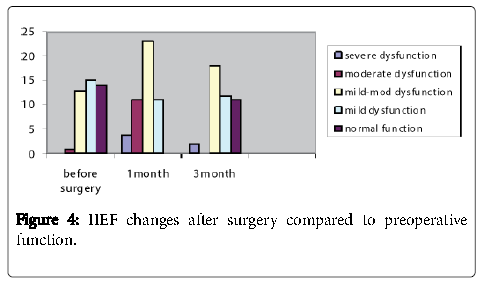
In our study total 47 patients were included, all were male and study period ranged from May 2010 to August 2012. Age distribution was from 20-76 years with mean of 50 years (Tables 1-7) (Figures 1-4).
| Number | Percentage | ||
|---|---|---|---|
| Presenting complaints | Bleeding per rectum-40 | 85.10% | |
| Altered bowel habits- 7 | 14.90% | ||
| Past history | Smoking | 9 | 19.10% |
| Hypertension | 10 | 1.20% | |
| Hypothyroidism | 3 | 6.30% | |
| Type 2 Diabetes Mellitus | 4 | 8.51% | |
| Cardiovascular disease | 2 | 4.20% | |
| Distance of tumor from anal verge | Low rectal-2 | 4.20% | |
| Mid rectal- 35 | 78.70% | ||
| Upper rectal-10 | 21.20% | ||
| Neoadjuvant treatment | 15 | 31.80% | |
| Surgical procedure | Low anterior resection -40 | 85% | |
| anterior resection-2 | 4% | ||
| LAR with Coloplasty-5 | 10.60% | ||
| PANP preservation | Complete-42 | 89.36% | |
| Partial-3 | 6.30% | ||
| Not known-2 | 4.20% | ||
| TNM Staging | Stage I-(7) | 25.50% | |
| Stage II-(14) | 29.78% | ||
| Staging IIIA-4,III-B8, III-C11(23) | 48.93% | ||
| Stage IV-(3) | 6.30% | ||
| Status of TME | Complete-42 | 89.36% | |
| Partial-5 | 10.63% | ||
Table 1: Demographic, clinical characteristics, past history and surgical details of patient undergoing surgery.
| Residual urine | Timing | Range | Mean | Normality test KS | P-value | Passed normality test |
| Before surgery | 0-240 | 54.34 | 0.1569 | 0.0054 | No | |
| After 1month | 0-280 | 82.29 | 0.1566 | 0.0055 | No | |
| After 3months | 0-260 | 66.85 | 0.1449 | 0.0151 | No | |
| IPSS | Before surgery | 0-12 | 3.8 | 0.0171 | 0.01417 | No |
| After 1month | 0-18 | 6.2 | 0.0522 | 0.1266 | Yes | |
| After 3 months | 0-14 | 4.8 | 0.0028 | 0.1646 | No |
IPSS ranges from 0-35, mild dysfunction 0-7, moderate dysfunction 8-19 and severe dysfunction 20-35
Table 2: Residual urine volume and IPSS changes before and after 1 and 3 months of surgery measured by utltrasonographic method.
| Variables | Timings | Range | Mean | Normality test KS | p-value | Passed normality test` |
|---|---|---|---|---|---|---|
| Peak flow rate ml/s | Before surgery | 12-24ml/s | 17.31 | 0.1661 | 0.0023 | No |
| 1 month | 6-22ml/s | 13.78 | 0.1089 | 0.001 | Yes | |
| 3 months | 9-23ml/s | 15.744 | 0.1341 | 0.0038 | No | |
| Residual urine | Before surgery | 0-216ml | 60.17 | 0.1496 | 0.0101 | No |
| 1 month | 0-290ml | 86.38 | 0.1275 | 0.1275 | Yes | |
| 3 months | 0-230ml | 72.27 | 0.1463 | 0.1463 | No |
Table 3: Urodynamic findings of patients before and after 1 and 3 months of surgery.
| PFR in ml/s | At1 month | 3 month | ||
|---|---|---|---|---|
| No | %age | No | %age | |
| Improvement in PFR ml/s | - | - | 2 | 4.25% |
| Same | 1 | 2.10% | 21 | 44.68% |
| Decrease in PFR by 4or > 4 ml/s | 21 | 44.60% | 1 | 2.10% |
| Decrease in PFR 2 or <4 ml/s | 15 | 31.90% | 12 | 25.53% |
| Decrease in PFR by 1ml/s | 10 | 21.20% | 11 | 23.40% |
Table 4: Peak flow rate (PFR) changes after surgery in quantitative measurements as compared to pre-op measurements.
| Timing | Range | Mean | Normality test KS | p-value | Passed normality test | |
|---|---|---|---|---|---|---|
| IIEF | Before surgery | 18- 70 | 46.255 | 0.1539 | 0.0121 | No |
| At 1month | May-60 | 28.604 | 0.1651 | 0.0048 | Yes | |
| At 3month | May-68 | 38.976 | 0.1398 | 0.0391 | No | |
| EF | Before surgery | Oct-30 | 18.787 | 0.1757 | 0.0091 | No |
| At 1month | Apr-25 | 10.57 | 0.2196 | <0.0001 | Yes | |
| At 3month | Aug-30 | 17.6 | 0.1419 | 0.0189 | No |
Table 5: International Index of Erectile Function questionnaires (IIEF) and erectile function domain (EF) before and after 1 and 3 months of surgery, with special emphasis on erectile function domain.
| IIEF (no. and % age) | EF [erectile function] (no. and % age ) | |||||
|---|---|---|---|---|---|---|
| Grade | Preop | 1 month | 3 month | Preop | 1 month | 3 month |
| Severe dysfunction | 0 | 4 (9.3%) | 2 (4.65%) | 0 | 6 (13.95%) | 1 (2.3%) |
| Moderate dysfunction | 1 (2.3%) | 11 (25.58%) | 0 | 5 (11.62%) | 21 (48.83%) | 7 (16.27%) |
| Mild-moderate dysfunction | 13 (30.23%) | 23 (53.48%) | 18 (41.85%) | 11 (25.58%) | 8 (18.60%) | 16 (37.20%) |
| Mild dysfunction | 15 (34.88%) | 5 (11.62%) | 12 (27.90%) | 12 (27.90%) | 5 (11.62%) | 10 (23.25%) |
| Normal | 14 (32.55%) | 0 | 11 (25.58%) | 15 (34.88%) | 3 (6.97%) | 9 (20.95%) |
| Total no. of patients | 43 | 43 | 43 | 43 | 43 | 43 |
Table 6: IIEF and EF in patients before and after surgery in reference to grading from severe dysfunction to normal, calculated from standard IIEF–protocol.
| Variable | Criteria | 1 month | 3 month | ||
|---|---|---|---|---|---|
| No. | %age | No. | %age | ||
| Bladder dysfunction | Residual urine volume (usg) | 39 | 82.30% | 14 | 29.78% |
| IPSS | 42 | 89.70% | 13 | 27.65% | |
| Residual urine volume (udm) | 40 | 85.10% | 14 | 29.78% | |
| PFR (urodynamic method) | 37 | 78.72% | 13 | 27.65% | |
| Sexual dysfunction | IIEF | 24 | 55.81% | 13 | 30.23% |
| EF | 22 | 51.16% | 16 | 37.20% | |
Table 7: Summarizes results of our study.
Discussion
In our study total 47 male patients were included with age range of 20-76 (mean 55), majority of patients were above 50years of age. 40 (85%) patients presented with history of bleeding per rectum and 7 (15%) patients with history of altered bowel habits as major complaint. This was contradictory to other studies [20]. In about 81% of cases growth were felt per rectally by DRE, similar to literature available [21]. Considerable importance was given to preservation of pelvic autonomic nerve preservation and same were completely preserved in 42 (89%) patients, partially preserved in 3 (6%) patients and in 2 (4%) patients; status of pelvic autonomic nerve preservation was not known as per intra-operative findings. Total Mesorectal Excision, was carried in all patients and complete TME was performed in majority of patients that is 42 (90%) and partial TME in 5 (10%) of patients.
Bladder function
None of the p-values passed normality test i.e., change in p-value was insignificant. Residual urine volume was measured and any patient having residual urine more than 10 ml as compared preoperative measured residual urine volume in same patient was considered significant. Resultant bladder dysfunction was 82% and 30% after 1 and 3 months of surgery respectively. Using IPSS, resultant bladder dysfunction was 90% and 3 months post-surgery 33 patients were having same IPSS as before surgery, so at 3 months after surgery resultant bladder dysfunction was 28%. This is consistent with results with other studies i.e., Kim et al. [12], Maas et al. [22] and Ameda et al. [23], as the voiding dysfunction in their studies were 26%, 28% and 30% respectively.
Using urodynamics method resultant bladder dysfunction was present in 85% and 30% at 3 and 1 month post-surgery respectively. We again analysed bladder function by comparing peak flow rate (PFR) in ml/s. and the resultant bladder dysfunction was present in 37 (70%) and 13 (28%) after 1 and 3 months post-surgery respectively. These results are consistent with other the studies i.e., Srerk et al. [24], Havenga et al. [25] and Maurer et al. [26] and in which bladder dysfunction was 23%, 24% and 32% respectively. 2 patients required intermittent catherization, in none of the patients neurogenic bladder developed, overactive bladder developed in 4 patients, urinary incontinence was noticed 6 patients and in 2 patients weak stream developed post-surgery.
Sexual function
The preoperative IIEF was 18-70 (mean=46.255, p-value=0.0121) preoperatively normal IIEF was noticed in only 14 (33%) patients and majority of patients 15 (35%) were having mild dysfunction and mild to moderate dysfunction was present 13 (30%) patients. Resultant sexual dysfunction was found in 13 (30%) of patients. Our results were consistent with other studies cited in literature like Kim et al. [12], Nesbakken et al. [16] and Sterk et al. [24] in which sexual dysfunction was found in 25%, 28% and 38% patient respectively.
Erectile function domain of IIEF before surgery was 10-30 (mean=18.787, p-value=0.0091), EF domain was graded and normal EF was present only in 15 (35%) patients, mild dysfunction in EF was noticed in 12 (28%), mild-moderate in 11 (26%), moderate dysfunction in 5 (12%) and none of the patients were having severe dysfunction EF before surgery. Resultant dysfunction EF was found only 22 (51%) after 1months post-surgery and 16 (37%) patients after 3 months post-surgery. The p-value passed normality test at month but was negative 3 month post-surgery. So resultant dysfunction in EF domain was found only in these results are consistent with other studies like Nesbaken et al. [16], Sterk et al. [24], Maurer et al. [26], and Pocard et al. [27] in which erectile dysfunction was present in 28%, 38% and 44% respectively. Even though comparisons between studies are difficult due to differing exclusion criteria and outcome measures, widely varying rates of voiding and sexual dysfunction after rectal surgery have been reported in the literature (Table 8). Postoperative voiding and sexual dysfunctions frequently develop after rectal surgery. These complications may result from thermal damage, ischemic injury, nerve stretching, ligation and the local inflammatory effects to the hypogastric nerve and the sacral splanchnic plexus during pelvic dissection. Injury to the sympathetic supply results in detrusor instability and ejaculatory difficulties, whereas injury to the parasympathetic supply results in poor detrusor contraction and erectile dysfunction (ED) [14,28-31].
| S.no. | Author | No. of Patients | Voiding Dysfunction % | Erectile Dysfunction % |
|---|---|---|---|---|
| 1 | Havenga | 138 | 32 | 17 |
| 2 | Mass | 47 | 28 | 11 |
| 3 | Maurer | 60 | 24 | 24 |
| 2 | Nesbakken | 49 | 13 | 28 |
| 3 | Kim | 68 | 26 | 25 |
| 4 | Pocard | 9 | 0 | 44 |
| 5 | Sterk | 49 | 23 | 38 |
| 6 | Ameda | 52 | 30 | 88 |
Table 8: Total number of patients handled by the authors.
During rectal surgery, the ANP procedure causes less impairment of genitourinary function [22,28,31]. Similarly, our study showed no significant complications related to voiding. Based on our data, rectal cancer surgery with ANP showed excellent preservation of voiding function, after 3 months post-surgery, the results of the IPSS did not change significantly.
The transient decrease in Qmax (peak flow rate) might be explained by postoperative inflammatory changes in the perivesical tissues and the possible resolution of partial nerve damage with time, resulting in improvement and even complete recovery [24]. In our study pelvic autonomic nerve were identified in 45 patients and complete preservation-PANP was achieved in 42 (89%) patients and partial- PANP was achieved 3 (6%) and in 2 (4%) pelvic autonomic nerves were not identified. Previous studies suggested that partial preservation of the pelvic autonomic nerves was sufficient to attain eventual functional recovery in voiding function [32]. The main cause of postoperative sexual dysfunction is intra-operative injury to the neurovascular bundles; partial dissection of the pelvic plexus can also affect sexual function [27]. Results of studies on male sexual function after rectal cancer surgery show impotence rates varying from 20% to 50% [16,24,33]. Ameda et al. [23] reported that postoperative EF was a serious complication, even in complete nerve preservation [22]. Hendren et al. [34] also reported that a high rate of sexual dysfunction is detected after rectal cancer excision, despite the use of nervepreserving techniques. The incidence of erectile dysfunction (ED) depends on the extent of resection, which may be reduced with nerve preservation [28].
Results
The results of our study show a significant proportion of rectal cancer patients suffer from sexual dysfunction after surgery. Overall, 2 patients experienced a complete loss of erectile function and 6 patients noticed loss of libido. In 3 patients retrograde ejaculation was noticed and 5 patients noticed weak penetration power. These patients will need follow-up to see improvement in their sexual function. The intimate anatomic relationship of the superior hypogastric nerve, the bilateral inferior hypogastric plexus, and the bilateral cavernosal nerves to the rectum and prostate explains their possible risk of injury. The nerve damage might have occurred after the nerve to the bladder had branched off in the deep narrow pelvis where precise dissection may be more difficult. The high incidence of sexual dysfunction may be due to the vulnerability to nerve damage. Although many factors influence postoperative sexual dysfunction, we could not determine a statistically significant relationship between sexual dysfunction and well-known adverse factors such as patient’s age, stage, type of operation, smoking, radiotherapy and co-morbidities because of the relatively small sample size in our study.
If there is an iatrogenic erectile dysfunction, patients should be offered a phosphodiesterase 5 inhibitor, preferably in the early postoperative phase after taking the opposite partner in full confidence. In general there is a good response in 87% of patients, but the effect of such a drug is dependent on, at least partially, intact cavernous nerves to produce nitric oxide. Erectile function was satisfactorily improved by use of sildenafil (Viagra) only in 79% of male patients with ED after rectal excision for either rectal cancer or inflammatory bowel disease [35,36].
Conclusion
TME surgery for carcinoma rectum can produce better QOL in case a colorectal surgeon always tries to do it with meticulous preservation of autonomic nerves after identifying them and saving them from injury by sharps or cautery.
References
- Park K (2011) Epidemiology of chronic non-communicable diseases and conditions. Park’s Text Book of Preventive and Social Medicine. Banarasi Das Bhanot Publishers.pp: 353-361.
- Indian Council of Medical Research (ICMR)(2004) Non-Communicable Diseases in Annual Report 2003-2004.
- Bruder P (1993) Reducing costs: Who really wants to? Hosp Top 71:7-10.
- Stewart BW, Kleihues P (2003) World Cancer Report. IARC Press, Lyon.
- (2005) Guidelines for New Regional Cancer Centres. National Cancer Control Programme Guidelines1: 1-13.
- Wani MA,Jan FA,Khan NA,Pandita KK,Khurshid R, et al. (2014) Cancer trends in Kashmir; common types, site incidence and demographic profiles: National Cancer Registry 2000-2012.Indian J of cancer51:133-137.
- Javid G, Zargar SA, Rather S, Khan AR, Khan BA, etal. (2011) Incidence of colorectal cancer in Kashmir valley, India. Indian J Gastroenterol30:7-11.
- Takahashi T, Ueno M, AzeKurale (2000) Lateral node dissection and total mesorectal excision for rectal cancers. Dis Colon Rectum43: S59-S68.
- Heald RJ, Husband EM, Ryall RDH (1982) The mesorectum in rectal cancer clue to pelvic recurance ? Br J Surg69: 613-616.
- Enker WE (1992) Potency, cure and local control in the operative treatment of rectal cancer. Arch Surg 127:1396-1402.
- MilesWE (1971) Method for performing abdominoperineal excision for carcinoma rectum and terminal position of pelvic colon (1908). Lancet21: 361-364.
- Kim NK, Aahn TW, Park Jk, Lee KY, Lee WH, et al. (2002) Assessment of sexual and voiding function after TME with PANP in males with rectal carcinoma. Dis Colon Rectum45:1178-1185.
- Havenga K, Enker WE (2002) Autonomic nerve preservation-TME. Surg Clinic North America82: 1009-1013.
- Lee JF, Maurer VM, Block GE (1973) Anatomic relation of pelvic autonomic nerves to pelvic operation.Arch Surg 107: 324-328.
- Merit T, Murata A, Koyama M, Totsuka E,Saraki M (2003) Current status of ANP surgery for mid and lower rectal cancers, Japanese experience with lateral node dissection. Dis Colon Rectum46: 78-88.
- Nesbakken A, Nygaard K, Bull Njaa, Carlsen E, Eril LM (2000) Bladder and sexual dysfunction after TME. Br J Surg 87:206-210.
- Ridgway PF, Darzi AW (2003) Role of TME in management of rectal carcinoma.Cancer Control 10:205-212.
- Suh KW (2006) Total mesorectal resection and preservation of autonomic nerves. Korean J of Gastroenterology 47:254-259.
- Choi HY, Park K, Hwang DY, Moon SM (2008) Voiding and sexual dysfunction following TME-ANP for rectal cancer in males a prospective study. Korean J Urol 49: 1041-1045.
- Majumdar SR, Fletcher RH, Evans AT (1999) How does colorectal cancer present? Symptoms, duration, and clues to location. Am J Gastroenterol 94:3039-3045.
- McSherry C, Cornell G, Glenn F (1969) Carcinoma of the colon and rectum. Ann Surg 169: 502-509.
- Maas CP, Moriya Y, Steup WH, Kiebert GM, Kranenbarg WM, et al. (1998) Radical and nerve-preserving surgery for rectal cancer in the Netherlands: a prospective study on morbidity and functional outcome. Br J Surg85:92-97.
- Ameda K, Kakizaki H, Koyanagi T, Hirakawa K, Kusumi T, et al. (2005) The long-term voiding function and sexual function after pelvic nerve-sparing radical surgery for rectal cancer. Int J Urol12:256-263.
- Sterk P, Shekarriz B, Günter S, Nolde J, Keller R, et al. (2005) Voiding and sexual dysfunction after deep rectal resection and total mesorectal excision: prospective study on 52 patients. Int J Colorectal Dis20:423-427.
- Havenga K, Enker WE, McDermott K, Cohen AM, Minsky BD, et al. (1996) Male and female sexual and urinary function after total mesorectal excision with autonomic nerve preservation for carcinoma of the rectum. J Am CollSurg 182:495-502.
- Maurer CA,Z’Graggen K, Renzulli P, Schilling MK, Netzer P, et al. (1999) Total mesorectal excision preserves male genital function compared with conventional rectal cancer surgery. Br J Surg 88: 1501-1515.
- Pocard M, Zinzindohoue F, Haab F, Caplin S, Parc R, et al. (2002) Aprospective study of sexual and urinary function before and after total mesorectal excision with autonomic nerve preservation for rectal cancer. Surgery 131:368-372.
- Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK (1998) Rectal cancer: the Basingstoke experience of total mesorectal excision 1978-1997. Arch Surg133:894-899.
- Bruheim K, Guren MG, Dahl AA, Skovlund E, Balteskard L, et al. (2010) Sexual function in males after radiotherapy for rectal cancer. Int J RadiatOncolBiolPhys76:1012-1017.
- Keating J (2004) Sexual function after rectal excision. ANZ J Surg 74:248-259.
- Shirouzu K, Ogata Y, Araki Y (2004) Oncologic and functional results of total mesorectal excision and autonomic nerve-preserving operation for advanced lower rectal cancer. Dis Colon Rectum 47:1442-1447.
- Schmidt C, Daun A, Malchow B, Küchler T (2010) Sexual impairment and its effects on quality of life in patients with rectal cancer. DtschArzteblInt 107:123-130.
- Havenga K, Mmas CP, DeRuiter MC, Welvaart K, Trimbos JB (2000) Avoiding long term disturbances to bladder and sexual function in pelvic surgery particularly with rectal Cancer. SeminSurgOncol18: 23-43.
- Hendren SK, O’Connor BI, Liu M, Asano T, Cohen Z, et al. (2005) Prevalence of male and female sexual dysfunction is high following surgery for rectal cancer. Ann Surg242:212-223.
- Carrier S, Zvara P, Nunes L, Kour NW, Rehman J, et al. (1995) Regeneration of nitric oxide synthase-containing nerves after cavernous nerve neurotomy in the rat. J Urol153:1722-1727.
- Lindsey I, George B, Kettlewell M, Mortensen N (2002) Randomized, double-blind, placebo-controlled trial of sildenafil for erectile dysfunction after rectal excision for cancer and inflammatory bowel disease. Dis Colon Rectum45:727-732.
Relevant Topics
- Breast Cancer Surgery
- Colon Cancer Surgery
- Dermatologic Surgery
- Kidney Cancer Surgery
- Leukemia Surgery
- Lung Cancer Surgery
- Lymphoma Surgery
- Oesophageal Cancer Surgery
- Pancreatic Cancer Surgery
- Prostate Cancer Surgery
- Radiation Therapy
- Skin Cancer Surgery
- Stomach Cancer Surgery
- Throat Cancer Surgery
- Thyroid Cancer Surgery
Recommended Journals
Article Tools
Article Usage
- Total views: 4082
- [From(publication date):
March-2017 - Dec 19, 2024] - Breakdown by view type
- HTML page views : 3333
- PDF downloads : 749