Short Communication Open Access
Impact of Single-Breath Mindfulness Technique on Physician Burnout and Stress
Pflugeisen BM1*, Mundell K1, Ebersole D1, Drummond D2 and Chen D11Multi Care Health System Institute, Tacoma, WA, USA
- *Corresponding Author:
- Bethann Mangel Pflugeisen
Multi Care Health System Institute
Mailstop 315-C2-RS, PO Box 5299
Tacoma, WA, 98415-9915, USA
Tel: +1 253-403-3629
Fax: +1 253-403-3629
E-mail: Bethann.Pflugeisen@multicare.org
Received date: April 27, 2016; Accepted date: May 23, 2016; Published date: May 30, 2016
Citation: Pflugeisen BM, Mundell K, Ebersole D, Drummond D, Chen D (2016) Impact of Single-Breath Mindfulness Technique on Physician Burnout and Stress. J Community Med Health 6:430. doi:10.4172/2161-0711.1000430
Copyright: © 2016 Pflugeisen BM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Introduction: Stress and burnout among health care providers can have serious repercussions. Mindfulness techniques, particularly when delivered by abbreviated training programs, have been studied for their success in managing symptoms and perceptions of stress and burnout among health care workers serving at the bedside, in clinic, as specialists, and in administration.
Materials and Methods: Our suburban community hospital system introduced an eight week, video-module based, single-breath mindfulness technique training program to a group of 23 physicians with a range of experience (0-38 years; 48% primary care). Repeated measures ANOVA were used to evaluate changes across the study period (baseline, end of study, and 8 weeks post-intervention). Multiple linear regression was used to assess the relationship between burnout/stress measures at baseline and provider sex, age, years in practice, and field of practice (primary care or specialty).
Results: 19 (83%) providers completed the program and 12 (52%) completed assessments at each time point. Significant improvements were observed across the study period in emotional exhaustion (p=0.01), personal accomplishment (p=0.007), and stress (p<0.001). The extent to which providers depersonalize their patients was not significantly impacted (p=0.14). No significant associations were observed between provider characteristics and burnout/stress metrics at baseline. However, at the α=0.10 level, primary care providers reported a significantly lower sense of personal accomplishment (-6.0 points, 95% CI: -12.2, 0.2 points; p=0.08) at baseline.
Conclusions: Symptoms of stress and burnout are equally likely to be observed in providers across discipline, age, sex, and experience. A flexible, easy to use, single-breath based mindfulness program can yield significant improvements for these professionals.
Keywords
Mindfulness; Burnout; Stress; Physician
Introduction
High levels of stress and physician burnout, a “syndrome of depersonalization, emotional exhaustion, and a sense of low personal accomplishment [1],” can lead to increased medical errors [2,3], suboptimal patient care [2,4], and an increase in medical lawsuits [5]. Numerous studies in the US and abroad have investigated this phenomenon as it relates to work-life balance [6,7], field of medical practice [8,9], and sense of “calling” to the profession [10,11]. Several studies have illuminated that, for some physicians, burnout begins as early as medical school or residency [12-16]. Practices of mindfulness, or focusing attention and awareness on only the present moment, have been widely explored as antidotes to burnout for this professional community [1,17-21].
Traditional Mindfulness Based Stress Reduction (MBSR) programs, as they were originally conceived of by Kabat-Zinn in the early 1980s [22,23], were designed for patients battling chronic pain and other illnesses. These programs typically require a weekend retreat and weekly sessions lasting up to three hours over an 8-10 week period. Paradoxically, the demonstrated benefits of such programs are often difficult for physicians to achieve due to the intensive time commitment. In response, many researchers and health care systems, including our own, have implemented modified mindfulness programs designed to help health care providers develop the attention and awareness skills that are believed to be at the core of MBSR’s success, but which ease the burden of time for these busy professionals [24-26]. Indeed, we describe elsewhere [27] a flexible, video-module based mindfulness program that was developed and deployed for providers in our community hospital system. Here we holistically re-evaluate our program using a repeated measures analysis and we explore the relationship between characteristics of providers in our sample and burnout/stress metrics at baseline.
Materials and Methods
Using a single-breath mindfulness technique taught during a live session and built upon using freely accessible video-modules, we sought to improve the well-being and decrease stress and burnout in a cohort of physicians serving a suburban hospital in the South Puget Sound region of Washington State. For full details of our program, see Pflugeisen et al. [27]. The Maslach Burnout Inventory [28] and Perceived Stress Scale [29] were used to measure physician burnout and stress, respectively, at three time points: baseline (T1; September 2014), immediately following the 8 week intervention (T2; November 2014), and 8 weeks post-intervention (T3; January 2015). At each time point the tests were each administered in the early morning prior to the physicians starting their workday.
Here we use repeated measures ANOVA to evaluate the change in each of these four metrics across time (Table 1). To examine characteristics of providers experiencing burnout, we use multiple linear regression to evaluate the relationship between the burnout and stress metrics at baseline with select demographic variables, including practice field (primary care or specialty), provider sex (female/male), provider age, and years in practice. Significance was assessed at the 0.05 level and all analyses were conducted in the R statistical computing environment [30].
| Measure | Estimate (T1-T3)95% CI | F (2,22) | p |
|---|---|---|---|
| Emotional exhaustion | 8.3 (1.2, 15.5) |
5.7 | 0.01 |
| Depersonalization | 2.7 (-1.2, 6.5) |
2.2 | 0.14 |
| Personal accomplishment | -4.7 (-9.2, -0.1) |
6.2 | 0.007 |
| Perceived stress | 9.1 (3.8, 14.4) |
14.7 | <0.001 |
Table 1: Repeated measures ANOVA for physician burnout and stress scales.
Results
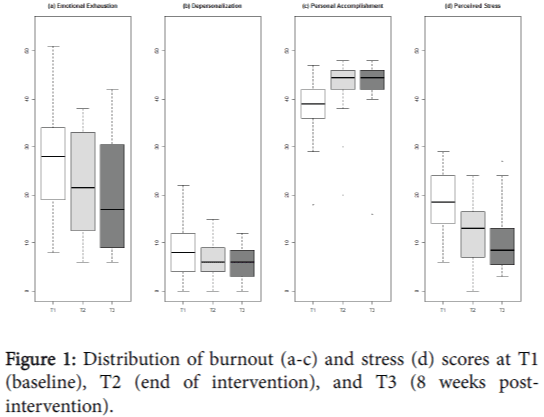
Twenty-three physicians enrolled in the pilot. Although 19 (82.6%) completed the program, only 12 (52.2%) completed all assessments at each time point. Mean emotional exhaustion, depersonalization, and stress decreased over the three time points, while providers’ sense of personal accomplishment increased over the 16 week period (Figure 1). While mean emotional exhaustion and stress continued to drop for study participants in the eight weeks post-intervention, depersonalization and sense of personal accomplishment remained constant between the end of the eight week intervention and follow up.
Repeated measures ANOVA revealed a significant association between time and emotional exhaustion (F2,22=5.7, p=0.01), with mean emotional exhaustion declining 8.3 points (95% CI 1.2-15.5 points; Figure 1a) over the sixteen week period. Similarly, perceived stress declined significantly (F2,22=14.7, p<0.001) across the study period, dropping 9.1 points (95% CI 3.8-14.4 points; Figure 1d) between T1 and T3.
Physicians’ sense of personal accomplishment rose during the intervention (Figure 1c) but plateaued during the follow up phase. Although personal accomplishment did not continue to rise, mean change over time was revealed to be significant for this metric (F2,22=6.2, p=0.007). Depersonalization alone did not demonstrate a significant improvement (F2,22=2.2, p =0.14) with a modest decrease of 2.7 points (95% CI -1.2 – 6.5 points; Figure 1b) across the study period.
Our study cohort was comprised of 11 (47.8%) primary care providers (Family or Internal Medicine), three (13%) Surgeons, two (8.7%) anesthesiologists, and seven (30.4%) physicians working in specialty practice, including Pediatric Neurology, Sleep Medicine, Clinical Informatics, Cardiology, Otolaryngology, Oncology, and Obstetrics/Gynecology. The cohort included nine (39.1%) women.
Neither status as a primary care provider nor female sex was significantly associated with the burnout or stress levels at baseline. However, at the a = 0.1 level, status as a primary care provider was associated with an average personal accomplishment score that was 6 points lower at baseline than that of specialists (95% CI -12.2, 0.2; p=0.08).
Mean age of the study cohort was 48.3 years, with participants ranging from 32-68 years of age. Average years in practice was 16.4, with as few as 0 years in practice for first year residents who enrolled in the program and as many as 38 years. Neither of these covariates were significantly associated with burnout or stress indicators at baseline (Table 2).
| Demographic variable | Summary information | Emotional exhaustion | Depersonalization | Personal accomplishment | Perceived stress | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimate 95% CI |
p | Estimate 95% CI |
p | Estimate 95% CI |
p | Estimate 95% CI |
p | |||
| Primary care provider [ N, % ] |
11 | 47.8% | -0.9 (-11.3, 9.5) |
0.86 | 1.1 (-4.4, 6.5) |
0.71 | -6.0 (-12.2, 0.2) |
0.08 | 0.9 (-5.7, 7.4) |
0.79 |
| Female [ N, % ] |
9 | 39.1% | 0.5 (-1.5, 2.5) |
0.63 | -0.4 (-1.4, 0.6) |
0.46 | -0.3 (-1.5, 0.9) |
0.62 | -0.01 (-1.2, 1.2) |
0.99 |
| Age [mean (SD), range] |
48.3 (10.0) | 32-68 | -0.3 (-2.4, 1.9) |
0.80 | 0.5 (-0.7, 1.6) |
0.43 | 0.5 (-0.8, 1.8) |
0.45 | 0.01 (-1.2, 1.4) |
0.87 |
| Years in practice [mean (SD), range] |
16.4 (10.5) | 0-38 | -4.5 (-15.5, 6.5) |
0.43 | -3.7 (-9.4, 2.0) |
0.22 | -0.4 (-7.0, 6.2) |
0.91 | 1.8 (-5.1, 8.6) |
0.62 |
Table 2: Association of demographic variables with burnout metrics at baseline.
Discussion
Physician burnout is an important and widespread phenomenon with serious implications for patients and providers alike when unaddressed. Our video-module based training program that focuses on a single-breath mindfulness technique was successfully implemented within a community hospital system for a diverse group of providers. Participants experienced a significant decrease in emotional exhaustion and stress during the study period as well as a significant increase in sense of personal accomplishment, and these improvements persisted eight weeks after the end of the program. The training did not significantly impact the extent to which providers depersonalized their patients.
Neither status as a primary care provider, female sex, age, nor years in practice were significantly associated with burnout and stress at baseline. This suggests that the prevalence of physician burnout is not discriminable by such characteristics, and that all health care providers are susceptible to burnout. We note that this study took place over what is typically deemed the “holiday season” in the United States, with the study ending the week before Thanksgiving and the follow up period occurring shortly after Christmas and New Year’s. This is typically perceived to be a very stressful time in the US, both personally and from a public health standpoint, lending anecdotal strength to the significance of our findings.
The primary limitation of our study is its small sample size, which is further hampered by poor fidelity to completion of assessments. We also did not include data collection on potential confounding factors related to lifestyle and personal history, such as smoking, use of drugs/ medications, history of depression, a sense of calling to the profession of medicine, and so on. These will be important things to consider in future studies. Additional work with the flexible, video-based format is needed. Beneficial studies would include using a larger sample to confirm the program’s overall success, exploring its impacts on more homogenous populations (i.e. a sample of exclusively primary care providers or exclusively specialists), and to expand its evaluation to additional types of providers at risk for burnout, such as nurses.
Conflicts of Interest
Dike Drummond is CEO of TheHappyMD.com. TheHappyMD.com did not finance the work related to this manuscript, is not financing the publication of this manuscript, and is not expected to benefit financially from the publication of this manuscript. The work that Dr. Drummond performed related to this manuscript was done under contract with MultiCare Health System. Should this manuscript be published, it is anticipated that Dr. Drummond will include the citation on TheHappyMD website. The other authors have no financial or non-financial conflicts of interest to declare.
Funding
Institutional
References
- Shapiro SL, Astin JA, Bishop SR, Cordova M (2005) Mindfulness-based stress reduction for health care professionals: results from a randomized trial. Int J Stress Management 12: 164-176.
- Williams ES, Manwell LB, Konrad TR, Linzer M (2007) The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Manage Rev 32: 203-212.
- Cimiotti JP, Aiken LH, Sloane DM, Wu ES (2012) Nurse staffing, burnout, and health care associated infection. Am J Infect Control 40: 486-490.
- Shanafelt TD, Sloan JA, Habermann TM (2003) The well-being of physicians. Am J Med 114: 513-519.
- Crane M (1998) Why burned-out doctors get sued more often. Med Econ 75: 210-218.
- Starmer AJ, Frintner MP, Freed GL (2016) Work-Life Balance, Burnout, and Satisfaction of Early Career Pediatricians. Pediatrics.
- Eckleberry-Hunt J, Kirkpatrick H, Taku K, Hunt R, Vasappa R (2016) Relation Between Physicians' Work Lives and Happiness. South Med J 109: 207-212.
- Abdo SM, El-Sallamy RM, El-Sherbiny AM, Kabbash IA (2016) Burnout among physicians and nursing staff working in the emergency hospital of Tanta University, Egypt. Eastern Mediterranean health J 21: 906-915.
- Lafreniere JP, Rios R, Packer H, Ghazarian S, Wright SM, et al. (2016) Burned Out at the Bedside: Patient Perceptions of Physician Burnout in an Internal Medicine Resident Continuity Clinic. J Gen Intern Med 31: 203-208.
- Yoon JD, Daley BM, Curlin FA (2016) The Association Between a Sense of Calling and Physician Well-Being: A National Study of Primary Care Physicians and Psychiatrists. Acad Psychiatry.
- Ford GA (2013) Physician burnout: "the call" derailed? South Med J 106: 295-296.
- Chan AM, Cuevas ST, Jenkins J (2016) Burnout Among Osteopathic Residents: A Cross-sectional Analysis. J Am Osteopath Assoc 116: 100-105.
- Fares J, Tabosh HA, Saadeddin Z, Mouhayyar EC, Aridi H (2016) Stress, Burnout and Coping Strategies in Preclinical Medical Students. N Am J Med Sci 8: 75-81.
- Lapinski J, Yost M, Sexton P, LaBaere RJ (2016) Factors Modifying Burnout in Osteopathic Medical Students. Acad Psychiatry 40: 55-62.
- Terrones-Rodriguez JF, Cisneros-Perez V, Arreola-Rocha JJ (2016) Burnout syndrome in medical residents at the General Hospital of Durango, Mexico. Rev Med Inst Mex SeguroSoc 54: 242-248.
- Zubairi AJ, Noordin S (2016) Factors associated with burnout among residents in a developing country. Ann Med Surg (Lond) 6: 60-63.
- Bazarko D, Cate RA, Azocar F, Kreitzer MJ (2013) The Impact of an Innovative Mindfulness-Based Stress Reduction Program on the Health and Well-Being of Nurses Employed in a Corporate Setting. J Workplace Behav Health 28: 107-133.
- Galantino ML, Baime M, Maguire M, Szapary PO, Farrar JT (2005) Association of psychological and physiological measures of stress in health-care professionals during an 8-week mindfulness meditation program: mindfulness in practice. Stress and Health 21: 255-261.
- Irving JA, Dobkin PL, Park J (2009) Cultivating mindfulness in health care professionals: a review of empirical studies of mindfulness-based stress reduction (MBSR). Complement TherClinPract 15: 61-66.
- Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, et al. (2009) Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 302: 1284-1293.
- Foureur M, Besley K, Burton G, Yu N, Crisp J (2013) Enhancing the resilience of nurses and midwives: pilot of a mindfulness based program for increased health, sense of coherence and decreased depression, anxiety and stress. Contemp Nurse 45: 114-125.
- Kabat-Zinn J (1982) An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. General hospital psychiatry 4: 33-47.
- Kabat-Zinn J, Lipworth L, Burney R (1985) The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med 8: 163-190.
- Fortney L, Luchterhand C, Zakletskaia L, Zgierska A, Rakel D (2013) Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: a pilot study. Ann Fam Med 11: 412-420.
- Klatt MD, Buckworth J, Malarkey WB (2009) Effects of low-dose mindfulness-based stress reduction (MBSR-ld) on working adults. Health EducBehav 36: 601-614.
- Mackenzie CS, Poulin PA, Seidman-Carlson R (2006) A brief mindfulness-based stress reduction intervention for nurses and nurse aides. ApplNurs Res 19: 105-109.
- Pflugeisen BM, Drummond D, Ebersole D, Mundell K, Chen D (2016) Brief Video-Module Administered Mindfulness Program for Physicians: A Pilot Study. Explore (NY) 12: 50-54.
- Maslach C, Jackson SE, Leiter MP (1986) Maslach burnout inventory. (Editor edn), California, USA.
- Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J health and social behavior 24: 385-396.
- R Development Core Team (2011) R: A language and environment for statistical computing. R Foundation for Statistical Computing.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 12408
- [From(publication date):
June-2016 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 11439
- PDF downloads : 969