Impact of Reamer Irrigator Aspirator versus Standard Reaming on Progression of Metastatic Bone Disease
Received: 01-Nov-2023 / Manuscript No. joo-23-122536 / Editor assigned: 03-Nov-2023 / PreQC No. joo-23-122536 (PQ) / Reviewed: 17-Nov-2023 / QC No. joo-23-122536 / Revised: 22-Nov-2023 / Manuscript No. joo-23-122536 (R) / Accepted Date: 29-Nov-2023 / Published Date: 29-Nov-2023
Abstract
Introduction: This study compared reamer-irrigator-aspirator (RIA) and standard reamer (SR) use in patients with metastatic bone disease (MBD) undergoing intramedullary nail (IMN) placement with regards to progression of MBD, complication rate, and overall survival. We hypothesize that RIA will reduce the rate of progression of MBD, reduce postoperative complications, and increase overall survival of patients with MBD.
Methods: One hundred forty-three patients (79 females, 64 males) with femur metastases were retrospectively analyzed after undergoing IMN placement with SR (122, 85.3%) or RIA (21, 17.2%) from 2009-2022. Patient demographics, oncologic and surgical history, complications, progressive disease, and survival were extracted from the medical record. Descriptive statistics including frequency counts and percentages for categorical variables as well as mean and standard deviation for continuous variables were used. Hypothesis testing with Fisher’s exact test for categorical variables and Student’s t-tests for continuous variables was performed. Finally, the Kaplan-Meier method was used to plot progression-free survival between RIA and SR groups.
Results: There were no statistically significant differences in length of operation, estimated blood loss, postoperative length of stay, complication rate, time to progression, time to death, or rates of postoperative cancer-specific mortality.
Conclusion: These findings failed to show a benefit to using RIA over SR; however, this study is limited by its small sample size and may be underpowered. Larger studies are needed to confirm these results.
Introduction
Bone is the third most common site of cancer metastases after liver and lung. Certain cancers, namely breast, prostate, thyroid, lung, and kidney, have a propensity to spread to bone with solitary or oligometastatic disease having longer overall survival than patients with widespread bony metastases [1]. Due to advances in systemic cancer treatment, the number of patients living with metastatic bone disease (MBD) continues to raise leading to increased rates of complications including pathologic fractures and bone pain. It has been estimated that half of patients treated for a pathologic fracture will die within 6 months of surgery and that around 350,000 people in the United States die with bony metastases each year [2,3]. The treatment of MBD in orthopedic oncology focuses on management of fractures, decreasing pain, and optimizing remaining quality of life. Surgery is often required and select patients can survive for several years postoperatively. Therefore, it is important to determine the most effective surgical management of impending or displaced pathologic fractures.
Intramedullary nailing (IMN) is frequently the operation of choice in patients with advanced MBD because it is fast, minimally invasive, and allows for early mobilization. The proximal femur is a common site for MBD and pathologic fractures. The efficacy of IMN in the setting of MBD can be seen in one review where 89-94% of patients experienced pain relief and improved or maintained function postoperatively. However, IMN was associated with a complication rate of 17% and a postoperative mortality rate of 4%. Additionally, there is variability in overall survival among patients with metastatic disease of the femur, with studies reporting survival times ranging between 5 and 17.5 months after IMN placement. Due to the poor prognosis and risk of complications, there is conflicting evidence on how to address impending pathologic fractures. Studies suggest there are improved outcomes after prophylactic fixation and standard of care utilizes the Mirels score to predict pathological fracture risk and determine surgical intervention indication [4-8].
A novel technique that may impact the complication and postoperative mortality rates of IMN is the use of the reamerirrigator- aspirator (RIA) (Synthes® Inc, West Chester, PA) during IMN placement in place of standard reaming (SR). A prior study conducted by Cipriano et al. suggests that by allowing for simultaneous irrigation and aspiration of intramedullary contents while reaming the bony canal and therefore preventing the systemic dissemination of malignant cells, the RIA may reduce risk of distant metastasis in MBD [9]. Additionally, the RIA may confer reduced risk of thermal necrosis and decreased risk of fat or tumor embolism, though these potential benefits need to be further explored [10]. RIA has been used to harvest bone grafts, treat intramedullary infections, and remove tumor cells prior to fixation of bones with metastases [11,12]. The aspiration of reamed material may be significant, and one notable study showed that cancer cells were retrieved by RIA during IMN placement in the femur. However, there is limited data on the impact of tumor cell retrieval by RIA on surgical and oncologic outcomes. Thus the purpose of this study was to compare outcomes of RIA versus SR use during IM nail placement in femurs with impending or complete fractures due to MBD. We hypothesized that RIA would reduce the rate of progression of MBD, reduce postoperative complications, and increase overall survival of patients with MBD.
Methods
This study was an Institutional Review Board approved retrospective chart review of patients with femoral bony metastatic disease treated with IMN for impending or complete pathologic femoral fractures between 2009 and 2022 at tertiary academic medical center and its affiliated country hospital.
Exclusion criteria
Patients with primary bone tumors and patients whose fracture was due to non-malignant causes (trauma and osteoporosis) were excluded. Patients with multiple IMN placements within 1-2 weeks of each other who had one operation with a standard reamer (SR) and one with a reamer-irrigator-aspirator (RIA) were excluded because the effect of RIA versus SR could not be adequately assessed. If patients had more than one IMN surgery within days to weeks of each other and all procedures used a single type of reamer, we used the date of the first procedure to calculate time to event.
Study parameters
Patient demographics, oncologic history, operative details, complications, perioperative radiotherapy, days to first progression, days to death, and cause of death were extracted from the electronic medical record. Operative details were extracted from the operative report, including reamer type. Progressive disease was identified using radiology reports. Type of progression was divided into progression at operative site, new metastatic disease, and progression of preexisting extramedullary metastatic disease. Complications included wound infections, hardware failure, deep vein thrombosis (DVT), pulmonary embolism (PE), myocardial infarction, respiratory failure requiring mechanical ventilation, intensive care unit (ICU) stay, and periprosthetic fracture. Survival data was collected, including death within 30 days after surgery and overall date of death.
Statistical methods
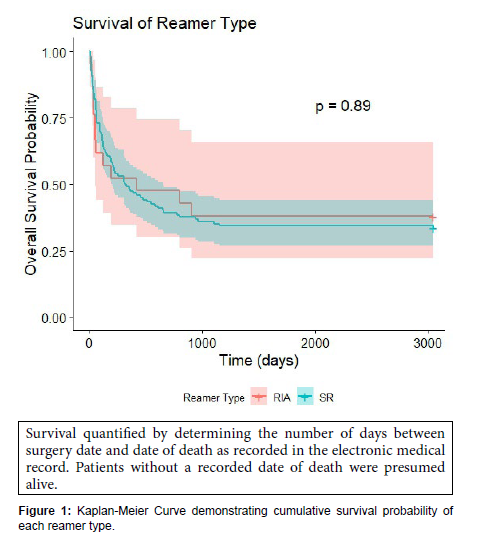
The Shapiro-Wilk test was performed to test the normality of continuous outcomes (length of unplanned hospitalization, days to first progression, age at death, days to death, and days to last followup). A t-test was performed and presented as mean and standard deviation (SD) if continuous outcomes were normally distributed, while the Wilcoxon rank sum test was performed and presented as median and interquartile range (IQR) if continuous outcomes were not normally distributed. Pearson’s Chi-squared test and Fisher’s exact test were conducted for the categorical outcomes and presented as count and percentage. Kaplan Meier survival analysis was conducted to show the effect of the reamer-irrigator-aspirator (RIA) and standard reamer (SR) groups on progression-free survival using the patient’s date of death. Survival quantified by determining the number of days between surgery date and date of death as recorded in the electronic medical record. Patients without a recorded date of death were presumed alive. All p values were two-sided, and the significance level was p<0.05. All tests were performed using R version 4.3.0 [13].
Results
Demographics
One hundred and forty-three patients with MBD of the femur were treated with 148 IMNs between 2009 and 2022. There was no statistically significant difference in age, sex, race, ethnicity, or pathologic diagnosis between the RIA and SR groups. IMN placement was performed with SR in 122 patients (85.3%) and RIA in 21 patients (17.2%). There were 43 patients with breast cancer (30.1%), 12 with prostate cancer (8.4%), 32 with lung cancer (22.3%), 25 with renal cancer (17.5%), and 31 patients with other types of cancer (21.7%) in the study population. This “other” category included: thyroid cancer, non-Hodgkin lymphoma, esophageal cancer, bladder cancer, parotid gland adenocarcinoma, hepatocellular carcinoma, duodenal adenocarcinoma, extraosseous Ewing sarcoma, colon cancer, melanoma, pancreatic cancer, hemangiopericytoma, and cholangiocarcinoma. A total of 19 surgeons performed the operations, and three of these surgeons used both RIA and SR in their practice (Table 1).
| Reamer Type | ||||
|---|---|---|---|---|
| Characteristic | Overall | RIA | SR | p-value2 |
| N = 1431 | N = 211 | N = 1221 | ||
| Sex (Female) | 79 (55.2%) | 14 (66.7%) | 65 (53.3%) | 0.3 |
| Race | 0.8 | |||
| Asian | 4 (2.9%) | 0 (0.0%) | 4 (3.4%) | |
| Black | 30 (21.4%) | 6 (28.6%) | 24 (20.2%) | |
| Caucasian | 104 (74.3%) | 15 (71.4%) | 89 (74.8%) | |
| Other | 2 (1.4%) | 0 (0.0%) | 2 (1.7%) | |
| Unknown | 3 | 0 | 3 | |
| Ethnicity (Non-Hispanic or Latino) | 101 (70.6%) | 14 (66.7%) | 87 (71.3%) | 0.7 |
| Ethnicity (Hispanic or Latino) | 38 (26.6%) | 7 (33.3%) | 31 (25.4%) | 0.4 |
| Pathologic Dx | 0.067 | |||
| Breast | 43 (30.1%) | 9 (42.9%) | 34 (27.9%) | |
| Prostate | 12 (8.4%) | 0 (0.0%) | 12 (9.8%) | |
| Lung | 32 (22.4%) | 8 (38.1%) | 24 (19.7%) | |
| Renal | 25 (17.5%) | 1 (4.8%) | 24 (19.7%) | |
| Other | 31 (21.7%) | 3 (14.3%) | 28 (23.0%) | |
| Length of operation (minutes) | 76.0 (62.5, 97.0) | 75.0 (67.0, 104.0) | 76.0 (62.0, 94.8) | 0.4 |
| Radiation Pre-operative | 14 (9.8%) | 4 (19.0%) | 10 (8.2%) | 0.13 |
| Radiation Post-operative | 59 (41.3%) | 8 (38.1%) | 51 (41.8%) | 0.7 |
| Radiation Dosage (cGy) | 2,000.0 (0.0, 3,000.0) | 2,000.0 (800.0, 2,750.0) | 2,000.0 (0.0, 3,000.0) | >0.9 |
| 1 n (%); Median (IQR) | ||||
| 2 Pearson’s Chi-squared test; Fisher’s exact test; Wilcoxon rank sum test | ||||
Table 1: Demographic characteristics of patients stratified by reamer type
Surgical and medical outcomes
Complication rates between SR and RIA groups were comparable. No statistically significant difference between post-operative rates of wound complications, hardware failures, and fractures was found between groups. Among SR patients, 1.6% experienced wound complications, with 0% in the RIA group (p > 0.9). Only one patient from each group experienced post-operative hardware failure (p = 0.3). Among SR patients, 2.5% experienced post-operative fracture, with 0% in the RIA group (p > 0.9). Post-operative rates of deep vein thrombosis did not differ among groups, with 4.1% in the SR group and 9.5% in the RIA group (p = 0.3). Similarly, pulmonary embolism rates were comparable, with 2.5% in the SR group and 4.8% in the RIA group (p = 0.5). Notably, there was no significant difference in unplanned reoperation rates between RIA (4.8%) and SR patients (2.5%) (p = 0.5).
In terms of medical complications and oncologic outcomes, rates of pulmonary and cardiac complications were not different between groups (p > 0.9). RIA and SR groups did not have significant differences in rates of local oncologic recurrence, with 5.2% of SR patients and 15% of RIA patients diagnosed with recurrence in the post-operative period (p = 0.13). There was no significant difference in rates of progression of existing metastatic disease or new diagnosis of metastatic disease between groups (p = 0.5, > 0.9, respectively). There was no statistically significant difference between rates of unplanned ICU stay or unplanned hospital readmission between groups (p = 0.2, >0.9).
Survival
There was no significant difference in post-operative death among groups, with 14.8% of SR patients and 14.3% of RIA patients passing within 30 days after surgery. (p > 0.9). Cumulative survival rates were comparable between both reamer groups (p = 0.89) (Table 2 and Figure 1).
| Reamer Type | ||||
|---|---|---|---|---|
| Characteristic | Overall | RIA | SR | p-value1 |
| N = 143 | N = 21 | N = 122 | ||
| Wound complication | 2 (1.4%) | 0 (0.0%) | 2 (1.6%) | >0.9 |
| Hardware failure | 2 (1.4%) | 1 (4.8%) | 1 (0.8%) | 0.3 |
| Fracture | 3 (2.1%) | 0 (0.0%) | 3 (2.5%) | >0.9 |
| DVT | 7 (4.9%) | 2 (9.5%) | 5 (4.1%) | 0.3 |
| PE | 4 (2.8%) | 1 (4.8%) | 3 (2.5%) | 0.5 |
| Pulmonary complications | 4 (2.8%) | 0 (0.0%) | 4 (3.3%) | >0.9 |
| Cardiac complications | 2 (1.4%) | 0 (0.0%) | 2 (1.6%) | >0.9 |
| Unplanned ICU stay | 12 (8.4%) | 0 (0.0%) | 12 (9.8%) | 0.2 |
| Died within or around 30 days | 21 (14.7%) | 3 (14.3%) | 18 (14.8%) | >0.9 |
| Require unplanned readmission | 6 (4.3%) | 1 (4.8%) | 5 (4.2%) | >0.9 |
| Unplanned reoperation | 4 (2.8%) | 1 (4.8%) | 3 (2.5%) | 0.5 |
| Local recurrence | 9 (6.6%) | 3 (15.0%) | 6 (5.2%) | 0.13 |
| New metastatic disease | 26 (19.1%) | 4 (20.0%) | 22 (19.0%) | >0.9 |
| Progression of metastatic disease | 45 (33.1%) | 8 (40.0%) | 37 (31.9%) | 0.5 |
| 1 Fisher’s exact test; Wilcoxon rank sum test; Pearson’s Chi-squared test | ||||
Table 2: Complication rates in Reamer Irrigator Aspirator group vs. Standard Reamer group
Discussion
Our study failed to demonstrate a difference in surgical and oncological outcomes in patients with metastatic bone disease (MBD) receiving femoral IMN with RIA versus SR for impending or complete pathologic fractures of the femur. Our findings are similar to another study by Streusel et al which found no statistically significant differences in fracture healing, length of hospital or ICU stay, pulmonary complications, or death in patients who underwent IMN for femur fractures using RIA vs SR [14].
Despite the established benefits of IMN in patients with MBD, there are undeniable complications associated with reaming. One study conducted by Karanko et al. noted worsening intra-and postoperative oxygenation status after intramedullary reaming in patients with MBD with a previously healthy baseline oxygenation [15]. Other observed risks of reaming include embolization leading to pulmonary embolism, arterio-occlusive disease secondary to a paradoxical embolism, and fat embolism during IMN nail placement in femurs, especially when nails are placed prophylactically [16,17]. The risk of emboli has been reported to be between 10.5% and 13% for IMN for impending pathologic fractures due to shaft metastases. Studies posit that these intraoperative embolic events are secondary to factors including increased intramedullary pressure which may force reaming fragments into systemic circulation, carrying these emboli to other organs [18- 20]. The pathologic hypervascularity of bone with secondary tumors and malignancy-associated coagulopathy may also play a role in embolization risk in MBD specifically.
A cadaveric study potentially identified an additional risk of reaming, tumor displacement distal to the initial lesion within the femur. The study posited that this displacement may lead to both spread of tumor cells and faster tumor growth within the bone, thus increasing destruction of the bone. This theoretical risk of new distant metastasis associated with reaming in the setting of metastatic disease has yet to be fully explored or established. Though one may presume that emboli associated with reaming may consist of cancerous particles that have become bloodborne during the high-pressure reaming process, this has not been proven.
The RIA aspirates intramedullary content while reaming to decrease intramedullary pressure. It has been hypothesized that through this reduction of intramedullary pressure, the RIA may lower the risk of embolic events associated with reaming. Van Gorp et al. found RIA significantly reduced intramedullary pressure by 86% proximally and 87% distally, keeping maximum pressure under 200 mmHg during simulated total knee arthroplasty on cadaver femurs [21]. This potential benefit of RIA, as compared, has been further explored in animal studies. Significantly lower intramedullary pressure was noted during reaming with RIA in pigs and sheep [22,23]. Decreased microemboli, decreased numbers of emboli in the lungs, and higher partial pressure of arterial oxygen with RIA use compared with SR use or no reaming in animal studies. Recently, a porcine model showed that an increased systemic inflammatory response is seen with SR or no reaming as compared to RIA [24]. Though the data for RIA in humans is sparser than animal studies, notable benefits that have been demonstrated include thermal necrosis prevention, decreased risk of fat embolism, decreased systemic inflammation, and shorter surgical time due to the single pass of RIA into the canal [25-29]. For oncology cases specifically, the RIA has been shown to be effective in obtaining tumor cells from the intramedullary space and can be used to take additional samples for histological evaluation [30].
When discussing potential benefits of RIA over SR, the risks associated with RIA must be noted. There is risk of eccentric reaming, cortical perforation, and iatrogenic fractures with RIA due to its larger size [31]. This is particularly important to consider in patients with MBD who have pathologic bone at baseline.
In this study, no adverse events related to RIA use were noted, with similar postoperative surgical and oncological outcomes in both groups. There were no significant differences in embolic events between reamer groups, as well as no difference in progression of metastatic disease or overall survival between the RIA and SR groups. This may suggest that the RIA does not eliminate or reduce the risk of micrometastatic embolization. However, it is important to note that the study included 148 cases total, which may be insufficient to detect differences in rare complications. While there appears to be a trend towards decreased rates of ICU stay and death within the first month after surgery when using RIA, numbers were not statistically significant due to the limited power of this study. Accordingly, multicenter trials with more patients are needed to further elucidate any potential benefit of RIA versus SR with IMNs in metastatic bone disease.
Limitations and future work
This study has important limitations. First, it is a retrospective study with no control group. The choice of RIA versus SR in this study is limited by selection bias on the part of the surgeon. We also had a small sample size of 143 patients and had fewer patients who underwent IMN placement with RIA than with SR. This study is thus limited by power, highlighting the need for a multi-institutional data set or, ideally, a multi-institutional randomized control trial to delineate the effects of RIA and SR in human subjects with MBD. Additionally, there were 26 patients total, with 5 in the RIA group and 21 in the SR group, who were lost to follow-up. Thus, survival probability may be over-reported. Finally, 19 different surgeons operated on the patients included in our study, but only 3 surgeons used both RIA and SR during IMN placement. We could not account for this variability of surgeons in a regression analysis due to the limited sample size. Thus, differences in surgical technique may have impacted patient outcomes.
Conclusion
Our study demonstrates no statistically significant differences between RIA and SR in the placement of IMN for MBD of the femur. Analyzing differences in outcomes between RIA versus SR during IMN placement is important for optimization of current surgical techniques in orthopedic oncology. Previous studies have shown promise, demonstrating that RIA prevents thermal necrosis, decreases embolic events, and decreases systemic inflammation compared to SR. In this study, RIA does not appear to reduce the risk of micrometastatic dissemination. Future studies utilizing multi-institutional cohorts and randomization may overcome the challenges faced in this study.
Acknowledgements
Thank you to our clinical, research, and administrative team members for their support throughout this project.
References
- Cappellari A, Trovarelli G, Crimì A, Pala E, Angelini A, et al (2023) New concepts in the surgical treatment of actual and impending pathological fractures in metastatic disease. Injury 54: S31-S35.
- Roodman GD (2004) Mechanisms of bone metastasis. New England journal of medicine 350: 1655-1664.
- Wood TJ, Racano A, Yeung H, Farrokhyar F, Ghert M, et al (2014) Surgical management of bone metastases: quality of evidence and systematic review. Annals of surgical oncology 21: 4081-4089.
- Ratasvuori M, Wedin R, Keller J, Nottrott M, Zaikova O, et al (2013) Insight opinion to surgically treated metastatic bone disease: Scandinavian Sarcoma Group Skeletal Metastasis Registry report of 1195 operated skeletal metastasis. Surgical oncology 22: 132-138.
- Gallaway KE, Ahn J, Callan AK (2020) Thirty-day outcomes after surgery for metastatic bone disease of the extremities: an analysis of the NSQIP database. JAAOS-Journal of the American Academy of Orthopaedic Surgeons 28: e1014-e1019.
- Ristevski B, Jenkinson RJ, Stephen DJ, Finkelstein J, Schemitsch EH, et al (2009) Mortality and complications following stabilization of femoral metastatic lesions: a population-based study of regional variation and outcome. Canadian Journal of Surgery 52: 302.
- Scolaro JA, Lackman RD (2014) Surgical management of metastatic long bone fractures: principles and techniques. JAAOS-Journal of the American Academy of Orthopaedic Surgeons 22: 90-100.
- Owen AR, Uvodich ME, Somasundaram V, Yuan BJ, Rose PS, et al (2022) Outcomes of Intramedullary Nail Fixation for Metastatic Disease: Impending and Pathologic Fractures. Anticancer Research 42: 919-922.
- Cipriano CA, Arvanitis LD, Virkus WW (2012) Use of the Reamer–Irrigator–Aspirator May Reduce Tumor Dissemination During Intramedullary Fixation of Malignancies. Orthopedics 35: e48-e52.
- Cox G, Jones E, McGonagle D, Giannoudis PV (2011) Reamer-irrigator-aspirator indications and clinical results: a systematic review. International orthopaedics 35: 951-956.
- Dehghan N, Schemitsch EH (2017) Extended applications of the reamer-irrigator-aspirator (RIA) system. Injury 48: S47-S51.
- Bellapianta J, Gerdeman A, Sharan A, Lozman J (2007) Use of the reamer irrigator aspirator for the treatment of a 20-year recurrent osteomyelitis of a healed femur fracture. Journal of orthopaedic trauma 21: 343-346.
- R Core Team (2013) R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna.
- Streubel PN, Desai P, Suk M (2010) Comparison of RIA and conventional reamed nailing for treatment of femur shaft fractures. Injury 41: S51-S56.
- Karanko MS, Helttula IO, Klemi PJ, Gullichsen REA (2010) Arterial oxygenation can fall critically during intramedullary nailing of pathological femoral fractures. Journal of Trauma and Acute Care Surgery 69: 1210-1216.
- Roth SE, Rebello MM, Kreder H, Whyne CM (2004) Pressurization of the metastatic femur during prophylactic intramedullary nail fixation. Journal of Trauma and Acute Care Surgery 57: 333-339.
- Kerr PS, Jackson M, Atkins RM (1993) Cardiac arrest during intramedullary nailing for femoral metastases. The Journal of Bone and Joint Surgery British volume 75: 972-973.
- Barre J, Lepouse C, Segal P (1997) Embolism and intramedullary femoral surgery. Revue de Chirurgie Orthopedique et Reparatrice de L'appareil Moteur 83: 9-21.
- Glover P, Worthley LI (1999) Fat embolism. Crit Care Resusc 1: 276-84,
- Högel F, Kamer L, Schlegel U, Rahn B, Südkamp NP, et al (2009) Fat extravasation due to unreamed and experimentally reamed intramedullary nailing of the sheep femur. Injury 40: 718-721.
- Van Gorp CC, Falk JV, Kmiec SJ, Siston RA (2009) The reamer/irrigator/aspirator reduces femoral canal pressure in simulated TKA. Clinical orthopaedics and related research 467: 805-809.
- Husebye EE, Lyberg T, Madsen JE, Eriksen M, Røise O (2006) The influence of a one-step reamer-irrigator-aspirator technique on the intramedullary pressure in the pig femur. Injury 37: 935-940.
- Smith PN, Leditschke A, McMahon D, Sample RR, Perriman D, et al (2008) Monitoring and controlling intramedullary pressure increase in long bone instrumentation: a study on sheep. Journal of Orthopaedic Research 26: 1327-1333.
- Miller AN, Deal D, Green J, Houle T, Brown W, et al (2016) Use of the reamer/irrigator/aspirator decreases carotid and cranial embolic events in a canine model. The Journal of Bone and Joint Surgery. American Volume 98: 658.
- Husebye EE, Lyberg T, Opdahl H, Laurvik H, Røise O (2010) Cardiopulmonary response to reamed intramedullary nailing of the femur comparing traditional reaming with a one-step reamer-irrigator-aspirator reaming system: an experimental study in pigs. Journal of Trauma and Acute Care Surgery 69: E6-E14.
- Wang RY, Li R, Zdero R, Bell D, Blankstein M, et al (2012) The physiologic and pathologic effects of the reamer irrigator aspirator on fat embolism outcome: an animal study. Journal of Orthopaedic Trauma 26: e132-e137.
- Halvachizadeh S, Teuben M, Lempert M, Kalbas Y, Cesarovic N, et al (2021) Protective effects of new femoral reaming techniques (Reamer irrigator aspirator, RIA I and II) on pulmonary function and posttraumatic contusion (CT morphology)–results from a standardized large animal model. Injury 52: 26-31.
- Volgas DA, Burch T, Stannard JP, Ellis T, Bilotta J, et al (2010) Fat embolus in femur fractures: a comparison of two reaming systems. Injury 41: S90-S93.
- Hartsock LA, Barfield WR, Kokko KP, Liles LL, Wind T, et al (2010) Randomized prospective clinical trial comparing reamer irrigator aspirator (RIA) to standard reaming (SR) in both minimally injured and multiply injured patients with closed femoral shaft fractures treated with reamed intramedullary nailing (IMN). Injury 41: S94-S98.
- Kanakaris NK, Morell D, Gudipati S, Britten S, Giannoudis PV (2011) Reaming Irrigator Aspirator system: early experience of its multipurpose use. Injury 42: S28-S34.
- Giannoudis PV, Tzioupis C, Green J (2009) Surgical techniques: how I do it? The Reamer/Irrigator/Aspirator (RIA) system. Injury 40: 1231-1236.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Callan KA, Patibandla SD, Powers CM, Hurd A, Cheng M, GallawayKE (2023) Impact of Reamer Irrigator Aspirator versus Standard Reaming onProgression of Metastatic Bone Disease. J Orthop Oncol 9: 238.
Copyright: © 2023 Callan KA, et al. This is an open-access article distributed underthe terms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1639
- [From(publication date): 0-0 - Jul 02, 2025]
- Breakdown by view type
- HTML page views: 1388
- PDF downloads: 251