Impact of Pre-Exposure Prophylaxis (PrEP) on Sexually Transmitted Infection (STI) Incidence among Men who have Sex with Men (MSM) in Mecklenburg County North Carolina
Received: 31-Oct-2022 / Manuscript No. JIDT-22-78662 / Editor assigned: 04-Nov-2022 / PreQC No. JIDT-22-78662(PQ) / Reviewed: 18-Nov-2022 / QC No. JIDT-22-78662 / Revised: 25-Nov-2022 / Manuscript No. JIDT-22-78662(R) / Published Date: 02-Dec-2022
Abstract
Impact of Pre-Exposure Prophylaxis (PrEP) on Sexually Transmitted Infection (STI) incidence among Men who have Sex with Men (MSM) in Mecklenburg County North Carolina.
Objective: This study aims to determine whether MSM who were prescribed Truvada for Pre-Exposure Prophylaxis (PrEP) have a higher incidence of Sexually Transmitted Infections (STIs) than MSM not using Truvada for PrEP.
Design: Primary analysis of longitudinal STI data obtained from MSM attending Rosedale Medical and Amity Medical Group in Charlotte North Carolina, USA, and January 2016-October 2018.
Methods: Men who have Sex with Men (MSM) individuals were identified and grouped into two, those who were prescribed PrEP and a second group not using PrEP (propensity score was used to match similar individuals). Patients’ STI data was used to compare the incidence of chlamydia, gonorrhea, and syphilis, and time to first symptomatic STI among PrEP users and nonusers.
Results: Propensity score matched 98 PrEP users to nonusers included in the analysis. Incidence Rate Ratios (IRRs) for chlamydia, gonorrhea and early syphilis were 3.2 {95% confidence interval (95% CI): 1.9-5.3}, 2.8 (95% CI: 1.7-4.6) and 2.9 (95%CI: 1.5-5.6), respectively, comparing PrEP users to nonusers. Time to first symptomatic STI was shorter among PrEP users (120 days, 95% CI: 77- 171) than among nonusers (185 days, 95% CI: 163-256).
Conclusion: Among MSM on PrEP, we observed a higher incidence of STIs and faster time to first symptomatic STI than MSM, not on PrEP. PrEP nonusers had a higher incidence of syphilis compared to PrEP users. However, there is insufficient evidence that PrEP maybe a contributing factor in increasing STI rates among MSM.
Keywords: Human Immunodeficiency Virus (HIV); Propensity- score; Survival analysis; Truvada; Pre-Exposure Prophylaxis (PrEP); Sexually Transmitted Infections (STI); Men who have Sex with Men (MSM)
Introduction
As part of the HIV comprehensive prevention strategy PrEP including safe-sex practices, regular HIV testing, HIV risk reduction counseling and consistent and correct condom use have been mostly effective. With PrEP, non-HIV positive individuals who are at high risk of HIV infection take antiretroviral medication daily to decrease their likelihood of becoming infected with HIV when they are exposed to the HIV virus during sexual acts. The PrEP pill (brand name Truvada) contains two medicines (tenofovir and emtricitabine) that are often used in combination with other medicines to treat HIV. When individuals are exposed to HIV through sex or injection drug use, these medicines work by preventing the virus from establishing a permanent infection [1]. Truvada when taken daily is highly effective for preventing HIV. Studies have shown that PrEP reduces the risk of getting HIV from sex by about 99% when taken daily, including for Men who have Sex with Men (MSM) the population mostly impacted by the disease. Among people who inject drugs, PrEP reduces the risk of getting HIV by at least 74% when taken daily. From 2014 to 2017, PrEP awareness is shown to have increased among MSM in 20 urban areas in the United States from 60% to 90%, and generally PrEP use increased from 6% to 35%. PrEP use increased in almost all demographic subgroups but has remained low among Black and Hispanic MSM [2]. Health care providers can play a critical role in ending the HIV epidemic by routinely testing patients for HIV, assessing HIV-negative patients for at-risk behaviors, and prescribing PrEP to patients as needed. Research has shown that increasing PrEP use is a principal strategy to ending the HIV epidemic [3]. Truvada was approved for use on July 16, 2012, by the U.S. Food and Drug Administration (FDA). Truvada for PrEP in combination with safer sex practices was approved to reduce the risk of sexually acquired HIV-infection in adults who are at high risk [4]. PrEP is less effective when use consistently and it does not protect against other STIs. PrEP only protects against HIV; condoms are important for the protection against other STIs. Condoms are also an important prevention strategy, especially if PrEP is not taken consistently [3]. Truvada for PrEP is being approved with a Risk Evaluation and Mitigation Strategy (REMS). PrEP REMS program engagement minimizes the risk to uninfected individuals of acquiring HIV infection and reduces the risk of development of resistant HIV-1 variants. The central component of the REMS is the training and education program that assist prescribers in counseling individuals who are taking or considering PrEP. The training and education program does not restrict the distribution of Truvada but provided information about the importance of adhering to the recommended dosing regimen and understanding the serious risks of becoming infected with HIV while inconsistently taking Truvada for PrEP.
REMS are an important aspect of PrEP that helps to support healthy sexual behaviors to prevent incidences of HIV and other likely STI while on Truvada [5]. The incidence of gonorrhea, chlamydia, and syphilis has risen sharply among men in the United States and other Western countries, with syphilis being disproportionately high in the MSM population. The sharp increase in the incidence of STIs among MSM may be coincidental with increased frequency of unprotected anal sex: in San Francisco for example, increasing proportions of MSM reported condomless anal sex in the preceding 12 months in the National Health Behavior Study during the 2005-2014 study period. In the study, persons attending sexually transmitted infection clinics also reported increases in the number of recent male sex partners in the same period. The motivation for decreased condom use may include confidence that the use of PrEP for prevention reduces transmission risk or the belief that HIV is no longer a serious health concern. In other studies of PrEP involving MSM, high rate of incident STI among MSM is has been shown to be driven by increasing rates of condomless sex. Condomless sex in the context of PrEP use may be only a part of the explanation for the increase in STI. Increase in STI incidence among MSM antedated the PrEP era. There is also an increasing rate of STI infection among already HIV-infected MSM. PrEP users are generally individuals with substantial risk for STIs, as well as HIV [2]. It is essential to know that these trends if they are broadly representative are not necessarily bad for STI control. Models from some studies have suggested that more frequent screening among MSM using PrEP might over time drive down rates of STIs. Such models assume STI screening increases substantially and STIs are appropriately treated when detected. There is also the possibility that more treatment of gonorrhea, for example, might promote the faster spread of antibiotic resistance Neisseria gonorrhoeae bacterium which may increase the spread of the disease. Routine STI testing has been part of PrEP studies, providing an opportunity for enhanced detection of asymptomatic infections. Certainly, evidence from randomized controlled trials would be needed to study these scenarios. Several studies have been conducted to understand the association between PrEP and STI over the years; however, very few studies have been published that address the association between PrEP and STIs in a non-experimental setting such as a clinic. Also, STIs are increasing in the United States at the same time as there is notably increase in the awareness and utilization of biomedical advances in HIV treatment such as Treatment as Prevention programs (TasP) and prevention with (PrEP) [6]. In the observed population of MSM the rates of reported new HIV incidence have stabilized and even declined in some geographical areas in the United States. On the population level, researchers suspect that the uptake of PrEP could contribute to increasing STI rates because the regular quarterly STI screening recommended for all people on PrEP may increase the detection of asymptomatic or recent STI infections [7]. Again, PrEP protects against HIV infection but does not offer protection against STIs such as syphilis, chlamydia, and gonorrhea, so the growing concern is that MSM who use PrEP have been observed to come in for STI treatment more frequently than before the initiation of PrEP [2].
The increase availability of urine testing, extragenital testing-rectal, and oral swabs has resulted in an increased number of MSM being tested for and diagnosed with an STI. However, the rates of infections varied among different racial and ethnic minority population in the United States including sub-populations such as MSM [8]. According to the Centers for Disease Control and Prevention CDC during 2015- 2016, the rate of reported gonorrhea increased by 22.2% among men. The magnitude of the increase among men suggests either increased transmission or increased case ascertainment (e.g., through increased extra-genital screening) among MSM or both [9]. In a similar report by the CDC during 2000-2016, the rise in the syphilis rate was primarily attributable to increased cases among men and, specifically, among MSM [10]. In 2016, men accounted for almost 90% of all cases of syphilis in the United States. Of those male cases for whom the gender of sex partner was known, 80.6% were MSM [11]. Additionally, reported cases of syphilis continued to be characterized by a high rate of HIV co-infection, particularly among MSM [12]. In 2016, 39,782 people were diagnosed with HIV infection in the United States [13]. In 2018, 37,968 people received an HIV diagnosis in the United States and the annual number of new diagnoses decreased 7% from 2014 to 2018 [14]. HIV testing has remained stable or increased in recent years, thus a decrease in diagnoses suggests a true decline in new infections [15]. This decrease may be due to targeted HIV prevention efforts; however, the progress has been uneven, and HIV diagnoses have increased among particular groups within the US-population. In Mecklenburg County, more than 6,837 persons are living with HIV and as many as 900 more may be infected but unaware of their status [16]. An estimated 103,009 MSM resided in North Carolina in 2013, representing 2.3% of the 4,503,084 MSM in the United States. Of the 3,536,017 adult men of North Carolina, 2.9% had had sex with another man in the past 5 years, which was less than the overall percentage of adult men in the United States who were MSM (3.9%). Most MSM in North Carolina resided in central counties of large metropolitan areas (38.8%) [17]. Among counties or county-equivalent areas in North Carolina, Mecklenburg County had the largest population of MSM at 20,920, representing 20.3% of all MSM in the state [18]. For adults and adolescents newly diagnosed with HIV in 2017, MSM accounted for 64.5% of all cases [19]. The Mecklenburg County Health Department (MCPH) initiated a pilot program to provide PrEP for HIV prevention in March 2018. Although the PrEP program for individuals with a high risk of contracting HIV has been in existence for some time there is little coordinated effort in delivery of PrEP to those who need it the most in the county. As a result, the surveillance efforts process focused on PrEP and STI trends in the county are needed. This is crucial to understand the trajectory of the impact of initiating PrEP and its relationship, if any, with STIs among MSM in the county since the extent of PrEP usage and practices in the county is unknown [20]. Truvada is provided free by the pharmaceutical manufacturer (Gilead) and the PrEP evaluation project monitors the PrEP program for patient enrollment rates, adherence, and new HIV infections while reporting STI diagnosis [21]. This data analysis on PrEP aims to compare the incidence rate of STIs among MSM who Truvada PrEP users and nonusers in two clinics are, Rosedale Medical and Amity Medical Group, in Mecklenburg County of North Carolina.
Methodology
Study design, setting, and population
This is a primary data analysis of MSM who prescribed PrEP from two clinics were, Amity Medical Group and Rosedale Medical, both in Mecklenburg County of North Carolina, between January 2016 and October 2018. This analysis study is part of a Mecklenburg County PrEP Project of 2018. Clinicians from both clinics evaluate all patients for PrEP eligibility at routine visits, and those who meet the recommended criteria are offered PrEP through the clinic. AthenaNet is the Electronic Medical Record (EMR) used to store and generate patient data for both clinics. This data includes the identification of MSM on PrEP, which was extracted for this analysis. Patients who are on PrEP are tested for HIV and STIs at their initial visit and are given (prescribed) a 3-month prescription for PrEP. They return 1 month after PrEP initiation, and then quarterly for clinical follow-up and monitoring, including HIV and STI testing. Included in this analysis are MSM who were prescribed PrEP, are HIV-negative and have at least 12 months follow-up period in the dataset. Our comparison group (Truvada PrEP nonusers) was composed of HIV-negative MSM who attended both clinics between January 2016 and October 2018 period. Also, to be included in this analysis patients must be 18 years or older and those who were HIV positive on the first occasion (January 2016) were excluded from the analysis. The comparison group was propensity score-matched to PrEP users. The rationale for this approach was that PrEP is not widely accessible or affordable to many MSM in the county so the data will be best comparable to PrEP nonusers in both clinics when propensity score-matched patients to similar controls [22]. The main variable of interest for this study is the incidence of STIs among MSM who prescribed PrEP was compared to MSM PrEP nonusers for the same period. Other covariates that were considered and controlled for in this analysis include patients’ age, race/ethnicity, marital status, education, alcohol use, and drug use. For this study, all terms and conditions of the Emory University Research Committee as set forth in the Policies and Guidelines of the University Research Committee was adhered to, including all methods with guidelines and regulations as established by Emory IRB. Informed consent was obtained from both clinics to use de-identified data from clinic EMR for the analysis after the nature of its use has been fully explained to the clinic’s responsible party. A waiver was received from the Institutional Review Board (IRB) of Emory University for participant’s informed consent requirement for this study. Also, there was no contact with individuals, and the individual’s right to privacy was not infringed. This study was approved by the Emory University Rollins School of Public Health Epidemiology Department. According to Emory University policy, neither approval from the ethics committee nor informed consent from the study populations is required for primary data analysis studies.
Propensity score matching and comparison group formation
The propensity score matching technique was used to select a group of comparison patients who were most similar to our PrEP users. These are MSM patients not on PrEP who present similarly as those on PrEP in both clinics at the same period of the investigation [23]. The goal of propensity score matching is to approximate the effect of randomization by balancing observed covariates between study groups [24]. Seven variables were included in the propensity score model, relating to STI diagnoses and demographic characteristics. Data for the propensity score model were from the initial PrEP visit for PrEP users and from the first clinic visit between January 2016 and October 2018 for PrEP nonusers [21]. Optimal fixed ratio matching 1:1 without replacement was used to select PrEP nonusers for each PrEP user based on their propensity scores.
Data sources, measures and data linkage
Data managers from both clinics with approval from the clinic’s management de-identified CSV data file of PrEP users and non-users who identify as MSM in both clinics was provided for this analysis. For both PrEP users and PrEP nonusers, we obtained data on demographics, clinic attendance, visit dates, PrEP status, and bacterial STI diagnoses from the clinic’s EMR. Bacterial STIs obtained for this analysis were gonorrhea, chlamydia, and syphilis. These were not categorized based on the different types and stages; rather, any diagnoses of bacterial STI including gonorrhea, chlamydia, and syphilis were included in the analysis. For example, EMR entries for the primary, secondary, latent (hidden), relapses of secondary and tertiary (late) stages of syphilis were concatenated, and the initial episode of syphilis based on treatment start date was used for the analysis. The treatment start date was also used to identify new incidence of gonorrhea and chlamydia to avoid duplicates of disease occurrence. The information on STI and disease incidence are stored as clinic encounter data and clinic encounter diagnosis and the treatment state date attached to the clinic encounter diagnosis reveals the date treatment was initiated. For incomplete treatment or failed treatment for any reason is entered as the clinic encounters follow-up date these data are dropped in the analysis.
Sexually transmitted infection testing
PrEP patients attend an initial evaluation (baseline) visit and patients who are prescribed PrEP are required to return to the clinic for a 1-month follow up. After the 1-month visit, patients are expected to make quarterly appointments for clinical follow-up and monitoring. MSM attending these clinics who were prescribed PrEP complete behavioral questionnaires for the intake process. Other MSM patients who are not prescribed PrEP go through the same intake process. Patients go through HIV and STI panel screening which includes testing for gonorrhea, chlamydia, and syphilis on initial clinic visits. Patients who are on PrEP are required to return to the clinic for their one-month STI screening after receiving the PrEP prescription and are also required to return quarterly after their first month for follow up visits. These quarterly visits involve HIV and STI screening [23].
Statistical analysis and follow-up time calculation
Poisson regression was used to compare the incidence of bacterial STIs between PrEP users and PrEP nonusers and Cox PH regression analysis used to investigate the effect of PrEP upon the time to STI. The semi-parametric model is appropriate for this analysis because it makes no assumptions about the shape of the baseline hazard. Other regression models that assume specific distributions for the survival times such as the exponential, Weibull, and log-normal distributions were not considered for this analysis. PrEP users were followed from their first PrEP prescription date for at least 12 months. Nonusers were also followed for the same period from the first clinic encounter date. During the follow-up period, both PrEP users and PrEP nonusers diagnosed with chlamydia, gonorrhea, or syphilis were counted as outcomes. To account for ascertainment bias resulting from more frequent STI screening among PrEP users, we compared time to first symptomatic STI between PrEP users and nonusers using Kaplan- Meier survival analysis, with follow-up time for both groups censored at the first diagnosis. We used a log-rank test to compare median time to first symptomatic STI between the groups. SAS 9.4 was used for all analysis and two-sided statistical tests were performed at a significance level of 0.05 [2].
Results
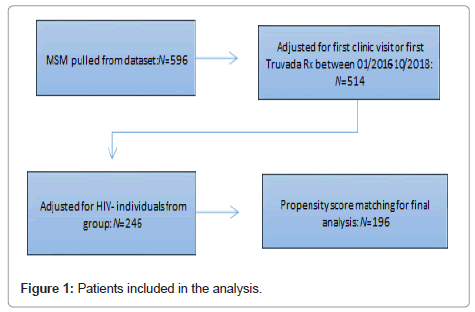
A total of 596 MSM patients from Amity Medical and Rosedale Medical clinic in Charlotte, North Carolina was extracted from clinics’ EMR. Using the initiation timeframe of January 2016 to October 2018 and an observation period of January 2016 to October 2019 allowing for individuals who initiated PrEP at the end of the initiation timeframe of October 2018 to have at least a one-year observation follow up period. A total of 514 MSM patients who had a first clinic visit date or first PrEP prescription fill date were extracted. This number was further reduced to 246 when HIV positive MSM were excluded from the analysis. PrEP users were propensity score-matched for PrEP nonusers based on demographics, resulting in a comparison group of 196 patients see Figure 1.
Among PrEP users, the median length of time contributed to the analysis is 1.65 years (Interquartile Range (IQR): 1.48-3.45). Both study groups were balanced in terms of age, race/ethnicity, and prior STI diagnosis. The mean age for the PrEP user groups was 35.7 years with a standard deviation of 11.3 years and the mean age for PrEP nonusers were 38.3 years with a standard deviation of 10.2 years. For both PrEP users and PrEP nonusers, most patients were between 18-39 years old. Half of both groups were non-Hispanic white. Of PrEP users, 10.2% had prior STI diagnosis, compared to 4.1% among PrEP nonusers (Table 1). Other variables including education, marital status, alcohol, and drug use were not significant (p-value > 0.05).
| Variable | PrEP nonusers | PrEP users | P-value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Age(M, SD) | 38.2(11.3) | 35.7(10.2) | 0.1087 | ||
| Race/ethnicity | |||||
| Non-hispanic black | 24 | 24.49 | 20 | 20.41 | 0.7821 |
| Non-hispanic white | 50 | 51.02 | 49 | 50 | |
| Hispanic any race/ethnicity | 6 | 6.12 | 9 | 9.18 | |
| Other | 18 | 18.37 | 20 | 20.41 | |
| Education | |||||
| High school diploma or less | 46 | 46.94 | 48 | 48.98 | 0.7749 |
| Post high school education | 52 | 53.06 | 50 | 51.02 | |
| Marital status | |||||
| Married | 11 | 11.22 | 11 | 11.22 | 0.9859 |
| Single | 62 | 63.27 | 63 | 64.29 | |
| Unknown | 25 | 25.51 | 24 | 24.29 | |
| Alcohol usea | 80 | 81.63 | 77 | 78.57 | 0.5914 |
| Drug useb | 18 | 18.37 | 17 | 17.35 | 0.8521 |
| Prior STI diagnosisc | 4 | 4.08 | 10 | 10.2 | 0.0961 |
Note: PrEP: Pre-Exposure Prophylaxis; SD: Standard Deviation; aAlcohol use: Yes or no, only yes was reported; bDrug use: Yes or no, only yes was reported; cPrior STI diagnosis: STI diagnosis before PrEP prescribed date for PrEP users and STI diagnosis for PrEP nonusers before clinic encounter date for the analysis period.
Table 1: Baseline characteristics of MSM patients from Rosedale Medical and Amity Medical Group in Mecklenburg County 2016-2018 (N=196).
Table 2 provides the incidence of each STI, comparing PrEP users to PrEP nonusers. Among PrEP users, the incidence of chlamydia, gonorrhea, and syphilis was 24.2, 16.6, and 8.9 per 100 person-years, respectively. PrEP users had an approximately four-fold higher incidence rate than PrEP nonusers for chlamydia (IRR: 4.4; 95% CI: 2.2-8.6), and approximately two-fold higher incidence rate for gonorrhea (IRR: 2.3; 95% CI: 1.2-4.5). Syphilis on the other hand was approximately three-fold high for PrEP nonusers compared to PrEP users (IRR: 0.3; 95% CI: 0.1-0.8). The analysis found that during a mean follow-up of 1.3 years (3185 person-years), there were 2928 STIs diagnosed (1434 chlamydia, 1242 gonorrhea, 252 syphilis) among 1427 (48%) of the total participants. Overall, the STI incidence was 91.9 per 100-person-years, with 736 participants (25%) accounting for 2237 (76%) of all STIs. The median time to STI diagnosis for PrEP nonusers was 858.5 days (IQR 14-1383) and that of users was 698 days (IQR 41-1306).
| STI | PrEP nonusers (n=98) incidence per 100 person years | PrEP users (n=98) incidence per 100 person years | IRRa | 95% CI |
|---|---|---|---|---|
| Chlamydia | 5.5 | 24.2 | 4.4 | 2.2-8.6 |
| Gonorrhea | 7 | 16.6 | 2.3 | 1.2-4.5 |
| Syphilis | 8.6 | 2.6 | 0.3 | 0.1-0.8 |
Note: IRR: Incidence Rate Ratio; CI: Confidence Interval; PrEP: Pre-Exposure Prophylaxis; aModel for IRR are clustered by patient ID and the IRR for MSM in both Rosedale Medical and Amity Medical Group in Mecklenburg County North Carolina per year for the duration of the analysis period 2016 to 2018; bModel was not adjusted for sub-categories of STI; all new STI cases within the analysis period were included.
Table 2: Incidence of STIs among PrEP users and nonusers attending Rosedale Medical and Amity Medical Group- Mecklenburg County (2016-2018), N=196.
The median time to chlamydia infection among PrEP nonusers was 984.5 days (147-1383) while among users it was 747.5 days (69-1306). The median time to gonorrhea infection among PrEP nonusers was 984.5 days (14-1383) while among users it was 768.5 days (41-1306). The median time to syphilis infection among PrEP nonusers was 925.5 days (15-1383) while among users it was 802.0 days (120-1306) see Table 3.
| STI | PrEP nonusers (n=98) | PrEP users (n=98) | p-value | ||
|---|---|---|---|---|---|
| Median time to event in daysa | IQR in days | Median time to event in daysa | IQR in days | ||
| Chlamydia | 984.5 | 147-1383 | 747.5 | 69-1306 | <0.01 |
| Gonorrhea | 984.5 | 14-1383 | 768 | 41-1306 | <0.01 |
| Syphilis | 925.5 | 15-1383 | 802 | 120-1306 | <0.01 |
Note: QR: Interquartile Range; PrEP: Pre-Exposure Prophylaxis; aMedian time to event, median time to STI.
Table 3: Time to STI among PrEP users and nonusers in Rosedale Medical and Amity Medical Group in Mecklenburg County North Carolina (2016-2018), N=196.
Also comparing MSM who are PrEP users to nonusers, the analysis indicates a four-fold higher incidence of chlamydia and a two-fold higher incidence of gonorrhea. However, PrEP users were also 2.5 times more likely to have had a prior STI diagnosis at baseline than nonusers. The analysis also indicates that syphilis has a three-fold higher incidence rate for MSM PrEP nonusers compare to PrEP users. Broad increases in STI screening and detection are occurring independently of PrEP, due to increased availability of free testing opportunity around the county for MSM in general [25].
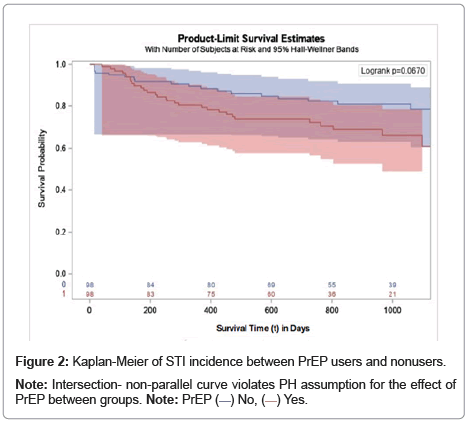
When comparing the survival time for both groups, MSM PrEP users showed a higher STI survival probability compared to nonusers see Figure 2. The result of the unadjusted effect of STI incidence (chlamydia, gonorrhea, and syphilis) from the Kaplan-Meier (KM) survival curve for this data indicate that MSM PrEP users have a better survival rate than MSM PrEP nonusers. In the crude comparison of time to STI between PrEP users and nonusers, there was no statistically significant difference (log-rank p=067, n=98). Before the first 200 days, PrEP users n=83 and PrEP nonusers n=84 were censored and by the end of the first 400 days, PrEP users n=75 and PrEP nonusers n=80 were censored. Over time PrEP nonusers were less likely to present with an STI diagnosis compared to PrEP users.
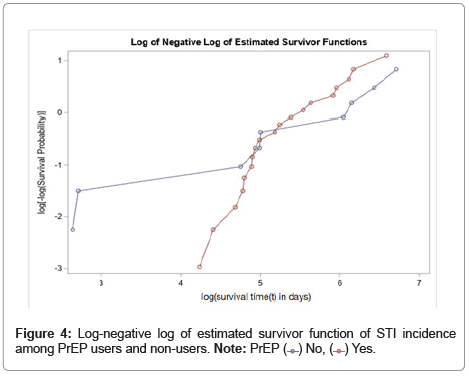
PH assumption violated
The survival curves are compared statistically to test the null hypothesis i.e., there is no significant difference regarding survival time to STI among the two groups. This null hypothesis is statistically tested using the log-rank test and the Cox PH test. The PH assumption is not satisfied because there is strong evidence of nonparallelism of the log- log curves. Further analysis was carried out to ascertain the difference in the incidence of STI if any by age category among PrEP users and nonusers. For this analysis, age was categorized as 18-29 years, 30-39 years, and 40+ years based on the age distribution of PrEP users. The age categories selected were constituted on the comparison of two study groups in a 2 2 table of counts, classifying into each combination PrEP users and PrEP nonusers. The number of individuals in each cell in the 2 × 2 table was similar. The frequency of age distribution between both groups was similar among PrEP users and nonusers for 30-39 years category. Overall, the KM survival curve indicates an increase in STI incidence among PrEP users compares to nonusers over time. This is an interesting finding because this age category 30-39 years had fewer PrEP users than any of the other age categories and its log-rank p-value is lower at 0.1957 than the other age categories. Overall, the KM survival curve indicates an increase in STI incidence among PrEP users compares to nonusers over time. This is an interesting finding because this age category 30-39 years had fewer PrEP users than any of the other age categories and its log-rank p-value is lower at 0.1957 than the other age categories.
In Figure 3, the survival curve for the adjusted age category 30-39 shows PrEP nonusers having a better survival rate for STI diagnosis compared to PrEP nonusers. At the end of the observational period ≈ 1000 days, only n=3 PrEP users were without an STI diagnosis compared to n=17 PrEP nonusers.
Discussion
As part of the PrEP program for those who engage in it, regular HIV and STI testing are required, and further findings suggest that PrEP use is associated with a higher risk of bacterial STIs incidence. These findings have been suggested to be a result of bias consistent with increased STI screening among PrEP users [6]. Other reports from the NC Mecklenburg County Health Department have suggested an increased incidence of syphilis among MSM. The independent t-test for chlamydia and gonorrhea outcomes was significant but was not significant for syphilis. The KM curve indicates the proportion of MSM PrEP nonusers at risk at time t (average of the true hazard ratio over time from initiation of PrEP for PrEP users and from fist STI diagnosis for PrEP nonusers at 120 days) for STIs is larger than the proportion of MSM PrEP users before the point of intersection, an indication that PrEP may have played a role in the risk of STI among MSM PrEP users in the first 120 days after PrEP use. However, after the intersection, PrEP use seems to have the opposite protective effect as users show a significant reduction in time to STI. The KM curve suggests a non-proportional hazard (PH) and because of the violation of the PH assumption where the true hazard ratio is changing over time, the Cox procedure may not be meaningful in estimating the between-group difference. Giving this situation, ‘non-proportional’ indicates that the effect of the independent variable (PrEP) is not constant over time. Hence, the hazard ratio is likely to change as time progresses. In general, the basic PH Cox model does not accommodate such effects where the independent variable is not constant over time; it is an average of the true hazard ratio over time. One of the main assumptions for the PH Cox model is that the hazards are proportional. The predictor variable PrEP does not satisfy the PH assumption since the graph of the survival function versus the survival time does not provide parallel curves. Similarly, the graph of the survival log of negative log plot of the survival time graph shown in Figure 4 result in unparalleled lines. The difference might be due to the true hazards being non-proportional or the variability of the variance in the tail estimates of the KM curves. Notably, at point 120 days the group total of 98 individuals has declined to a much smaller population still at risk. Both groups PrEP users and nonusers have individuals experiencing the event and individuals who are censored. Consequently, as the population at risk declines, the survival estimates become less certain due to fewer numbers of individuals available in the study at that particular time t. The 95% confidence intervals around the KM lines have increased width, an important statistic for the estimation of hazards as the population at risk and the number of events in the final period of the analysis is low. The final time period in the analysis contributes little to the estimates in the initial Cox model. The effect of small numbers of individuals represented in the final period of the analysis is that estimates of the hazards at those points in time in the analysis are uncertain. Further, based on the unadjusted STI incidence results from the analysis, it is uncertain whether the apparent violation of the PH assumption is due to chance or the effect of the significant difference in the variance of syphilis incidence between-groups. This suggests that the variance between-groups for the incidence of syphilis modifies the effect of the unadjusted KM curve of the unadjusted STI incidence between the groups. The result from this analysis will not be controlling of the effect modification because the effect modifier variable syphilis is also an outcome variable for the analysis. In recent studies, including two meta-analyses of STI incidence among PrEP users, published in AIDS, Kojima and colleagues shows that unadjusted rates for STIs among PrEP users in five studies, compared with low unadjusted rates for PrEP nonusers in 14 studies suggests increased incidence in STIs following PrEP initiation [26]. The study reported incidence of STIs among PrEP users in the range of 38.0- 56.7 per 100 person-years, 37.5-51.7 per 100 person-years, and 9.1-14.5 per 100 person-years for chlamydia, gonorrhea and syphilis, respectively [27]. These results are further supported by incidence of chlamydia and gonorrhea among PrEP users obtained from this analysis (24.2, 16.6, and 2.6 per 100 person-years, respectively) which were similar in proportion to this and other previous studies. However, unlike other studies, this analysis found that the incidence of syphilis was much lower among PrEP users compared to nonusers. Although the reported incidence of gonorrhea and chlamydia during PrEP use is somewhat similar to our group of MSM PrEP users, and the incidence of syphilis was higher among PrEP nonusers compare to users. Indeed, the hypothesis that PrEP users would experience higher incidence and faster time to first symptomatic STI was supported by the results in this analysis, providing evidence that PrEP use is associated with an increased risk of STIs independent of increased screening frequency. However, this analysis did not find evidence that PrEP use can be linked to increased incidence of syphilis. More research is required to understand why the incidence of syphilis did not follow a similar pattern as seen in other settings and documented reports [28]. Individuals who have once tested positive for syphilis will always have a reactive positive result for subsequent syphilis testing even after the successful treatment of an infection. To avoid a situation where the data captures used in this analysis count every reactive positive syphilis test, leading to possible double-counting, only new cases of initial positive syphilis infection were counted [29]. Possible reinfection of syphilis was also accounted for by reporting individuals’ prescriptions associated with syphilis found in clinic encounter diagnosis records of individuals. The method used for this analysis addresses several concerns in the data analysis approach for PrEP use and STI risk research, including the difficulty of comparison group formation, which has been a source of limitation present in many past studies. This analysis observed an increased STI risk among PrEP users relative to nonusers. Incidence of STIs among MSM has been increasing over the past decade in Mecklenburg County and nationally, and evidence that PrEP may be contributing to these increases is troubling. However, the findings of this analysis are not conclusive to suggest that PrEP initiation contributes to an increase in STI among MSM in Mecklenburg County. The significant difference in the hazard ratio over time for syphilis between-group with higher HR for PrEP users in this analysis is a cause for concern; nonetheless, these findings do not negate the tremendous success of PrEP as a tool for HIV prevention [25].
Limitations
There are several limitations to this analysis. First, those who were prescribed PrEP in either clinic may not be representative of the wider population of MSM in the county. Hence, selection bias may be present in this analysis as individuals who use these clinics may have unique characteristics that were not accounted for in the analysis, such as the individual’s address and type of insurance. Second, only clinical testing data were extracted and no data on STI treatments prescribed to participants were available; it is therefore not certain if every STI was treated effectively and if all positive diagnoses were incident infections. Third, though helpful in reducing within-group bias, propensity score matching assumes the variables included in the propensity score can predict the likelihood of PrEP use, but this is inconclusive. Such an assumption may result in biased estimates of the impact of PrEP on STI risk if not properly accounted for. There is a lack of comprehensive available data on STI screening frequency for both groups and it was assumed that each time individuals attend appointments in the clinics there is either an event or censoring. Resulting in an analysis of the incidence of symptomatic STIs and comparison of time to first symptomatic STI. Fourth, there was inconsistent data entry by clinic staff members, and this limits the quality of data available for a more robust analysis, which impacts the validity of the result to adequately respond to the research question. Therefore, our results should be interpreted with caution. Propensity score matching approximates the effect of randomization and allowed us to balance a large number of observed characteristics between study groups. Further, this method of comparison group formation enabled us to identify PrEP nonusers who were most likely to have been on PrEP, if it had been available [30].
Conclusion
The result from the analysis showed that among MSM PrEP users, the incidence of the STIs gonorrhea and chlamydia was higher than compared to nonusers, but the incidence of syphilis was higher among PrEP nonusers compare to users. Overall, these findings emphasize the importance of frequent STI testing among MSM using PrEP. Also, the results from this analysis demonstrated that STI prevention campaigns should not focus solely on condom use but also on reducing the time to STI diagnosis and treatment by promoting easy access to frequent testing. The results highlight the importance of ongoing screening and treatment of STIs among PrEP users as an important component of PrEP patient care, and PrEP programs can be leveraged to continue to engage MSM in more comprehensive STI prevention programs in the future. The success of PrEP programs may provide a unique opportunity to design and implement novel interventions to address increasing STI rates in the MSM population. The incidence of syphilis is of great concern, though this analysis did not conclusively link PrEP to STI there is a high incidence of syphilis in both groups. Also, the data entry process for these clinics needs attention, clinic staff, and administrators involved in patients’ data entry from intake to follow-up must apply standardized data entry and data quality control techniques. This would allow for more accurate capture of detailed events over time and provide valuable information to predict trends and study the relationship between PrEP and STIs.
Acknowledgments
The author wishes to thank Wesley J Thompson MHS, PA, AAHIVS, DFAAPA for his help with providing access to client data, and the staff at the Amity Medical Group Eastway Clinic. We also wish to thank Dr. Fredrick Cruickshank and Staff of Rosedale Medical Huntersville Clinic for the provision of patient data. We also wish to thank Bernard Davis MBA HCM and Tiffany Williams MPH for their contribution in seeing that this manuscript receives the highest quality critic. The author would also like to the Mecklenburg County Health Department “Get to Zero Program” and the PrEP Pilot Project for putting initiatives to combat the HIV epidemic in the county for their guidance and leadership.
Conflict of Interest Statement
There is no financial relationship or commitment of any size with any organization or persons in connection to this study from the past two years. In addition, there are no current negotiations regarding future employment or current job offers, either full- or parttime in connection to this study. There are no conflicts of interest in membership or affiliation to nongovernmental organizations that have an interest in the submission.
Declarations
Ethical approval
All research was reviewed and approved by the Emory University Institutional Review Board.
Competing interests
No financial disclosures to report. No conflict of interests to report.
Authors’ Contributions
Omerhi: Conceived and designed the analysis; Collected the data; Performed the analysis; Writing of manuscript.
Burks: Contributed to analysis tools; Contributed to writing of manuscript.
Funding
No funding to report.
Availability of Data and Materials
All datasets are available upon request to the Mecklenburg County Health Department, Emory University School of Public Health, and/or the primary author.
References
- McMahon JM, Myers JE, Kurth AE, Cohen SE, Mannheimer SB, et al. (2014) Oral pre-exposure prophylaxis (PrEP) for prevention of HIV in serodiscordant heterosexual couples in the United States: opportunities and challenges. AIDS Patient Care STDS 28:462-74.
[Crossref] [Google Scholar] [PubMed]
- Barreiro P (2018) Hot News: Sexually Transmitted Infections on the Rise in PrEP Users. AIDS Rev 20:71.
[Google Scholar] [PubMed]
- Teresa Finlayson PS (2019) Changes in HIV Preexposure Prophylaxis Awareness and Use Among Men Who Have Sex with Men-20 Urban Areas, 2014 and 2017. MMWR Morb Mortal Wkly Rep 68:597-603.
[Google Scholar] [PubMed]
- CDC (2012). NCHHSTP Newsroom.
- FDA (2012). FDA approves first drug for reducing the risk of sexually acquired HIV infection.
- Traeger MW, Cornelisse VJ, Asselin J, Price B, Roth NJ, et al. (2019) Association of HIV Preexposure Prophylaxis with Incidence of Sexually Transmitted Infections among Individuals at High Risk of HIV Infection. JAMA 321:1380-1390.
[Google Scholar] [PubMed]
- Schillinger J (2018) The intersection of prep and sexually transmitted infections: Prep works, now what? Croi. Atlanta: US Centers for Disease Control and Prevention.
- Jones ML, Chapin-Bardales J, Bizune D, Papp JR, Phillips C et al. (2019) Extragenital Chlamydia and Gonorrhea Among Community Venue-Attending Men Who Have Sex with Men - Five Cities, United States, 2017. MMWR Morb Mortal Wkly Rep 68:321-325.
[Crossref] [Google Scholar] [PubMed]
- CDC Sexually Transmitted Disease Surveillance (2019) CDC Sexually Transmitted Disease Surveillance.
- CDC Sexually Transmitted Disease Surveillance (2018) CDC Transmitted Disease Surveillance National Profile - Overview.
- CDC Sexually Transmitted Disease Surveillance (2019) CDC Sexually Transmitted Disease Surveillance National Profile.
- Patton ME, Kidd S, Llata E, Stenger M, Braxton J, et al. (2014) Extragenital Gonorrhea and Chlamydia Testing and Infection among Men Who Have Sex with Men-STD Surveillance Network, United States, 2010-2012. Clin Infect Dis 58:1564-1570.
[Crossref] [Google Scholar] [PubMed]
- CDC HIV HIV Public Health Partners Statistics Center (2020) CDC HIV.
- CDC HIV (2021) CDC HIV HIV Basics.
- McQuillan GM, Kruszon-Moran D, Masciotra S, Gu Q, Storandt R (2020) Prevalence and trends in HIV infection and testing among adults in the United States: The National Health and Nutrition Examination Surveys, 1999-2018. J Acquir Immune Defic Syndr 86:523-529
[Crossref] [Google Scholar] [PubMed]
- Nyki Hardy TH (2018) Getting to Zero Mecklenburg A Community Plan to Reduce New Cases of HIV in Mecklenburg County. Charlotte: Mecklenburg County Department of Health and Human Services.
- Grey JA, Bernstein KT, Sullivan PS, Purcell DW, Chesson HW et al. (2016) Estimating the Population Sizes of Men Who Have Sex With Men in US States and Counties Using Data From the American Community Survey. JMIR Public Health Surveill 2:14.
[Crossref] [Google Scholar] [PubMed]
- Grey JA (2016) Estimating the Population Sizes of Men Who Have Sex with Men in US States and Counties Using Data From the American Community Survey. JMIR Public Health Surveill 2.
[Crossref] [Google Scholar] [PubMed]
- North Carolina HIV/STD/Hepatitis Surveillance Unit (2018) 2017 North Carolina HIV/STD/Hepatitis Surveillance. North Carolina Department of Health and Human Services, Division of Public Health, Communicable Disease Branch, Raleigh.
- Harihar S, Witt B, Robinson P (2018) Pre-Exposure Prophylaxis (PrEP) Pilot in Mecklenburg County - Evaluation Project: Database and Management Considerations. UNC Charlotte College of Health and Human Services, APHi, Charlotte.
- Montaño MA, Dombrowski JC, Dasgupta S, Golden MR, Manhart LE, et al. (2019) Differences in sexually transmitted infection risk comparing preexposure prophylaxis users and propensity score matched historical controls in a clinic setting. AIDS 33:1773-1780.
[Crossref] [Google Scholar] [PubMed]
- Scott HM, Klausner JD (2016) Sexually transmitted infections and pre-exposure prophylaxis: challenges and opportunities among men who have sex with men in the US. AIDS Res Ther 13:1-5.
[Crossref] [Google Scholar] [PubMed]
- Saberi P, Berrean B, Thomas S, Gandhi M, Scott H (2018) A Simple Pre-Exposure Prophylaxis (PrEP) Optimization Intervention for Health Care Providers Prescribing PrEP: Pilot Study. JMIR Form Res 2:e2.
[Crossref] [Google Scholar] [PubMed]
- Xu Z, Kalbfleisch JD (2010) Propensity Score Matching in Randomized Clinical Trials. Biometrics 66:813-823.
[Crossref] [Google Scholar] [PubMed]
- Nguyen VK, Greenwald ZR, Trottier H, Cadieux M, Goyette A, et al. (2018) Incidence of sexually transmitted infections before and after preexposure prophylaxis for HIV. AIDS 32:523-530.
[Crossref] [Google Scholar] [PubMed]
- Harawa NT, Holloway IW, Leibowitz A, Weiss R, Gildner J, et al. (2017) Serious concerns regarding a meta-analysis of preexposure prophylaxis use and STI acquisition. Aids 31:739-740.
[Crossref] [Google Scholar] [PubMed]
- Kojima N, Davey DJ, Klausner JD (2016) Pre-exposure prophylaxis for HIV infection and new sexually transmitted infections among men who have sex with men. Aids 30:2251-2252.
[Crossref] [Google Scholar] [PubMed]
- Jenness SM, Weiss KM, Goodreau SM, Gift T, Chesson H, et al. (2017) Incidence of Gonorrhea and Chlamydia Following Human Immunodeficiency Virus Preexposure Prophylaxis Among Men Who Have Sex With Men: A Modeling Study. Clin Infect Dis 65:712-718.
[Crossref] [Google Scholar] [PubMed]
- Henao-Martínez AF, Johnson SC (2014) Diagnostic tests for syphilis: New tests and new algorithms. Neurol Clin Pract 4:114-122.
[Crossref] [Google Scholar] [PubMed]
- Calabrese SK, Earnshaw VA, Underhill K, Hansen NB, Dovidio JF (2014) The Impact of Patient Race on Clinical Decisions Related to Prescribing HIV Pre-Exposure Prophylaxis (PrEP): Assumptions About Sexual Risk Compensation and Implications for Access. AIDS Behav 18:226-240.
[Crossref] [Google Scholar] [PubMed]
Citation: Omerhi I, Burks LQ. (2022) Impact of Pre-Exposure Prophylaxis on Sexually Transmitted Infection Incidence among Men who have Sex with Men in Mecklenburg County North Carolina. J Infect Dis Ther S6:005.
Copyright: © 2022 Omerhi I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 904
- [From(publication date): 0-2022 - Sep 18, 2024]
- Breakdown by view type
- HTML page views: 739
- PDF downloads: 165

 ) No, (
) No, ( ) Yes.
) Yes.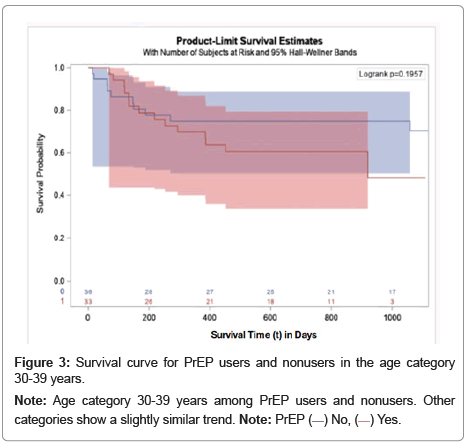
 ) No, (
) No, ( ) Yes.
) Yes.