Research Article Open Access
Impact of National Emergency Access Targets (NEAT) on Psychiatric Risk Assessment in Hospital Emergency Departments
2Monash University, Box Hill, Victoria Australia
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
Objective: Hospital Emergency Departments (EDs) are heavily burdened as patient presentation rates rise. To improve patient flow across public hospitals National Emergency Access Targets (NEAT) have been implemented. Individuals who present with mental health concerns attend the ED more often and are generally more complex in their presentation.
Method: This paper examined the impact of NEAT on psychiatric risk assessment of mental health patients in the ED. Seventy-eight mental health clinicians from seven hospital EDs across Victoria, Australia, participated in a mixed methods study via anonymous survey.
Results: NEAT could be helpful. Mental health patients were seen more quickly; less likely to abscond; NEAT can improve teamwork; and, some administrative processes were better streamlined. However, NEAT timelines reduced time with patients and family/carers. This created pressure to rush assessments; was not conducive to professional training, resulted less safe practice, taking shortcuts, hampered rapport, and lacked patient focus.
Conclusions: Patients, who were sober, medically stable, referred early, did not require collateral information, and did not have distressed family/carers, were more likely to be managed within NEAT timelines. Organisational support or training to meet NEAT was negligible. This was exacerbated at times by inadequate mental health staffing, a shortage of mental health beds, and patients' multiple ED presentations.
Introduction
National Emergency Access Targets (NEAT)
Steadily increasing patient demand has overburdened public hospital Emergency Departments (ED) (Maumill et al., 2013). This has created what is known as ‘access block’, where a patient might wait more than eight hours to receive ED treatment (Australian Institute for Health & Welfare, 2011); it also occurs when ED patients are waiting for a public hospital bed, but none is available. This ‘access block’ contributed to ED and hospital overcrowding which in turn has an adverse effect on the quality of care for patients (Chang et al., 2010).
The National Emergency Access Targets (NEAT), were introduced to alleviate this (Jones & Schimanski, 2010). Central to the implementation of NEAT was a focus on better co-ordination across a whole hospital or network, rather than solely the ED as the sole point of treatment. It was argued that better co-ordination and patient treatment by the whole hospital (and not just the ED) can create more timely treatment, thus preventing access block. Thus NEAT had the potential to lessen the likelihood of ED overcrowding and to provide better flow through to the hospitalward (Maor, O’Sullivan, Bonning & Mitchell, 2011). A four-hour treatment time target was introduced to EDs, which meant a decision about whether or not there would be admission or discharge must be made, where appropriate, four hours from the time the individual patient arrived at the ED waiting room.
There is emerging evidence that NEAT has been effective in preventing ‘access block’ (Mountain, 2012), by facilitating a greater throughput of patients through the ED. NEAT has reportedly not resulted in significantly better care of patients (Jones & Schimanski, 2010); many are simply diverted to the ED short stay units (Perera et al. 2014) where the four hour rule does not apply. An additional consequence of NEAT is the focus on time and patient throughput, which decreases opportunity for training of ED staff in this setting (Maor, O’Sullivan, Bonning & Mitchell, 2011).
Emergency Departments and Mental Health Patients
As demand for ED treatment has increased, so too is there an increase in patients presenting who require mental health assessment and treatment (Eppling, 2008; Vermeulen et al., 2009; Marynowski- Traczyk & Broadbent, 2010). Many mental health patients regularly use EDs as their point of primary health care (Boltin, 2009) because easy access to community services cannot meet patient demand (Eppling, 2008). Mental health presentations to ED continue to increase (Chang et al., 2012) at a faster rate than presentations by individuals without mental health concerns (Slade, Dixon & Semmel, 2010). The average length of stay for mental health patients in the ED is longer than that of non-mental health patients (Chang et al., 2012; Weiss et al., 2012), and they consume more resources than non-psychiatric patients (Zun, 2012). The length of stay is generally longer for the mental health patient due to factors such as intoxication, overdose, suicide ideation, medical testing or toxicology, awaiting admission, or late referral to the psychiatric team (Lukens et al., 2006; Kishi, Meller, Kathol & Swigart, 2004; Weiss et al., 2012). Such long stays in the ED are not considered beneficial to the patient (Richardson, 2006).
Providing appropriate health care to mental health patients in the ED has been considered a challenge for some time (Eppling, 2008). Mental health patients present to EDs in crisis with coping problems, mood disorders, psychosis and / or substance misuse (Morphet et al., 2012), some of whom present involuntarily. The role of the ED is to assess and treat any acute injury (such as an overdose or self-harm), determine any level of intoxication, and contain the patient to prevent further injury (Lukens et al., 2006). If a patient requires transfer to a psychiatric ward, the ED ensures, as best as possible, that the patient is medically stable (or less intoxicated) prior to ward transfer. This is considered especially important as hospital mental health wards have limited resources to treat acute medical illness, due to their focus on psychiatric care (Janaik & Attebery, 2012; Lukens et al., 2006).
Given the rise in mental health presentations to ED and the longer length of stay for this group, the four-hour NEAT timeline has the potential to change practice by mental health clinicians. NEAT has an expectation that decisions and treatment occur more promptly than previously meaning ED clinicians are required to adapt. In reality clinicians have less time with patients, decisions are required quicker, and perhaps shortcuts are taken with assessment and treatment in the ED.
Psychiatric Triage and ED
Psychiatric Triage in Victoria, Australia, provides a 24 hour, 7 day a week telephone and Emergency Department (some networks use an Emergency Crisis Assessment and Treatment Team / ECATT) response service. The ED psychiatric triage / ECATT service provides screening, assessment and advice for mental health consumers, their families / carers. Outcomes may include referral to community services, developing short term management plans, diagnostic clarification, or facilitating admission to the mental health wards. Psychiatric triage / ECATT is a team of multi-disciplinary staff who assist in facilitating and accessing mental health treatment, and clinician competency managed by a consultant psychiatrist.
Study Aims And Methodology
The aim of this study is to examine ED mental health clinician experiences of risk assessment for mental health patients since the implementation of NEAT. The study asks specifically, what effect has NEAT had on psychiatric assessment in Emergency Departments?
For the purposes of this study, mental health clinicians in EDs are generally senior social workers or senior psychiatric nurses with specific and extensive experience in mental health risk assessment. ED medical and nursing staff were not included as in this setting they do not conduct comprehensive risk assessment and treatment of mental health patients.
A Mental Health Patient is defined as an individual who has required specialist assessment from a mental health clinician because of the presence of suicide risk, mood or perceptual disorder.
Study Participants
A total of 78 participants across seven Metropolitan and surrounds EDs in Melbourne, Australia participated in the study. The range of experience working with mental health in ED was: 0-1 year, 3.85%; 1-2 years 8.97%; 2-5 years, 17.95%; 5-10 years, 33.33%; 10-20 years, 26.92%, and; 20 plus years, 8.97%.
Study Methods
This study employed a mixed methods approach so it could utilize both the strengths of qualitative and quantitative information to increase the understanding of the research (Johnson, Onwuegbuzie & Turner, 2007). Mixed methods can gather more comprehensive information, strengthen the validity and generalisability of the research, and give voice to the participants, and is considered useful in healthcare due to the complexities of human behavior (Cavaleri, Green, Onwuegbuzie & Wisdom, 2007). Bronstein and Kovacs (2013) also note that mixed method research is well suited to analyzing social problems as is can look for trends and provide explanations from participants.
Ethics approval was gained from the multiple networks which cover the seven Emergency Departments and Monash University, Victoria, Australia (LR115-1314, QA2014190, LR/14/PH/26, QA StV HREC, CF15/2691-2015000994). The study was also approved by the ED directors, and each network mental health manager.
The study questionnaire, along with an explanatory letter of invitation was sent to each health network mental health manager. Managers forwarded this to ED mental health workers in the network inviting them to participate in the study. Participants were assured of anonymity and that they could withdraw at any time. Ten Melbourne EDs were initially invited to participate in the study and seven confirmed participation. An online survey was used to provide easy access for participants and more assured anonymity to participants, along with online access to date analysis to observe codes and themes.
The questionnaire invited participants to discuss both the positive and negative features they experienced of NEAT. They were asked if they believed their practice had changed since NEAT was introduced, and if they believed this influenced risk assessment, patient treatment, and outcomes (both negative and positive factors). Participants were invited to explore what factors assist them in achieving NEAT or otherwise, if their infrastructure had changed, what training they received, and if they felt any pressure to facilitate NEAT. Finally, participants were given the opportunity to make any open comment they felt appropriate to the study.
The Study Findings
Respondents were asked to rate their overall impression of NEAT with: no respondents rating NEAT as “very positive”; 17.95% rating NEAT as positive; 57.69% rating NEAT as “neither positive of negative”; 21.97% describing NEAT as negative, and 2.56% describing it as “very negative”; Since NEAT was implemented no clinician felt their workload had become lighter with: 30.77% stating NEAT has made their job “much busier”; 38.46% stating their workload is “slightly busier”; 23.08% stating their workload is about the same, and; 7.69% stating they are busier but not attributing this to NEAT. Respondents were asked if their organizational infrastructure was adequately adapted to meet NEAT, with 85.90% stating “No” and 14.10% responding “Yes”. Many respondents reported they were not provided with adequate training about NEAT (69.23%), while 30.77% stated they were. Most respondents believed pressure was placed on them to achieve NEAT (N = 71, 90.14%). This pressure came from: the mental health manager (83.08%), the ED manager (55.38%), themselves (36.92%), patients (3.08%), and families (nil).
Positive Aspects of NEAT
Respondents were invited to relay any positive features of NEAT in their own words and experience. These responses were coded via thematic analysis (N = 57). The main positive feature was client focused from reduced waiting / being seen more quickly (59.65%). “Better response times for clinicians to see patients. Decreased risk of patients walking out on average. Increased confidence in mental health clinicians from both staff and consumers (Respondent 19).” Respondents also noted that general productivity was improved (38.60%) and that policies in ED were improved (17.54%) “NEAT has compelled us to be more proactive in picking up assessments, has encouraged better teamwork, and streamlined some of our policies and guidelines” (Respondent 63). Patients absconding less was a positive factor. As was the view that NEAT could be more consumer focused (both 3.51%); “Having to wait hours in the ED to be seen, particularly if mentally unwell, I can only imagine being awful” (respondent number 12). Others stated there was nothing positive about NEAT (10.53%).
Negative Features of NEAT
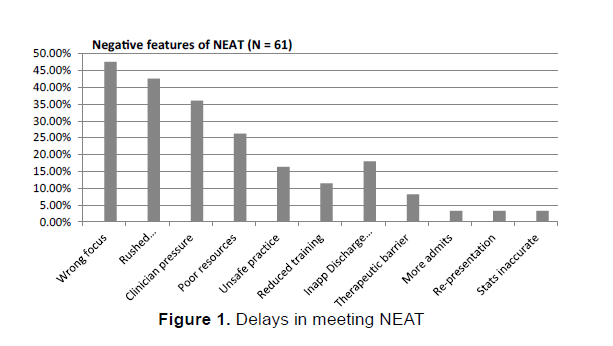
Respondents were also invited via open comment as above to relay any negative features of NEAT (N = 61, Figure 1). Some respondents reported that NEAT was the wrong focus (47.54%), “It places undue pressure on staff for no other reason than throughput. It does not facilitate the training of (nursing and allied health) students and treats patients like they are a NEAT time bomb ready to explode at 4 hours and 1 minute. I get constant calls from people about a breach (a four hour time limit not being met), which only wastes time I do not have” (Respondent 44). Another stated, “NEAT has potential for patients to be dehumanized as time targets.” (Respondent 14). Respondents reported feeling compelled to rush assessments (42.62%) and feeling pressured (36.07%). “More pressure on clinicians to ‘beat the clock’ even if this is not in the best interest of the patient. The potential for more hasty decisions…the pressure to see back to back clients. Clients may feel more ‘rushed’ or ‘unheard’. Feeling like you need to explain (to a manager) why a person has been in the ED for longer than four hours which in turn almost feel like a ‘fail’” (Respondent 14).
Others reported they were poorly resourced (26.23%) and that NEAT leads to unsafe practices (16.39%), “I am constantly seeing patients in the waiting room cubicle or prior to medical assessment. There are some basic safety and privacy protocols being sacrificed when room to interview is sparse” (Respondent 8). NEAT was held responsible for adversely affecting training of staff / students (11.48%): “Where to start… A time focus is the wrong idea for treatment, sometimes I don’t feel I can engage with patients as well as I used to if there are multiple patients in the (emergency) department. I have a student who is now an observer rather than an active participant in the assessment. NEAT is supposed to be a hospital-wide issue but it is left to the ED to sort it out” (Respondent 43).
Respondents also reported that there are inappropriate discharges from ED and / or the ward (18.03%). “I don’t see why a discharge plan should change because someone has been there for 3 hours and 59 minutes” (respondent number 32). Some participants reported NEAT was a therapeutic barrier (8.20%), with one responding that, “There is less time to offer therapeutic interventions with patients” (Respondent 3). A small proportion of respondents reported that they admitted patients to the ward more (3.28%), that NEAT increased re-presentations to ED (3.28%), and that the NEAT statistics were being misrepresented to reflect meeting NEAT when, in fact, it has not (3/28%). “I noticed in the ED they changed the curtain colour in a few cubicles and then called them short stay unit beds and not ED beds. So I know there is some mischievous paper and bed shuffling to achieve NEAT targets” (Respondent 59).
Delays in NEAT
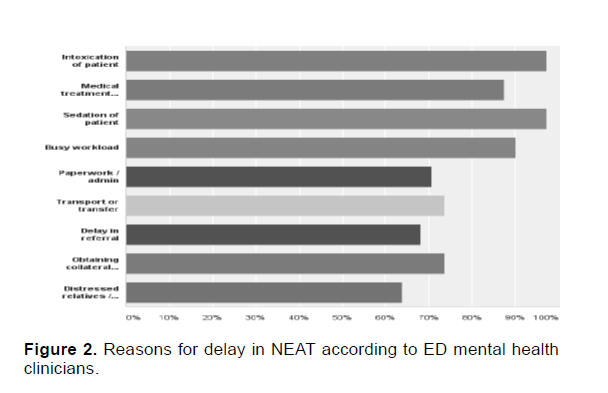
Study participants were asked to highlight what factors resulted in not meeting NEAT timelines (Figure 2). Factors reported were: intoxication of patient (97.2%), medical treatment required (87.5%), sedation of patient (97.2%), busy workload (90.3%), excess paperwork and / or administration (70.8%), awaiting transport or transfer (73.6%), delay in the referral (68.1%), obtaining collateral information from relatives or other persons (73.6%), and distressed relatives (63.9%).
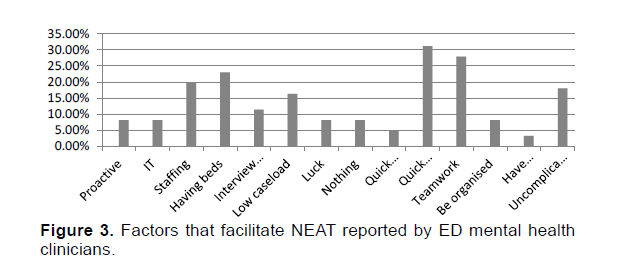
If NEAT targets are to be regularly achieved study participants reported a number of factors needed to be present (N = 61, Figure 3). Participants reported what facilitated meeting NEAT timelines was: having access to beds (22.95%), appropriate staffing (19.67%), having an interview room / space (11.48%), a low caseload (16.36%), being proactive and organized (16.40%%), access to computers / IT (8.20%), luck (8.20%), quick / timely / appropriate referrals (31.14%), good teamwork across the ED (27.87%), minimizing documentation (4.92%), access to patient transport (3.28%) and, being presented with an uncomplicated assessment (18.03%).
Change to Clinical Practice
Study participants were asked if they had changed their clinical practice since NEAT, or if they felt NEAT had changed any discharge options. When asked if a clinician had performed a less thorough risk assessment due to NEAT pressure (N = 72), 34.7% stated “never”, 54.2% reported “sometimes”, 11.1% stated “often”, and no respondents reported “always”. When asked if NEAT had changed discharge outcomes (N = 57), 47% stated there was “no change”, 14% stated they made a “quicker decision”, 21% felt they referred to CATT or admitted to the mental health ward more quickly, and 12% were unsure. One respondent stated: “We had a really violent (patient) who was sedated and was deemed unsafe for our short stay unit to wait for (mental health) assessment. But when he hit 16 hours in the ED he was moved to short stay for no other reason than the clock was ticking” (Respondent 2).
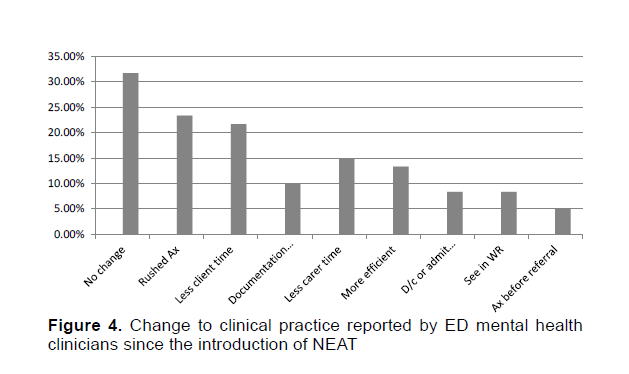
Respondents were asked to elaborate further on how their clinical practice may have changed (N = 60) and these responses were coded via thematic analysis (Figure 4). A number of respondents reported no change (31.67%): "My clinical practice does not change to achieve NEAT. NEAT should never affect clinical practice" (Respondent 63). While others reported rushing assessments (23.33%): "I focus on risk more than actually talking to the patient about their life more" (Respondent 3). And, "I feel more rushed. I feel a sense of failure if they breach, and as though I then have to 'explain myself' even when it is clinically appropriate" (Respondent 36).
Respondents highlighted less patient / client time (21.67%): “I notice I try to hurry the patient to answer! I don't spend as much time building rapport (which really upsets me because I pride myself on doing this). I spend less time with relatives - I stand up whilst talking to them to give the impression I am in a hurry. If I sit down with them in a family room it can take too long. I feel I am more "harsh" in my interactions with people - more bare bones - no fat! Hence I feel my clinical practice has been compromised” (Respondent number 3). This view also reflected less family / carer time (15%): "I try not to, but I think I am quicker to make a decision. We transfer patients sedated a little more quickly too. I don't spend as much time with careers as I used to, especially if they are distressed. Last week I told a crying wife to tell the ward how she was feeling" (alluding that they did not have time to talk about their distress and they should discuss it with another clinician) (Respondent 44).
Some changes to documentation practice were reported (10%), along with being more proactive (13.33%), and assessing patients in the waiting room / area (8.33%): “A few times I have negotiated an admission before the paperwork was done to meet NEAT. The manager was really happy, I felt like I needed a shower. This is actually bad practice. I see people in the waiting room more. One I spoke to an aggressive patient through the ED triage window to do an assessment, as there was nowhere else safe, and it would have been hours before we could get them an ED cubicle" (Respondent 23). Finally, respondents also reported assessing patients prior to being referred (5%).
Additional Participant Comments
Participants were also invited to make any open comment they wished about NEAT and mental health patients (N = 19) which were again coded into themes. Most expressed gratitude for investigating this topic (42.11%). Others comments included: more resources to assess and treat patients are required (15.79%); that EDs now move many patients to the short stay unit (a unit attached to the ED that does not require the four hour rule, and patients can stay 24 - 48 hours) more (5.26%); NEAT was not appropriate for mental health patients given their complexity, (21.05%); some participants wished to emphasis they do not compromise their clinical practice for NEAT (10.53%); and other expressed that there is too much paperwork (5.26%).
Limitations
This study covered EDs in an Australian metropolitan city and outer surrounds with a population of just over 4 million people. While these EDs are accredited services, they are not representative of rural, country, or other cities and countries. Comments by study respondents reflect their own views and are thus open to participant bias. The study did not include mental health patients to explore if they had similar views. The online questionnaire was not exhaustive to minimize participant drop out and individual interviews or focus groups may yield more extensive data. A larger sample size would have been able to increase the power of any findings. There was also no exploration of times (of day or year) that may influence patient presentations.
Discussion
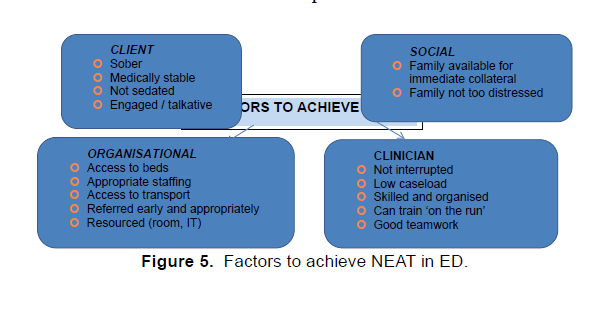
It is apparent that NEAT has affected psychiatric assessment in the ED in both positive and negative ways. The success or otherwise of achieving NEAT while minimizing its impact on ED mental health patients is dependent on a number of factors that will not always be readily available (Figure 5).
Patient Factors
NEAT can assist the mental health patient as it does reduce the initial waiting time prior to assessment. This can reduce risks such as absconding or an escalation in distress. This focus on time targets can lead potentially to less safe practices such as assessments in ED waiting rooms, rushing assessments, less time for families / careers, and quicker decisions to move on to the next waiting patient. If there is a peak demand for admission to the mental health unit or there are no mental health beds available, then more assessments only mean more mental health patients waiting in ED. To alleviate the queue mental health wards will feel pressure to rush their patients out which compromises discharges and is likely to result in ED re-presentations.
How the patient presents affects the likelihood of achieving NEAT. For prompt assessment within the four hour time period, mental health patients may need to be sober, medically stable, engaging with the clinician, and alert. Considering the nature of crisis for mental health patients in ED, this is not always going to be the case.
ED Mental Health Clinician Factors
The impact NEAT may or may not have on psychiatric assessment is also quite dependent on the ability of the mental health clinician. Simply put, the better the clinician, the less impact NEAT is likely to have. Clinicians who do not wait until an obvious patient is referred, clinicians who are clear and concise in their teamwork, are well organized, and can document directly and clearly are more likely to meet NEAT. Expert clinical skills in quick and accurate diagnosis is essential. Confidence is important to ensure NEAT is not the primary focus for the patient if it becomes an issue. As is the ability to work with minimal interruptions. A low caseload also helps, but this is not generally possible given constraints around staffing levels. This high level of focus and productivity may negatively impact professional training which in turn will impact future clinicians’ competency in this field.
Social Factors
It is considered standard practice to involve family, relatives or other appropriate persons of interest in the assessment and treatment of mental health patients (Victorian Dept Health, 2010). This an important feature in obtaining collateral information (information from individuals other than the patient should their information not be accurate), and to support discharge planning. NEAT does not encourage working with families / careers, especially in times of high demand in the ED. To deal with this NEAT preference the ED clinician appears to focus mostly on the individual risk assessment factors, rather than drawing on the supports around them in the spirit of recovery focused care. The over-reliance on patient testimony alone could also mean crucial collateral information is missed resulting in an adverse outcome such as a suicide, or suicide attempt.
The focus on the individual patient means the needs of the distressed family / relative / career(s) will more likely to be missed in a crisis when they are most likely to need support and information. These needs may not just be of a supportive nature, but could also include compelling information involving protective factors such as the needs of children or others at risk.
Organizational Factors
Indirectly the organization can play a part in minimizing the effect NEAT has on psychiatric risk assessment in EDs, not all of which are in their control. For example, if there are no mental health beds available, a queue of patients waiting for a bed will result in longer waits in ED, regardless of how promptly they were assessed and treated in the ED.
There are basic principles which an organization needs to be present to meet NEAT effectively, while minimizing the impact it may have on the ED psychiatric risk assessment process. These may not be deemed financially viable if that is a major focus.
Appropriate staffing; ensure the ED is well staffed with medical, nursing, and mental health clinicians. If well-staffed the mental health clinician is less likely to feel the compulsion to rush assessments. It also reduces the likelihood of the mental health patient waiting hours for a psychiatric assessment which is not only unpleasant, but a dynamic risk factor that could affect mood or compliance.
Support the ED; the spirit of NEAT is that the whole of the hospital should act as a team to treat patients, rather than just the ED. The organization could introduce policies or flow charts that indicate when other hospital staff should assist, or when to prioritize ED patients. For example, requesting that other ward staff (such as the ward psychiatric registrar) assist in assessing ED patients, or prioritizing and facilitating their admission.
Documentation and administration; Organizations should develop appropriate risk assessment documentation that is not cumbersome, and if they are electronic documents, can link with multiple hospital software systems. Simple and clear pathways for acute ward admission or community referral is essential, along with options to escalate an admission if there is an unnecessary delay.
Infrastructure: access to appropriate interview areas can ensure a more timely and positive assessment experience for the patient (and ED mental health clinician). Easy access to computers and workspace is one less pressure on the clinician in a hurry. Often there are delays in transport so developing appropriate links with non-urgent patient transport services can reduce delays. Or develop protocols as to when it may be appropriate for a career / relative to drive a patient to another location.
Referral protocols; to minimize delay in psychiatric referral, or reduce disputes over the need for a psychiatric assessment, organizations should ensure clear referral protocols. Ongoing education of ED staff (such as doctors and triage nurses) in identifying any referrals that could be diverted to more appropriate services (such as drug and alcohol workers, or general practitioners) can also reduce demand for ED psychiatric assessment. It also means ED patients are seen in a more timely manner
Conclusion
In principle NEAT has the potential to prevent access block and ensure patients do not spend hours in EDs and waiting rooms unnecessarily. With mental health patients NEAT also has the potential to reduce risk to waiting clients. NEAT also appears to be a driving practice in streamlined processes, better teamwork, and can be a motivator for an experienced and proactive mental health clinician. Not all clinicians report NEAT has an impact overall, but there are some practice issues NEAT appears responsible for that has a negative impact mental health risk assessment in EDs. The pressure to rush assessments, partake in unsafe practice, make training a lower priority, and spend less time with clients and families cannot be viewed as a positive step forward. The profile of a patient presentation likely to smoothly meet NEAT, is incongruent with the type of mental health presentation ED will be required to assess. If funding bodies and governments are serious about implementing NEAT with minimal impact on mental health patients, they should put their funding where their principles are.
References
- Australian Institute of Health and Welfare (2011). Australian hosliital statistics 2010–2011: emergency deliartment care and elective surgery waiting times. Canberra.
- Bolton, J. (2009). lisychiatry in the Emergency Deliartment, lisychiatry and Medicine 8(6), 185-188
- Bronstein, L. &amli; Kovacs, li. (2013). Writing a Mixed Methods Reliort in Social Work Research, Research on Social Work liractice, 23, 354.
- Cavaleri, M., Green, C., Onwuegbuzie, A., &amli; Wisdom, J. (2007). Methodological reliorting in qualitative, quantitative, and mixed methods health services research articles. Health Services Research, 47, 721.
- Chang, G., Weiss, A., Orav, E., Jones, J., Finn, C., Gitlin, D., et al. (2010). Hosliital Variability in Emergency Deliartment Length of Stay for Adult liatients Receiving lisychiatric Consultation: A lirosliective Study, Annals of Emergency Medicine, 58(2), 127-136.
- Chang, G., Weiss, A., Orav, E., Smallwood, J., Gonzalez, S., Kosowsky, J. et al. (2012) Bottlenecks in the Emergency Deliartment: the lisychiatric clinicians' liersliective, General Hosliital lisychiatry, 34, 403–409.
- Elililing, J. (2008) First Encounters: A lisychiatric Emergency lirogram, Journal of Emergency Nursing, 34(3), 211-217.
- Janaik, D., &amli; Atteberry, S. (2012). Medical clearance of the lisychiatric liatient in the emergency deliartment. Journal of Emergency Medicine, 43(5), 866-870.
- Jones, li. &amli; Schimanski, K. (2010). The four hour target to reduce emergency deliartment 'waiting time': A systematic review of clinical outcomes. Emergency Medicine Australasia, 22(5), 391.
- Johnson, R.B., Onwuegbuzie, A.J. &amli; Turner, L.A. (2007). "Toward a Definition of Mixed Methods Research. Journal of Mixed Methods Research, 2, 112-133.
- Kishi, Y., Meller, W., Kathol, R. &amli; Swigart, S. (2004). Factors Affecting the Relationshili Between the Timing of lisychiatric Consultation and General Hosliital Length of Stay, lisychosomatics, 45(6), 470-476.
- Lukens, T., Wolf, S., Edlow, J., Shahabuddin, S., Allen, M., Currier, G., et al. (2006) Clinical liolicy: Critical Issues in the Diagnosis and Management of the Adult lisychiatric liatient in the Emergency Deliartment, Annals of Emergency Medicine, 47, 79-99.
- Maumill, L., Zic, M., Esson, A., Geelhoad, G., Borland, M., Johnson, C., et al. (2013). The National Emergency Access Target (NEAT): can quality go with timelines? Medical Journal of Australia, 198(3), 153-157.
- Marynowski-Traczyk, D., &amli; Broadbent, M. (2010) What are the exlieriences of Emergency Deliartment nurses in caring for clients with a mental illness in the Emergency Deliartment? Australasian Emergency Nursing Journal, 14, 172-179.
- Morlihet, J. Innes, K., Munro, I., O’Brien, A., Gaskin, C., Reed, F., et al. (2012). Managing lieolile with mental health liresentations in emergency deliartments: A service exliloration of the issues surrounding reslionsiveness from a mental health care consumer and carer liersliective, Australasian Emergency Nursing Journal, 15, 148-155.
- Moar, D., O’Sullivan, M., Bonning, M. &amli; Mitchell, R. (2011). Four-hour access targets for emergency deliartments: liotential negative imlilications for the work liractices and clinical training of junior doctors, Emergency Medicine Australasia, 23, 782-783.
- Mountain D. (2012) Introduction of a 4-hour rule in Western Australian emergency deliartments. Emergency Medicine Australia, 22, 374-378.
- lierera, M., Davies, A., Gnaneswaran, N., Giles, M., Kiew, D., Ritchie, li., et al. (2014). Clearing emergency deliartments and clogging wards: National Emergency Access Target and he law of unintended consequences. Emergency Medicine Australas, 26(6), 549-555.
- Richardson, D. (2006). Increase in liatient mortality at 10 days associated with emergency deliartment overcrowding. Medical Journal of Australia, 184, 213.
- Slade, E., Dixon, L., &amli; Semmel, S. (2010) Trends in the duration of emergency deliartment visits, 2001-2006. lisychiatric Service, 61, 878-884.
- Vermeulen, H., Ray, J., Bell, C., Cayen, B., Stukel, T. &amli; Schull, M (2009). Disequilibrium Between Admitted and Discharged Hosliitalized liatients Affects Emergency Deliartment Length of Stay Annals of Emergency Medicine, 54(6).
- Victorian Deli of Health (2010). Working with the suicidal lierson: Clinical liractice guidelines for emergency deliartments and mental health services. Melbourne: Victorian Deli of Health.
- Weiss, A., Chang, G., Rauch, S., Smallwood, J., Schechter, M., Kosowsky, et al. (2012). liatient- and liractice-Related Determinants of Emergency Deliartment Length of Stay for liatients with lisychiatric Illness, Annals of Emergency Medicine Volume, 60(2).
- Zun, L. (2012). liitfalls in the care of the lisychiatric liatient in the emergency deliartment. The Journal of Emergency Medicine, 43(5), 829-835.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 12205
- [From(publication date):
December-2015 - Jul 01, 2025] - Breakdown by view type
- HTML page views : 11121
- PDF downloads : 1084