Impact of In-Patient Palliative Care Consultation on Patient Outcomes in Advanced Breast Cancer - A Retrospective Review
Received: 14-Mar-2024 / Manuscript No. jpcm-24-129487 / Editor assigned: 16-Mar-2024 / PreQC No. jpcm-24-129487 / Reviewed: 29-Mar-2024 / QC No. jpcm-24-129487 / Revised: 01-Apr-2024 / Manuscript No. jpcm-24-129487 / Published Date: 08-Apr-2024
Abstract
Background: Palliative care is a holistic patient-centered approach that aims to address the physical, emotional, social, and spiritual needs of patients with serious illnesses. Advanced Breast Cancer (ABC) poses significant challenges to patients and their families requiring comprehensive supportive and palliative care interventions to improve patient's quality of life. When the patients' needs are not addressed, it can culminate in profound distress compromising their quality of life.
Objectives: This performance indicators study aims to review and assess the impact of inpatient palliative care consultation on code status and patients' length of stay (LOS) for patients with ABC.
Methods: A retrospective quantitative evaluation of data on the total number of ABC patients seen by the palliative care team between 2014 and 2022 at the American University of Beirut Medical Center in Lebanon was done. The average LOS for each patient before and after palliative care consultation was calculated as well as the percentage of patients who chose to de-escalate their care from full code to "Do Not Resuscitate, Do Not Intubate" (DNR/DNI). Data were analyzed using descriptive statistics to identify trends in the data.
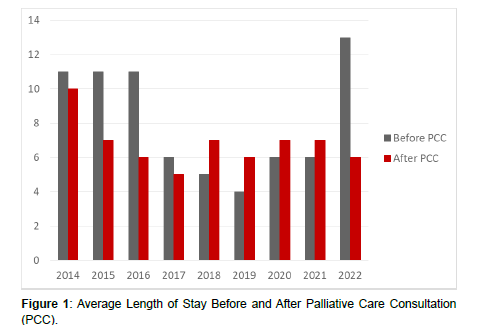
Results: A total of 263 patients were included in the analysis. The average LOS before palliative care consultation was 8.02 days (min: 4 days in 2019; max: 13 days in 2022) compared to 6.85 days post palliative care consultation (min: 5 days in 2017; max: 10 days in 2014) showing a significant reduction in the average LOS post consultation.
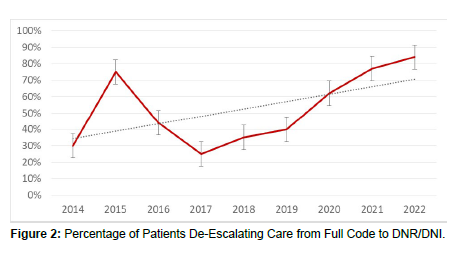
When it comes to code status and serious illness conversation, 30% of patients with ABC chose to change their care status from full code to DNR/DNI in 2014 compared to 84% of patients in 2022.
Conclusion: ABC illness imposes immense hardships on all stakeholders, encompassing patients and healthcare professionals, especially when the needs of these patients are left unhinged. A palliative care consultation for patients with ABC has demonstrated significant benefits. The findings of this study indicate a notable reduction in the average LOS post-consultation and a substantial decrease in aggressive and futile care at end of life, shedding light on the positive impact of palliative care team involvement. These results underscore the dire need to incorporate palliative care into primary care for all patients with advanced breast cancer.
Keywords
Palliative Care in Oncology; Advanced Breast Cancer Management; Patient Quality of Life; Hospital Length of Stay; Code Status Decisions; Retrospective Quantitative Evaluation; Patient-Centered Care; Healthcare Utilization; Palliative Care Consultation Impact
Introduction
Palliative care, with its holistic, patient-centered approach, has become increasingly recognized as an essential component of comprehensive cancer care. This multidisciplinary service aims to improve the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification, impeccable assessment, and the treatment of pain and other problems, physical, psychosocial, and spiritual [1]. The importance of integrating palliative care into the treatment plans for patients with advanced breast cancer cannot be overstated, given the complex challenges this population faces.
Advanced Breast Cancer (ABC) represents a particularly distressing phase of the disease, where curative treatments are no longer effective, and the focus shifts towards extending the quality and duration of life [2]. Patients with ABC often endure significant physical symptoms, including pain, fatigue, and the side effects of ongoing treatment, as well as profound emotional, social, and spiritual distress. These multifaceted challenges highlight the need for a comprehensive approach to care that addresses these diverse needs.
Despite the proven benefits of palliative care in enhancing patient outcomes and quality of life, the integration of these services into the care continuum for patients with ABC remains inconsistent [3,4]. Barriers to integration include a lack of awareness among healthcare providers and patients about the benefits of palliative care, misconceptions that it is synonymous with end-of-life care, and systemic issues within healthcare systems that limit access to these services.
Recent guidelines from leading oncology and palliative care organizations advocate for the early introduction of palliative care into the treatment plan for patients with advanced cancer [4]. These guidelines are based on a growing body of evidence suggesting that early palliative care consultation can lead to better symptom management, improved patient, and caregiver satisfaction, and even extended survival in some cases [4,5].
The current study aims to explore the impact of inpatient palliative care consultation on specific outcomes for patients with ABC, including the length of stay in the hospital and changes in code status, from full code to “Do Not Resuscitate, Do Not Intubate” (DNR/DNI). By focusing on these outcomes, the study seeks to provide insights into the tangible benefits of palliative care for this patient population and to contribute to the ongoing dialogue about how best to integrate palliative care into the comprehensive management of advanced breast cancer.
Overall, the necessity of palliative care in the treatment of advanced breast cancer is clear, given its potential benefit to address the complex needs of this patient population holistically. This study endeavors to add to the evidence base supporting the integration of palliative care, with the goal of improving outcomes and quality of life for patients with ABC.
Literature Review
The Evolution and Definition of Palliative Care
Palliative care has undergone significant evolution since its inception, growing from a service primarily associated with end-oflife care to a comprehensive, multidisciplinary approach that aims to improve the quality of life for patients and their families facing the challenges of serious illness. The World Health Organization (WHO) defines palliative care as an approach that enhances the quality of life of patients and their families facing life-threatening illness, through the prevention and relief of suffering by means of early identification, assessment, and treatment of pain and other problems, physical, psychosocial, and spiritual. This definition underscores the holistic nature of palliative care, extending beyond mere symptom management to address the full spectrum of needs experienced by patients [6].
Palliative Care in Oncology: A Paradigm Shift
In the realm of oncology, the integration of palliative care has marked a paradigm shift towards a more patient-centered model of care. Seminal studies in the early 21st century began to highlight the benefits of early palliative care involvement for cancer patients, challenging the traditional trajectory of introducing palliative care only at the end stages of disease. For instance, Temel et al. demonstrated that patients with metastatic non-small-cell lung cancer who received early palliative care experienced significant improvements in both quality of life and mood compared to those receiving standard care. Furthermore, this early intervention was associated with extended survival, challenging misconceptions that palliative care is synonymous with giving up on active treatment [7,8].
Palliative Care for Advanced Breast Cancer
Focusing on ABC, the need for palliative care becomes particularly acute. ABC represents a stage where the disease is no longer curable, and treatment goals pivot towards extending life and alleviating symptoms. The complexity of managing ABC – encompassing aggressive treatment regimens, symptom burden, and the emotional toll of facing a terminal diagnosis – highlights the indispensability of palliative care in this context. Studies have consistently shown that palliative care, when integrated with standard oncologic treatment, leads to better management of symptoms, reduced psychological distress, and improved decision-making about end-of-life care [3,9,10].
The Impact of Palliative Care on Quality of Life and Healthcare Utilization
The literature consistently supports the notion that palliative care interventions improve the quality of life for patients with advanced cancer, including ABC. A systematic review by Zimmermann et al. synthesized evidence from multiple studies, finding that palliative care led to significant improvements in patient-reported outcomes related to quality of life, symptom intensity, and mood. Beyond patientcentered outcomes, palliative care has also been shown to influence healthcare utilization patterns. By facilitating advanced care planning and aligning treatment decisions with patient preferences, palliative care can lead to a more judicious use of healthcare resources, often resulting in reduced hospital stays and less aggressive care at the end of life [11-14].
Barriers to Integrating Palliative Care
Despite the recognized benefits, barriers to the timely integration of palliative care in oncology persist. These include healthcare professional misconceptions about palliative care equating to end-oflife care, lack of training in palliative care principles among oncologists, and systemic issues such as insufficient palliative care resources and referral pathways. The lack of financial reimbursement remains one of the main barriers in Lebanon. Overcoming these barriers is crucial for ensuring that patients with ABC receive the full spectrum of care they need and deserve [15].
The Role of Palliative Care in Advanced Care Planning and End-of-Life Decision Making
One of the critical roles of palliative care in the context of ABC is facilitating advanced care planning and end-of-life decisionmaking. This process involves discussions about patient preferences for life-sustaining treatments, including resuscitation and mechanical ventilation, in the context of what is medically appropriate and aligned with the patient’s values and goals. Research indicates that palliative care consultations increase the frequency and quality of these conversations, leading to more patients choosing care options focused on comfort and quality of life, such as Do Not Resuscitate (DNR) and Do Not Intubate (DNI) orders [16,17].
Methodology
Study Design
This research employs a retrospective quantitative study approach to evaluate the impact of inpatient palliative care consultation on patients with advanced breast cancer. The study focuses on examining changes in code status and LOS before and after palliative care consultation.
Setting and Patients
The study was conducted at the American University of Beirut Medical Center (AUBMC) in Lebanon, within the Palliative and Supportive Care Program. A total of 263 patients admitted to AUBMC and seen by the palliative care team from 2014-2022 were included. The patient cohort comprised individuals hospitalized for various reasons, including but not limited to, pain management and end-oflife care, specifically targeting those with advanced breast cancer. The inclusion of a wide range of hospitalization reasons was instrumental in understanding the broad impact of palliative care services on this patient population.
Data Collection
Data was meticulously collected from the palliative care program records. A de-identification process was employed to ensure patient confidentiality, removing identifiers such as names, medical record numbers (MRN), and dates of admission. What remained were key variables that are central to our investigation: reasons for hospitalization, LOS before and after receiving in-patient care consultation, and patients’ code status before and after such consultations.
Data Analysis
Descriptive statistics were calculated utilizing Microsoft Excel as our primary tool. This choice was driven by Excel's wide accessibility and its robust functionality for calculating means and identifying trends in data. Through this analysis, we aimed to capture a comprehensive picture of how palliative care consultations influenced the length of stay in the hospital and decisions regarding code status, moving from full code to "Do Not Resuscitate, Do Not Intubate" (DNR/DNI) options. The analysis focused on calculating the mean LOS for patients before and after palliative care consultation, and code status changes pre- and post- consultation. By calculating the average LOS before and after palliative care consultation, we were able to assess whether the involvement of palliative care could be associated with changes in hospital stay duration. Similarly, evaluating the percentage of patients who altered their code status from full code to DNR/DNI before and after consultation provided insights into the patients' decision-making processes and their preferences for end-of-life care.
Ethical Consideration
The methodology was designed with a strong emphasis on ethical considerations, particularly the confidentiality and privacy of patient information. The de-identification process prior to analysis ensured that patient data was handled with the utmost respect and care, aligning with ethical standards in medical research.
Results
Length of Stay (LOS)
The average LOS before palliative care consultation was 8.02 days, which significantly reduced to 6.85 days post-consultation. The trend observed over the years suggests a consistent reduction in LOS following palliative care intervention, indicating enhanced efficiency in patient care and hospital resource utilization (Figure 1).
Code Status Change
A substantial increase in the proportion of patients opting for DNR/ DNI status was observed, rising from 30% in 2014 to 84% in 2022. This trend underscores a growing preference for care de-escalation and a focus on quality of life among ABC patients (Figure 2).
Discussion
Our retrospective review of palliative care’s impact on ABC patients reveals two primary outcomes: a significant reduction in hospital LOS post-palliative care consultation and a marked increase in the proportion of patients opting for DNR/DNI status. These findings, illustrated in our accompanying graphs, underscore the tangible benefits of palliative care integration into ABC management.
The observed decrease in LOS from an average of 8.02 days before palliative care consultation to 6.85 days afterward highlights the effectiveness of palliative care in addressing the complex needs of ABC patients more efficiently, facilitating earlier transitions to outpatient care settings. This reduction not only reflects improved patient management but also has broader implications for healthcare resource utilization, potentially alleviating the burden on hospital services and reducing healthcare costs. Moreover, the increase in patients shifting to DNR/DNI status, from 30% in 2014 to 84% in 2022, suggests a significant change in patient preferences towards end-of-life care. This shift likely reflects the success of palliative care consultations in fostering more informed decision-making by providing patients and their families with a clear understanding of the prognosis and treatment options. Such discussions empower patients to make choices that align with their values and preferences, emphasizing quality of life.
Reduction in Length of Stay
The observed reduction in LOS post-palliative care consultation aligns with emerging evidence that palliative care interventions can streamline patient management, leading to more efficient use of hospital resources [18]. This efficiency likely stems from the comprehensive assessment and management of symptoms, both physical and psychosocial, that palliative care teams offer. By addressing these issues proactively, palliative care can prevent complications and reduce the need for acute care services, facilitating earlier discharge from the hospital [19].
Furthermore, the reduction in LOS has implications beyond the immediate benefits to patients and healthcare systems. It may reflect a broader shift in care goals towards prioritizing quality of life and patient-centered decision-making. As palliative care teams work closely with patients and families to clarify goals of care and align treatment decisions with these goals, unnecessary interventions that do not contribute to patient well-being can be minimized [11,12,20].
Shift in Code Status Preferences
The significant increase in patients opting for DNR/DNI status post-palliative care consultation is a critical finding of our study. This trend suggests that palliative care consultations play a vital role in facilitating serious illness conversations, where patients are encouraged to reflect on their values and preferences for end-of-life care [16]. Such discussions are essential for ensuring that care plans are in alignment with patients’ wishes, ultimately leading to more patient-centered care. This shift also indicates a growing recognition among ABC patients of the importance of focusing on the quality rather than the quantity of life in the advanced stages of illness. By choosing DNR/DNI status, patients often seek to avoid aggressive interventions that may not significantly improve their prognosis while potentially detracting from their quality of life [17,21].
Comparison with Existing Literature
Our findings contribute to a growing body of literature that underscores the value of early palliative care integration for patients with advanced cancers. Studies have consistently shown that palliative care can improve a range of outcomes, from symptom management and emotional support to patient and family satisfaction and even survival in certain cases [7,13]. Our study builds on this evidence, specifically highlighting the impact of palliative care on hospital LOS and end-of-life care preferences in the ABC patient population.
Study Limitations and Future Research
While our study provides valuable insights, it is not without limitations. The retrospective design and single-center setting may limit the generalizability of our findings. Additionally, the use of descriptive statistics, while informative, does not allow for causal inferences. Future research should employ prospective, multicenter designs to validate and expand upon our findings, exploring the mechanisms through which palliative care achieves its benefits.
Moreover, future studies should examine the role of patientreported outcome measures in assessing the impact of palliative care. These measures can provide critical insights into the patient’s experience, offering a more nuanced understanding of how palliative care interventions affect quality of life, symptom burden, and psychological well-being [22].
Conclusion
The results of our study affirm the critical role of palliative care in the management of advanced breast cancer, demonstrating significant benefits in terms of both patient-centered outcomes and healthcare resource utilization. By facilitating a shift towards care that aligns with patient preferences and enhancing the efficiency of hospital resource use, palliative care consultations represent a key component of comprehensive cancer care. These findings underscore the need for healthcare policies and practices that support the integration of palliative care into the standard care pathway for patients with advanced breast cancer, ensuring that all patients have access to care that prioritizes their quality of life and respects their values and preferences.
References
- Rome RB, Luminais HH, Bourgeois DA, Blais CM (2011) the role of palliative care at the end of life. Ochsner Journal 11: 348-352.
- Fallowfield L, Boyle FM, Travado L, Kiely BE, Jewell P, et al. (2021) Gaps in Care and Support for Patients with Advanced Breast Cancer: A Report from the Advanced Breast Cancer Global Alliance. JCO Glob Oncol 7: 976-984.
- Oliver D (2018) Improving patient outcomes through palliative care integration in other specialised health services: What we have learned so far and how can we improve? Ann Palliat Med 7: S219-S230.
- Hui D, Hannon BL, Zimmermann C, Bruera E (2018) Improving patient and caregiver outcomes in oncology: Team-based, timely, and targeted palliative care. CA: A Cancer J Clinic 68: 356-376.
- Mason H, Derubeis MB, Hesseltine B (2021) Early Palliative Care for Oncology Patients: How APRNs Can Take the Lead. JADPRO12: 477-484.
- https://www.who.int/news-room/fact-sheets/detail/palliative-care
- Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, et al. (2010) Early palliative care for patients with metastatic non-small-cell lung cancer. The New England J Med 363: 733-742.
- Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, et al. (2009) Effects of a Palliative Care Intervention on Clinical Outcomes in Patients With Advanced Cancer: The Project ENABLE II Randomized Controlled Trial. JAMA 302: 741-749.
- Smith TJ, Temin S, Alesi ER, Abernethy AP, Balboni TA, et al. (2012) American Society of Clinical Oncology provisional clinical opinion: The integration of palliative care into standard oncology care. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology 30: 880-887.
- Greer JA, Jackson VA, Meier DE, Temel JS (2013) Early integration of palliative care services with standard oncology care for patients with advanced cancer. CA: Cancer J Clinicians 63: 349-363.
- Zaborowski N, Scheu A, Glowacki N, Lindell M, Battle-Miller K (2022) Early Palliative Care Consults Reduce Patients’ Length of Stay and Overall Hospital Costs. The American J Hospice Palliat Care 39: 1268-1273.
- Srinivasan VJ, Akhtar S, Huppertz JW, Sidhu M, Coates A, et al. (2023) Prospective Cohort Study on the Impact of Early Versus Late Inpatient Palliative Care on Length of Stay and Cost of Care. The American J Hospice & Palliat Care 40: 704-710.
- Zimmermann C, Swami N, Krzyzanowska M, Hannon B, Leighl N, Oza A, et al. (2014) Early palliative care for patients with advanced cancer: A cluster-randomised controlled trial. The Lancet 383: 1721-1730.
- May P, Hynes G, McCallion P, Payne S, Larkin P, et al. (2014) Policy analysis: Palliative care in Ireland. Health Policy (Amsterdam, Netherlands) 115: 68-74.
- Parikh RB, Kirch RA, Smith TJ, JS Temel JS (2013) Early specialty palliative care—Translating data in oncology into practice. The New England J Med 369: 2347-2351.
- Wright AA, Zhang B, Ray A, Mack JW, Trice E, et al. (2008) Associations Between End-of-Life Discussions, Patient Mental Health, Medical Care Near Death, and Caregiver Bereavement Adjustment. JAMA 300: 1665-1673.
- Bernacki RE, SD Block for the American College of Physicians High Value Care Task Force (2014) Communication about Serious Illness Care Goals: A Review and Synthesis of Best Practices. JAMA Int Med 174: 1994-2003.
- Smith GM, Calton BA, Rabow MW, Marks AK, Bischoff, et al. (2021) Comparing the Palliative Care Needs of Patients Seen by Specialty Palliative Care Teams at Home Versus in Clinic. J Pain Symptom Manag 62: 28-38.
- Gómez-Batiste X, Amblàs Novellas J, Costa X, lasmarías C, Santaeugènia Gonzàlez S, et al. (2019) Development of Palliative Care: Past, Present, and Future 77-88.
- Meier DE (2018) Palliative care and the diffusion of innovation. J Palliat Med 21: 736-739.
- Kuosmanen L, Hupli M, Ahtiluoto S, Haavisto E (2021) Patient participation in shared decision-making in palliative care-An integrative review. J Clin Nur 30: 3415-3428.
- Kaasa S, Loge JH, Aapro M, Albreht T, Anderson R, et al. (2018) Integration of oncology and palliative care: A Lancet Oncology Commission. The Lancet Oncol 19: e588-e653.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Yamout R (2024) Impact of In-Patient Palliative Care Consultation onPatient Outcomes in Advanced Breast Cancer - A Retrospective Review. J PalliatCare Med 14: 622.
Copyright: © 2024 Yamout R. This is an open-access article distributed under theterms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Usage
- Total views: 695
- [From(publication date): 0-2024 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 506
- PDF downloads: 189