Impact of Acupuncture on Fatigue Management in Individuals with Parkinson's Disease
Received: 28-Jun-2023 / Manuscript No. JADP-23-104196 / Editor assigned: 30-Jun-2023 / PreQC No. JADP-23-104196 (PQ) / Reviewed: 14-Jul-2023 / QC No. JADP-23-104196 / Revised: 21-Jul-2023 / Manuscript No. JADP-23-104196 (R) / Published Date: 28-Jul-2023 DOI: 10.4172/2161-0460.1000574
Abstract
Parkinson’s Disease (PD) is the second most common neurodegenerative disease in the United States, effecting approximately a million Americans every year. Though the disease is not fatal, it puts patients at risk for other causes of morbidity and mortality (example: falls, aspiration, serious infections). Along with classic psychiatric and motor symptoms reported by Parkinson’s patients, fatigue is a common and disabling problem. Medical treatment for fatigue in PD is typically managed non-medically through lifestyle modifications (example: sleep hygiene, daytime naps, exercise) though medications may also be used (example: antidepressants, stimulants). Medications may come with side effects; at this point there is no satisfactory treatment specifically targeted at fatigue in PD.
Keywords: Parkinson’s disease; Acupuncture; Fatigue; Electroacupuncture; Traditional chinese medicine
Introduction
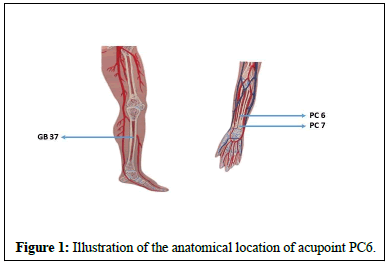
Parkinson’s disease is the second most common neurodegenerative disease in the United States, with an estimated 500,000 new diagnoses every year-though some argue PD is underdiagnosed [1]. PD is caused by the loss of the dopaminergic neurons in the substantia nigra, leading to PD’s widely known movement symptoms (for example resting tremor, stiffness, bradykinesia, posture and gait changes, and poor coordination). Movement symptoms however can be accompanied by a wide range of other issues including psychiatric symptoms, sympathetic dysregulation, fatigue, and disordered sleep. The causes of PD are not well understood. Rare genetic mutations of alpha-synuclein (a normal protein, an accumulation of which is seen in PD) do exist in most PD patients who do not have such mutations [1]. PD presents a significant burden not only to patients and family members but on American society writ large (Figure 1).
Anecdotally some PD patients report benefits from acupuncture as an adjunct to traditional medical management. Acupuncture is a form of medicine practiced in China for more than 3,000 years [2]. Different acupuncture traditions evolved across East Asian countries before eventually spreading to Europe and America in the sixteenth to nineteenth centuries [3]. Formal interest in acupuncture died down in nineteenth-century Britain and America, Sir William Osler described dramatic success in the treatment of back pain with hat pins in one of his textbooks [2]. While practitioners and patients espouse the benefits of acupuncture, research into acupuncture as a medical treatment is limited, especially in the United States. Many theories have been offered for acupuncture’s proposed health benefits, but the exact mechanism is not yet known.
To this day acupuncture remains controversial. This study aims to perform a systematic review of the existing scientific literature on the effectiveness of acupuncture as a treatment for fatigue in PD based on Randomized Controlled Trials (RCTs).
Materials and Methods
A systematic literature search was conducted from 23 May until 20 June 2023, following the PRISMA guidelines in the following databases: EMBASE, Medline, Pubmed, Science Direct, The Cochrane Library, Cochrane Central Register of Controlled Trials (Central), and Scielo. Search terms used were PD and acupuncture. This yielded 442 papers published in English between 1974 and 2023. Narrowing search parameters to clinical trial and randomized control trial articles brought the total number of publications to 34, which were manually reviewed for relevance. Trials must have included fatigue as an outcome measure and must specifically have been discussed in the conclusions and/or discussion section. Patients diagnosed with idiopathic PD were considered without restrictions based on age, race, gender, or disease duration/severity. Experimental studies with animal models and in vitro studies were also excluded. Three studies (all RCTs) were ultimately identified as meeting inclusion criteria.
Interventions
Different types of acupuncture were used among the three studies. Two studies considered fatigue as their primary outcome measure: One study (Kong, et al) compared sham (non-penetrative) acupuncture (control group) to true (penetrative) acupuncture using a set 11-point treatment based on traditional Chinese medicine (TCM) principles (treatment group), described as the following: It includes For patients in the real acupuncture group, acupoints were needled to a depth of 0.5 to 1 inch, depending on patient's size and sensitivity in the following order: right PC 6, left PC 6, right Large Intestine 4 (LI 4), left LI 4, right ST 36, left Stomach 36 (ST 36), right Spleen 6 (SP 6), left SP 6, right Kidney Meridian 3 (KI 3), left KI 3, and Conception Vessel 6 (CV 6). Thus, a total of 11 acupoints were needled at each session. No flicking or rotation of needles was allowed after insertion. The needles were retained in position for 20 minutes after which they were removed. Each session was based on a strict protocol, and conversation between acupuncturists and patients was kept to a minimum [4].
The second study Klugler, et al. considered sham acupuncture compared to penetrative acupuncture but provided no detail on the acupuncture points used [5]. In the final study (Nazarova, et al.) traditional medical treatment (control group) was compared to traditional medical treatment plus scalp and abdominal electroacupuncture (treatment group). Primary outcomes were changes in the score of clinical scales including the Non-motor Symptom Rating Scale (NMSS), PD Sleep Scale (PDSS), Bristol Stool Function Scale (BSFS), and Patient Associated Constipation and Quality of Life Scale (PAC-QOL). The secondary outcomes were the Unified PD Rating Scale (UPDRS) and Modified Hoehn-Yahr Staging Scale scores. Fatigue/sleep is a subcategory within NMSS, upon which the authors explicitly commented. Neither the specific acupuncture points nor the method of point selection were discussed [6].
Outcome measures
In two studies fatigue was the primary outcome measure, using the General Fatigue score of the Multidimensional Fatigue Inventory (MFI‐GF) and the Modified Fatigue Impact Scale and respectively. In the third study, the primary outcomes included changes in the Non-motor Symptom Rating Scale (NMSS), of which one subcategory is fatigue/sleep. The authors commented on the statistical significance of the change, though exact data were not provided.
Participants and study design
All three studies included patients with a known diagnosis of PD, in whom traditional medical management (for example: Medications) was continued for the duration of the study. In Kong, et al, forty PD patients with moderate fatigue were randomized into real and sham acupuncture treatment, biweekly for five weeks. The exclusion criteria for this study were: significant cognitive, language or psychiatric illnesses which prevent the subject from understanding instructions and participating in the study, needle phobia, comorbidity with a bleeding disorder, known anemia with hemoglobin level <10 g/dL, known congestive cardiac failure and/or end‐stage renal disease, female subjects of childbearing age, and presence of symptomatic postural hypotension. In Kluger, et al, ninety-four participants with moderate-to-high fatigue associated with PD were randomized into treatment acupuncture (penetrative) and control (sham, non-penetrative acupuncture) groups, which they received biweekly for six weeks. In Nazarova, et al, thirty patients with mild to moderate PD were randomized into treatment (scalp and abdominal electroacupuncture) and control (continuation of conventional drug treatment, no placebo) groups. The intervention group received electroacupuncture twice a week for 30 min. As per the study, inclusion and exclusion criteria were as follows: 1) diagnosed idiopathic PD according to the UK PD Society Brain Bank criteria; 2) modified Hoehn-Yahr scale is 1–3 grades; 3) willingness to participate. The exclusion criteria were as follows: 1) suspected or diagnosed with secondary Parkinsonism; 2) suspected or diagnosed with atypical Parkinson’s syndrome; 3) previous history of moderate to severe traumatic brain injury, hydrocephalus, or brain surgery; 4) severe surgical disease or history of malignancy; 5) inability to cooperate; 6) received acupuncture or electroacupuncture therapy in the last 6 months; and 7) unsuitable for acupuncture procedure. The primary outcomes were changes in the score of clinical scales including the Non-motor Symptom Rating Scale (NMSS), PD Sleep Scale (PDSS), Bristol Stool Function Scale (BSFS), and Patient Associated Constipation and Quality of Life Scale (PAC-QOL). The secondary outcomes were the Unified PD Rating Scale (UPDRS) and Modified Hoehn-Yahr Staging Scale scores. Fatigue and sleep were remarked on as a subcategory of the NMSS [6,7].
Results and Discussion
The two studies involving a sham acupuncture treatment, both the control and treatment groups showed an improvement in symptoms though without a statistically significant difference between groups. In the scalp-abdominal electroacupuncture study, in which conventional treatment was compared to convention medical treatment with adjunctive electroacupuncture patients showed improvements in NMSS, PDSS, and UPDRS scores in patients, particularly in the subdomain of fatigue/sleep. The three studies included in this review were published between 2016 and 2022. While a broad search was conducted the pool of research on acupuncture as a potential treatment for fatigue in PD is quite small, though relatively recent.
All three studies reported an improvement in self-reported fatigue symptoms, however in the two studies with sham acupuncture treatments no statistically significant difference was found in the improvement between the intervention and control groups. This may indicate some of the improvement seen in patients could be attributed to other aspects of participation in a research study (social interaction, sense of purpose, and hands-on care/practitioner’s caring touch), as opposed to the acupuncture itself. In the study with a well-described list of treatment points, it is unclear whether the same points were used in the sham acupuncture group as well.
In the electroacupuncture study, patients showed an improvement in symptoms with electroacupuncture treatment and a statistically significant improvement in fatigue/sleep related domain of the NMSS as compared to the control group. However, the control group did not receive a sham treatment making the improvements more difficult to parse. All three studies were small, n ranging from 30 to 90. Two of the studies described the acupuncture treatments as ‘biweekly’, without explicitly stating if the patients were treated twice a week or every other week. While one study did exclude potential participants with anemia (hemoglobin levels <10) no other lab test were performed to rule out other potential contributors to fatigue (vitamin D deficiency, etc) nor was the seasonal timing of the beginning/end of any of the studies discussed.
None of the studies followed up with patients after the course of the treatment to track the course of the symptoms. Only one study that provided a list of treatment points (and logic for the treatment point selection). While standardized treatment points have a value and are more easily replicated, future studies should consider including treatment groups where patients’ symptoms are assessed and treated based on the discretion of an experienced practitioner (not limited to a list of set points). While more difficult to implement this is an oft given criticism of clinical studies of acupuncture.
Conclusion
Few studies exist on the role of acupuncture in the treatment of fatigue in PD. The studies that do exist are small and not all include sham treatment groups, making it difficult to draw conclusions. Existing studies do not always provide detailed information on treatment protocols, making them difficult to replicate. Future studies should include both sham acupuncture and traditional medical treatment control groups to better elucidate the impacts of true acupuncture. Where possible, studies on acupuncture should also consider comparing standardized treatments with treatment plans created and implemented by an experienced practitioner. Larger trials may also consider blocking by disease severity.
References
- National Institute of Neurological Disorders, Stroke (US) (2023). Parkinson's disease: Challenges, progress, and promise. NINDS.
- Jishun J, Mittelman M (2014). Acupuncture: past, present, and future. Glob Adv Health Med. 3(4):6-8.
[Crossref] [Google Scholar] [PubMed]
- Lu DP, Lu GP (2013). An historical review and perspective on the impact of acupuncture on US medicine and society. Med Acupunct 25(5):311-316.
[Crossref] [Google Scholar] [PubMed]
- Kong KH, Ng HL, Li W, Ng DW, Tan SI, et al. (2018). Acupuncture in the treatment of fatigue in Parkinson's disease: a pilot, randomized, controlled, study. Brain Behav 8(1):e00897-e00897.
[Crossref] [Google Scholar] [PubMed]
- Kluger BM, Rakowski D, Christian M, Cedar D, Wong B, et al. (2016). Randomized, controlled trial of acupuncture for fatigue in Parkinson's Disease. Mov Disord 31(7):1027-1032.
[Crossref] [Google Scholar] [PubMed]
- Nazarova L, Liu H, Xie H, Wang L, Ding H, et al. (2022). Targeting gut-brain axis through scalp-abdominal electroacupuncture in Parkinson’s disease. Brain Res 1790:147956-147956.
[Crossref] [Google Scholar] [PubMed]
- Kong KH, Ng HL, Li W, Ng DW, Tan SI, Tay KY, et al. Acupuncture in the treatment of fatigue in Parkinson's disease: a pilot, randomized, controlled, study. Brain Behav. 2018;8(1):e00897.
[Crossref] [Google Scholar] [PubMed]
Citation: Stockton-Brown M (2023) Impact of Acupuncture on Fatigue Management in Individuals with Parkinson's Disease. J Alzheimers Dis Parkinsonism 13:574. DOI: 10.4172/2161-0460.1000574
Copyright: © 2023 Stockton-Brown M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1526
- [From(publication date): 0-2023 - Sep 29, 2025]
- Breakdown by view type
- HTML page views: 1224
- PDF downloads: 302