Imaging of Pediatric Extra-Cranial Tumor
Received: 05-Sep-2022 / Manuscript No. roa-22-76104 / Editor assigned: 07-Sep-2022 / PreQC No. roa-22-76104 (PQ) / Reviewed: 21-Sep-2022 / QC No. roa-22-76104 / Revised: 23-Sep-2022 / Manuscript No. roa-22-76104 (R) / Published Date: 30-Sep-2022
Image Article
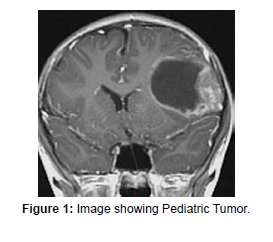
Dynamic contrast-enhanced magnetic resonance imaging (DCEMR) is turning into a generally acknowledged reciprocal method for diagnosing cancers in adults [1]. This procedure is also helpful to predict tumor response to anticancer treatment and screen the tumor response to the treatment [2]. Past investigations utilizing DCE-MR exhibited that malignant tumors typically showed quicker and higher levels of improvement than ordinary tissue. This enhancement characteristic showed that threatening malignant tumors expanded vascularity and endothelial porousness to the contrast molecules than that of typical or less aggressive malignant tissues [3]. In many tumors, the estimations of micro vascular thickness made on histopathological tests associated intimately with various clinical stages. The relationship could be because of the rapid tumor growth which must be upheld by profoundly dynamic angiogenesis. The more forceful growths were subsequently connected with higher angiogenesis-related microvasculature irregularities (Figure 1).
Based on this histopathological proof it had been recommended that DCE-MR could possibly provide additional independent indices of angiogenic movement and could hence go about as a prognostic pointer in an expansive scope of tumor types. DCE-MR time intensity curve designs are sorted into three types: Type 1, persistently upgrading (moderate), which recommends less angiogenic; Type 2, plateau type, which has a middle probability for malignancy; and type 3, washout type, which is characteristic of malignancy with a lot of angiogenesis. Our past concentrate on the use of DCE-MR in a wide scope of pediatric extra-cranial tumors showed comparative outcomes as in grown-ups. Type 1 bend with maximal improvement intensity (SImax) less than 350 might be an extra pointer for h benign or inactive tumors. The degree of growth putrefaction was connected intimately with pathology discoveries in follow-up cases. The absence of irradiation has an upper hand over CT or PET in pediatric applications.
References
- Bhujwalla ZM, Artemov D, Glockner J (1999) Tumor angiogenesis, vascularization, and contrast-enhanced magnetic resonance imaging. Top Magn Reson Imaging 10: 92-103.
- Padhani AR (1999) Dynamic contrast-enhanced MRI studies in human tumours. Br J Radio 72: 427-431.
- Weidner N (1996) Intratumoural vascularity as a prognostic factor in cancers of the urogenital tract. Eur J Cancer 32A: 2506-2512.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Joel J (2022) Imaging of Pediatric Extra-Cranial Tumor. OMICS J Radiol 11: 404.
Copyright: © 2022 Joel J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 1559
- [From(publication date): 0-2022 - Mar 29, 2025]
- Breakdown by view type
- HTML page views: 1236
- PDF downloads: 323