Imaging in Therapeutic Radiology
Received: 28-Feb-2023 / Manuscript No. roa-23-92471 / Editor assigned: 02-Mar-2023 / PreQC No. roa-23-92471 (PQ) / Reviewed: 16-Mar-2023 / QC No. roa-23-92471 / Revised: 20-Mar-2023 / Manuscript No. roa-23-92471 (R) / Published Date: 27-Mar-2023 DOI: 10.4172/2167-7964.1000433
Image Article
Radiation therapy, also known as radiotherapy or RT, RTx, or XRT, is a treatment that uses ionizing radiation to control or kill cancer cells and is typically administered by a linear accelerator. Radiation treatment might be healing in various sorts of malignant growth assuming they are restricted to one region of the body. After surgery to remove a primary malignant tumor (such as the early stages of breast cancer), it may also be used as part of adjuvant therapy to prevent tumor recurrence. In cancers that are susceptible, radiation therapy has been utilized prior to during and after chemotherapy due to its synergistic effect with chemotherapy. Radiation oncology is the name given to the subspecialty of oncology that focuses on radiotherapy. A radiation oncologist is a doctor who practices in this subspecialty [1].
Because it can control cell growth, radiation therapy is often used to treat cancerous tumors. If the draining lymph nodes are thought to be at risk of subclinical malignant spread or are clinically or radiologically associated with the tumor, the radiation fields may also include the tumor itself. It is important to incorporate an edge of typical tissue around the cancer to consider vulnerabilities in day to day set-up and inward growth movement. Internal movement, such as breathing and emptying the bladder, and movement of external skin marks in relation to the tumor position can both contribute to these ambiguities [2].
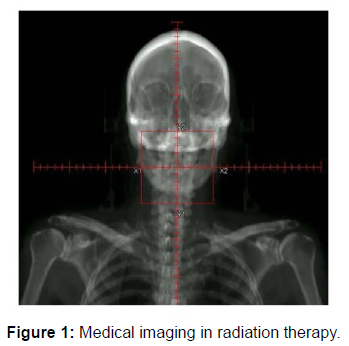
In contrast to radiology, which uses radiation in medical imaging and diagnosis, radiation oncology is the medical specialty that focuses on prescribing radiation. A radiation oncologist may prescribe radiation with the intention of curing (curative) or as adjuvant therapy. It can also be used as a palliative treatment (when a cure is not possible and the goal is local disease control or symptom relief) or as a therapeutic treatment (when the treatment has a survival benefit and can be curative). It is also common to combine radiation therapy with surgery, chemotherapy, hormone therapy, immunotherapy or a combination of the four. Radiation therapy can be used in some way to treat the majority of common cancers (Figure 1).
Acknowledgement
None
Conflict of Interest
None
References
- Rades D, Stalpers LJ, Veninga T, Schulte R, Hoskin PJ, et al. (2005) Evaluation of five radiation schedules and prognostic factors for metastatic spinal cord compression. J Clin Oncol 23: 3366-3375.
- Maverakis E, Cornelius LA, Bowen GM, Phan T, Patel FB, et al. (2015) Metastatic melanoma - a review of current and future treatment options. Acta Derm Venereol 95: 516-524.
Indexed at, Google Scholar, Crossref
Citation: Gupta S (2023) Imaging in Therapeutic Radiology. OMICS J Radiol 12: 433. DOI: 10.4172/2167-7964.1000433
Copyright: © 2023 Gupta S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 1482
- [From(publication date): 0-2023 - Dec 05, 2025]
- Breakdown by view type
- HTML page views: 1156
- PDF downloads: 326