Imaging and Radiation Therapy for Meningioma
Received: 02-May-2022 / Manuscript No. roa-22-64827 / Editor assigned: 04-May-2022 / PreQC No. roa-22-64827 (PQ) / Reviewed: 18-May-2022 / QC No. roa-22-64827 / Revised: 20-May-2022 / Manuscript No. roa-22-64827 (R) / Published Date: 27-May-2022 DOI: 10.4172/2167-7964.1000382
Image Article
Radiation therapy can be an essential therapy for meningioma, or it tends to be directed after a medical procedure to destroy any abnormal cells that remain. During radiation therapy, high-energy beams are aimed at a tumor to damage the DNA inside its abnormal cells. This can assist with preventing the tumor cells from separating; it can likewise make existing cells to self-destruct. Tumors frequently shrivel after radiation therapy, which helps reduce pressure on the brain or spinal cord. This in turn can assist with mitigating side effects.
Meningiomas are characterized morphologically by the World Health Organization (WHO) evaluating plan into three categories [1]. While most meningiomas are harmless or grade I the affinity of certain subtypes to repeat following treatment makes a pathological course that can prompt a range of malignant disease.
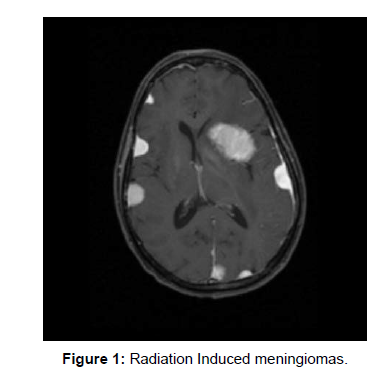
The objective of medical procedure is to securely resect the tumor and acquire a diagnosis and pathological grade. Ensuing radiation therapy relies upon the degree of resection and pathological qualities. Patients holding on to either WHO grade II or III meningiomas have higher recurrence rates differing between 29-52 and 50-94% respectively [2]. This might be expected partially to parenchymal invasion or the aggressiveness of residual tumor cells. Higher recurrence rates correlate with decreased overall survival (Figure 1).
Diagnosis
A Meningioma can be difficult to diagnose in light of the fact that the tumor is often slow growing. Side effects of a meningioma may likewise be unobtrusive and mistaken with other medical issue or written off as ordinary indications of aging.
If your provider suspects a meningioma, you might be alluded to a doctor who specializes in neurological conditions (neurologist).
References
- Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, et al. (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114: 97-109.
- Aghi MK, Carter BS, Cosgrove GR, Ojemann RG, Amin-Hanjani S, et al. (2009) Long-term recurrence rates of atypical meningiomas after gross total resection with or without postoperative adjuvant radiation. Neurosurgery 64: 56-60.
Indexed at, Google Scholar, Crossref
Citation: Patel P (2022) Imaging and Radiation Therapy for Meningioma. OMICS J Radiol 11: 382. DOI: 10.4172/2167-7964.1000382
Copyright: © 2022 Patel P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 1207
- [From(publication date): 0-2022 - Mar 29, 2025]
- Breakdown by view type
- HTML page views: 781
- PDF downloads: 426