Identification of the Factors of Utilization Pattern of Post Natal Services by the Mothers and Their Satisfaction Level in a Selected Rural Community, West Bengal
Received: 02-Dec-2022 / Manuscript No. gnfs-22-80156 / Editor assigned: 05-Dec-2022 / PreQC No. gnfs-22-80156(PQ) / Reviewed: 19-Dec-2022 / QC No. gnfs-22-80156 / Revised: 24-Dec-2022 / Manuscript No. gnfs-22-80156 (R) / Published Date: 29-Dec-2022 DOI: 10.4172/2572-0899.1000205
Abstract
A descriptive survey to identify factors of utilization pattern of postnatal services by the mothers and their satisfaction level among 100 mothers having baby of 6 weeks to 6 months of age. The conceptual framework was based on Anderson Model of Health service utilization. Non –probability purposive sampling technique was used. Data were collected through valid and reliable tools which included a semi structure interview schedule, record analysis proforma and a rating scale. The study revealed that majority (86%) of the mothers were not aware about the postnatal services and only (34%) of the participants utilized three postnatal visits. It was also found out that majority of the mothers were satisfied related to physical facilities of the post-natal service except for waiting time where majority of the mothers were partially satisfied. (52%). Regarding health worker’s behavior majority was satisfied, except for maintaining privacy for examination where majority of them were partially satisfied, (65%). Majority of the mothers were satisfied with the quality of post-natal care, except for conveying the findings where majority were partially satisfied (55%). The study further revealed that there is significant association between mother’s education and utilization pattern of post-natal services at 0.05 level of significance as evidenced by x2 = 5.8The study also revealed that there is significant association between husband’s education (x2 =5.1), and per- capita income(x2 =4.5) with immunization on schedule date.
Keywords
Postnatal service; Utilization pattern; Factors; Satisfaction level; Postnatal mothers
Introduction
Post-partum period is recognized as a critical time for both mother and new-borns. Postpartum period is a crucial phase for the women as there are physiological changes along with psychological adaptation for changing role in the family. Many post-partum complications occur during this period. Among these the important obstetric morbidities are post-partum hemorrhage, pulmonary embolism and puerperal sepsis. The common surgical complications are wounds breakdown, breast abscess and urinary fecal incontinence. Medical conditions such as anaemia, headache, backache, sexual problems may also be present. Worldwide everyday at least 1600 women die from complications of pregnancy and child birth, the majority of which takes place in the developing countries [1]. Most deaths of mothers and new-born occur soon after delivery, over 60 percent of maternal death occur within first 48hrs after child birth,(WHO 2005) [2]. All neonatal deaths in 1st month of life are due to non HIV (asphyxia, sepsis, pre maturity), highlighting the need to address the quality of basic maternal and new-born care. Three quarter of new born death occurs, in the first week and of those, two thirds occurs in the first 24 hrs. Inter pregnancy interval of less than 18 months and more than 59 months are significantly associated with increased risk of adverse perinatal outcomes. Throughout the world, many women use the return of their menstrual period as a signal to begin contraception yet the return of menses may indicate that the fertility returned several weeks before, thus leaving up to 10percent of women at risk of becoming pregnant before their menses resume [3]. Post-partum care is the most neglected aspect of maternity care and more research is needed on issues related to postnatal maternal health. Early post-partum care is essential to diagnose and treat complications. Only 1 in 6 women receive care during the postpartum period in India. The National Family Health Survey data indicate that only 17percent of the women delivering at home was followed by a check –up within two months of delivery, and a meager five percent within the first 7 days. Even out of this minor range of women, most of them were not provided with the entire range of information and services that should have been provided to a woman during a postpartum visit [4]. WHO estimates that out of the 529,000 maternal deaths globally each year 136, 000, (25 percent) are contributed by India.(6) It is estimated that between 11-17 percent of maternal death occurs during child birth itself and between 50 to 71 percent in the post-partum period and 45 percent of postpartum maternal death occurs during the first 24hrs and more than two thirds during the first week [5]. On an average, skilled birth attendants cover 66 percent of all births worldwide, and some parts of Africa and Asia have much lower coverage rates. In developed countries virtually all women and their infants receive postpartum and post natal care albeit the nature and frequency of this care. In developing countries the need for care and support after birth was, until recently, less recognized. Despite its importance, this period is generally the most neglected. Rates of provision of skilled care are lower after childbirth than during pregnancy or childbirth, even though both the risks for illness and the potential to improve longerterm outcomes are great [6].
One of the major challenges in our country is to reduce the maternal mortality rate. An alarming scenario of pregnancy related complications claim the lives of an estimated 0.5 million women worldwide and one women every minute. Besides maternal death increases child’s risk of death 3-10 times within the first two years of their life [7].
Current models of postpartum care in developed countries originated in the beginning of the 20th century in response to high maternal and neonatal mortality rates of the time. Research into the current coverage and content of postpartum and postnatal care has been limited. The average range in the number of visits or contacts that women and their infants have with their health- care providers is not well documented. Even in developed countries there has been little evaluation to assess whether the current models of care meet individual women’s and babies’ physical and emotional health needs, and whether they make the most appropriate use of the skills and time of the relevant health care professionals and of financial resources [8-10].
Mother and child are the most vulnerable group and in India they contribute about 32-40 percent of the total population in India, and therefore it is very vital to improve their health and well-being [11].
West Bengal contributes about 4.7 percent of total maternal death in the country. It was found out through studies that in the year 2005- 2006 , the total number of maternal deaths in West Bengal was 4624 and out of them 1808 (39%) were reported, reflecting the under reporting to a great extent [12]. Against this backdrop the Department of Health and Family Welfare, Government of West Bengal in its mission to improve the healthstatus of all the people of West Bengal especially the poorest and those in need, has embarked on several health sector reforms for reducing maternal and child mortality and the burden of communicable, non-communicable diseases, etc. The Health Sector Strategy (HSS) 2004-2013 has been formulated to address these priority health goals, ensuring quality care and improved access [13].
Client satisfaction reflects quality of services. Good client satisfaction studies are not ends in themselves; they are means to improve service to the public. Broadly, the knowledge on the degree of client satisfaction serves two principal purposes: identifying areas of improvement, in the quality of services offered and highlighting the needs for corrective actions [14].
Satisfaction is an important health outcome in today’s cost conscious health care arena. Quality improvement in healthcare organization requires effective measurement of patient satisfaction. The differences in satisfaction mirror the realities of care to a substantial extent and such information can provide dependent measures of services of quality. So as the realization develop the magnitude of the maternal and infant mortality and morbidity and post-partum complications, the investigator attention has been shifted to identification of the factors of the utilization pattern of the postnatal services and their satisfaction level regarding the services [15].
Materials and Methods
This descriptive survey was conducted with the following objectives
• To assess the utilization pattern of postnatal services availed by the mothers in a selected rural area.
• To identify the factors related to the utilization pattern of the service.
• To assess the satisfaction level of the mothers regarding the availed services
• To identify the association of the utilization pattern of services with selected Variables.
Settings
The selection of an appropriate setting is important because the setting can influence the way people behave, feel and how they respond.
Settings of the study - Chaduria 1, Madanpure GP and Rautari sub centre under Chakdaha B.P.H.C, Nadia, West Bengal.
Final study - Chaprah-1 & Doyerbazar Subcentres under Chaprah B.P.H.C, Nadia , West Bengal.
Samples
In the present study 100 mothers having babies of 6 weeks to 6 months of age during the study period were chosen as samples.
Inclusion criteria
• Mothers having babies 6weeks to 6 months of age.
• Mothers who can understand and speak Bengali.
• Mothers who were willing to participate.
Exclusion criteria
• Mother’s having complications (mother /baby)
• Mothers who cannot understand or speak Bengali.
Sampling technique
Non probability purposive sampling technique was adopted to select the participants for the study.
Data collection tools and techniques
• A semi structured interview schedule for back ground information and factors of utilization pattern of mothers was developed.
• A structured record analysis proforma for assessing the coverage of immunization of the babies till 6 weeks of age was used.
• A rating scale for assessing the satisfaction level of the mothers regarding the postnatal service was also developed.
Steps of data collection
• After getting the administrative permission from B.M.O.H, Chaprah BPHC, two sub centers were selected.
• On the first day, formal introduction with the health workers (A.N.M) and Anganwadi workers was done.
• Registers were checked to get the sample and their home address and fulfillment of sampling criteria.
• On the subsequent days the investigator met the mothers collectively at Anganwadi center and out reach camp , with the help of link person.
• Purpose of the study was explained to the mothers
• Informed written Consent was taken from the mothers who participated.
• Data was collected according to the objectives using validated and reliable tools.
Results
[Table 1] Data presented in the table, reveals that majority of the mothers(56) were in the age group of 20-30 years. Regarding religion majority (73) mothers were Muslim & only 27 were Hindu. Data shows that majority of the mothers (71) belonged to primary level of education and only one of the mothers had higher secondary level of education. On the other hand, majority of the husbands (64) had primary level of education, and only one of them was graduate [16-20]. [Table 2] Data presented in the table shows that all the mothers were house wife. Majority (55) of the participant’s husbands were labour. Data also showed that majority (58), of the mothers were living in joint family and majority of the mothers (75) were having more than four members. Maximum (39) of the participant’s per capita income was between Rs1095-Rs548 and only 10 had per capita income of Rs 3652-Rs 1896. Majority (51) of the mothers were having more than four km distance from nearest health centre.[Table 3] The data presented in the table shows that majority (52) of the mothers were primi para and 48 were multi para. Majority (67) of the last deliveries were conducted in hospital and 10 in home. Regarding mode of last delivery, majority (65) of the mothers delivered normally and 35 mothers delivered by caesarean section. Majority (52) of the deliveries were conducted by the nursing staff and 10 by Dai. [Table 4]
| Sl.No. | Sample characteristics | f |
|---|---|---|
| 1. | Age -20 yrs. -20-30 yrs. -31-35 yrs. |
41 56 03 |
| 2. | Religion - Hindu - Muslim |
27 73 |
| 3. | Mother’s education -Illiterate -Primary - Secondary - Higher Secondary - Graduate |
12 71 16 01 - |
| 4. | Husband’s education - Illiterate - Primary - Secondary - Higher secondary - Graduate |
16 64 15 04 01 |
Table 1: Frequency distribution of mothers according to their personal characteristics. N= 100
Sl.No. |
Sample characteristics | f |
|---|---|---|
| 1. | Mother’s occupation - House wife - Labour |
100 - |
| 2. | Husband’s occupation - Farmer - Labour - Business - Service - Private Tutor |
24 55 13 07 01 |
| 3. | Type of family - Nuclear - Joint |
42 58 |
| 4. | No of family member - 2-4 - >4 |
25 75 |
| 5. | Per capital income - Rs 547 & below -Rs 1095-Rs 548 -Rs 1895- Rs 1096 -Rs3652-Rs1896 |
30 39 21 10 |
| 6. | Distance of nearest health centre - <2km - 2-4km - >4km |
45 04 51 |
Table 2: Frequency distribution of mothers according to the socio- economic characteristics. N=100
Sl.No. |
Sample characteristics | f |
|---|---|---|
| 1. | Para Primipara Multipara |
52 48 |
| 2 | Place of last delivery Home District hospital Nursing home |
10 67 23 |
| 3 | Mode of last delivery Normal delivery Caesarean section |
65 35 |
| 4 | Last delivery conducted by Doctor Nurse Dai |
38 52 10 |
Table 3: frequency and percentage distribution of mothers related to the obstetrical history.
N=100
Sl.No |
Sample characteristics | f |
|---|---|---|
| 1. | Sex of the last baby Male Female |
41 59 |
| 2. | Condition of the last baby immediately after birth Cried Not cried Congenital anomalies |
98 02 - |
| 3. | Complication arised of the last baby after birth Jaundice Birth asphyxia Hyperthermia No complication |
01 02 01 96 |
Table 4: Frequency and percentage distribution of the mothers related to the condition of the last
baby at birth. N=100
Table 4 reveals that majority (59) of the last baby were female. Majority (98) of the last baby cried immediately after birth and two had birth asphyxia and one had jaundice and hyperthermia respectively [21-25].
Section 2: Findings related to utilization pattern of postnatal services of the mothers
This section describes the utilization pattern of postnatal services of 100 participants in terms of, number of postnatal visits, place of first post natal visit, first post natal visit conducted by, utilization of subsequent post natal check-up, areas of health advice received and immunization of the last baby upto 6 weeks of age [Table 5]
| Sl. No. | Sample characteristics | f | n | % |
|---|---|---|---|---|
| 1. | Post natal visit - 3 visit -< 3 visit - No visit |
34 65 01 |
100 |
34 65 01 |
| 2. | Place of 1st post natal check up -Hospital -Nursing home -Home |
67 23 09 |
99 | 68 23 09 |
| 3. | 1st post natal check up by -Nurse -Doctor -Health worker |
35 62 02 |
99 | 35 63 02 |
| 4 | Subsequent post natal check up - Received -Not received |
57 42 |
99 | 58 42 |
Table 5:Frequency and percentage distribution of the mothers according to the utilization pattern of post natal service. N= 100
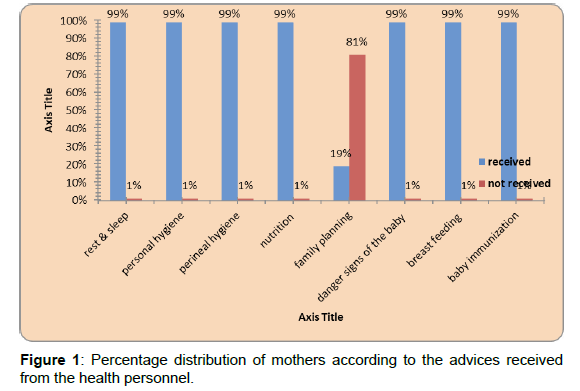
Data presented in the table 5 shows that majority (66%) of the mothers received less than 3 post natal visit. From further investigation, the investigator found that one mother did not receive any post natal check-up. Out of 99 mothers majority (81%) received first postnatal check-up from institution and among them majority (63%) were checked by doctor. Data again reveals that 58 percent mothers received subsequent postnatal checkup. [Figure 1]
The data presented in the table shows that majority (99%) of the mothers received advice from health personnel in the areas of rest and sleep, personal hygiene, perineal hygiene, nutrition, danger signs of the baby breast feeding and baby immunization, whereas majority (81%) of the mothers did not receive health advices on family planning. [Table 6]
| Sl. No. | Sample characteristics | f |
|---|---|---|
| 1. | OPV- 0 dose Received |
95 |
| 2. | OPV- 1 Received |
84 |
| 3. | BCG Received |
95 |
| 4. | Hb-1 Received |
79 |
| 5. | DPT-1 Received |
83 |
Table 6: Frequency and percentage distribution of last baby related to immunization upto 6 weeks of age.
N= 100
The data present in the table 6 shows, majority (95%) of the last baby received OPV -0 dose and B.C.G, 84% received OPV-1, 79% received Hb-1 and 83% received DPT-1.
Section 3- Findings related to the factors of the utilization and non -utilization of post natal Services
This section describes the factors for utilization and non-utilization of post natal services of 100 participants in terms of utilization and non-utilization of first post natal visit, subsequent postnatal services, immunization on schedule date. [Table 7]
| Sl.No | Factors | n | Frequency | Percentege |
|---|---|---|---|---|
| 1. | First post natal services :Health worker advised |
99 |
89 - 10 |
89 11 |
| 2 | Subsequent postnatal service: :Illness of the baby |
57 | - 14 36 07 |
- 25 63 12 |
| 3. | For not recieving Subsequent post natal service : :Not aware :Baby’s illness, :Mother’s illness |
42 | 42 - - |
100 |
Table 7: Frequency and percentage distribution of mothers according to factors of utilization and non utilization of post natal services. N=100
Table 7 reveals that for utilization of first postnatal visit majority (89%) were for health worker advice and only 11 percent for health worker’s visit at home. Regarding utilization of sub sequent post natal service majority (63%) were for immunization of the child and only 12 percent for self-illness. The table further depicts that out of 42 mothers, all the mothers did not receive subsequent post natal service as not being aware. [Table 8]
| Immunization | n | Institutional delivery f % |
Mothers awareness f % |
Health worker’s advice f % |
||||
|---|---|---|---|---|---|---|---|---|
| 0.P.V-0 | 95 | 90 | 95 | 02 | 02 | 03 | 03 | |
| B.C.G | 95 | 90 | - | 02 | 02 | 03 | -03 | |
| O.P.V-1 | 84 | - | - | 21 | 25 | 63 | 75 | |
| Hb-1 | 79 | - | - | - | - | 79 | 100 | |
| D.P.T-1 | 83 | - | - | - | - | 83 | 100 | |
Table 8: Frequency and percentage distribution of last child according to factors of receiving immunization on scheduled date. N = 100
The table shows that out of 95 babies (95%) received OPV-“0” and B.C.G for institutional delivery and only two percent for mother’s awareness. Out of 84 babies majority (75%) received OPV-1 for health worker’s advice and 25 percent for mother’s awareness .For Hb- 1vaccine out of 79 babies all of them received as their mothers were aware. Out of 83 babies all of them received DPT-1 because of health worker’s advice. [Table 9]
| Immunization | n | Not aware | Non availability of vaccine | Baby’s illness | Mothers illness | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| f | % | f | % | f | % | f | % | |||||
| O.P.V -0 | 05 | - | - | 04 | 80 | - | - | 01 | 20 | |||
| B.C.G | 05 | - | - | 04 | 80 | - | - | 01 | 20 | |||
| O.P.V-1 | 16 | 15 | 94 | 01 | 06 | |||||||
| DPT - 1 | 17 | - | - | 14 | 82 | 02 | 12 | 01 | 06 | |||
| Hb -1 | 21 | - | - | 20 | 95 | - | - | 01 | 05 | |||
Table 9: Frequency and percentage distribution of mothers according to factors of not receiving immunization of last baby on scheduled date.N = 100
The data presented in the table shows that out of 5, majority (80%) of the last babies did not receive O.P.V-0 and B.C.G for non-availability of the vaccine and20 percent for mother’s illness. Out of 16 babies, 94percent did not receive O.P.V-1 for non-availability of vaccine and six percent for mother’s illness. For D.P.T-1, out of 17 babies, 82percent did not receive for non-availability of the vaccine and six percent for mother’s illness. Out of 21 babies, 95 percent did not receive for nonavailability of vaccine and five percent for mother’s illness.
Section 4- Findings related to the satisfaction level of mothers related to the post natal services.
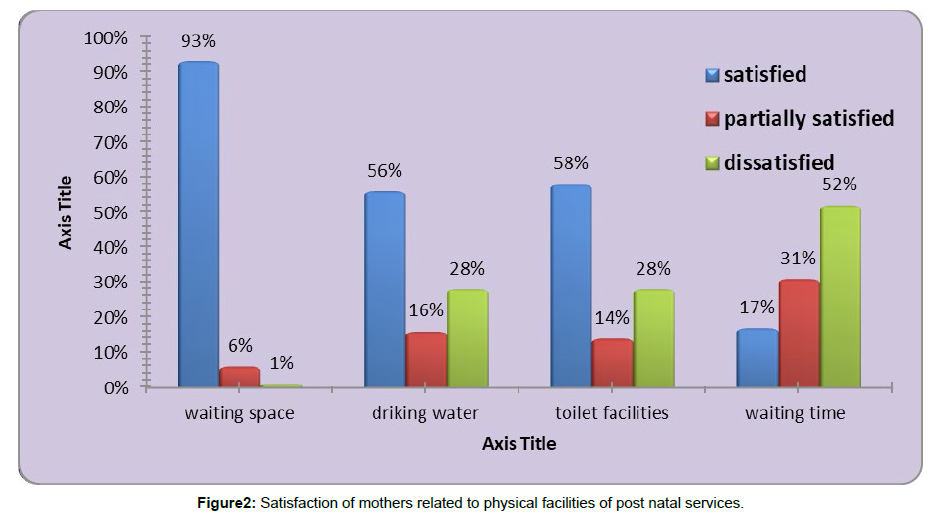
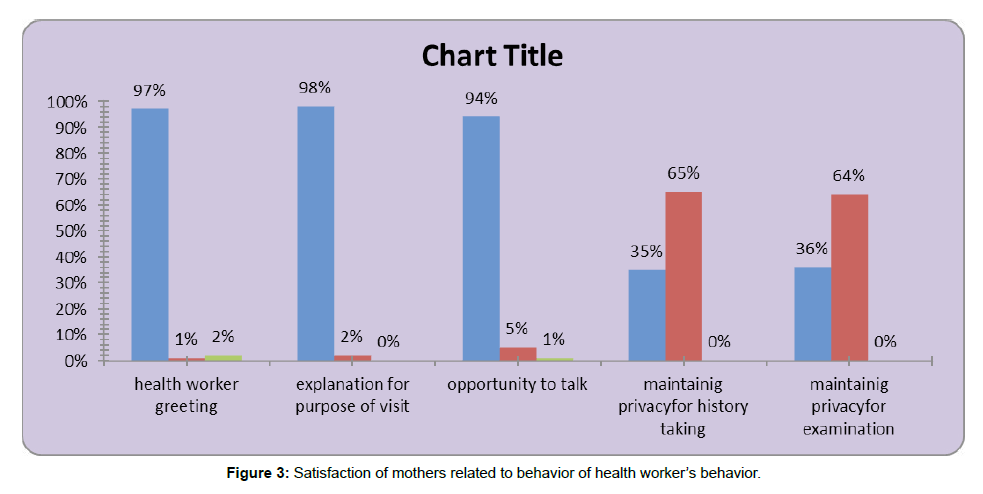
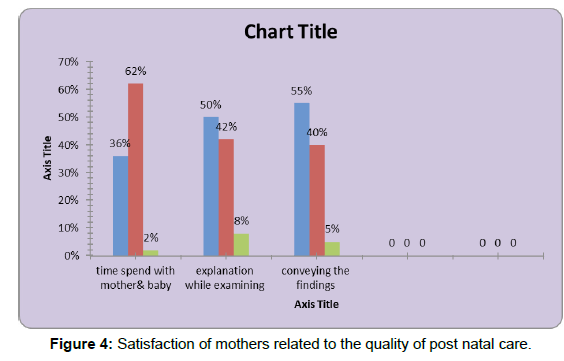
This section describes the satisfaction level of 100 mother related to areas of physical facilities- (waiting space, drinking water, toilet facilities and waiting time), health worker’s behavior (health worker’s greeting, explanation for purpose of visit, opportunity to talk, maintaining privacy for history taking, maintaining privacy for examination), quality of postnatal care (time spend with the mother and baby, explanation while examining, conveying the findings of the study). [Figure 2]
Above bar diagram represents that majority of the mothers were satisfied related to physical facilities of the institution for postnatal service like waiting space (93%), drinking water (56%), toilet facilities (58%) except waiting time where only (17%) Mothers were satisfied. [Figure 3]
Above figure depicts that majority of the mothers were satisfied with health workers behavior related to greetings (97%), explanation regarding purpose of the visit (98%), opportunity to talk (94%). Figure also shows that majority of the mothers were partially satisfied with health worker’s behavior related to maintaining privacy for history taking(65%) and for maintaining privacy for examination (65%). [Figure 4]
Figure 4 shows that majority of the mothers (63%) were partially satisfied with time spend with mother and baby by the health worker. Regarding explanation while examining (50%) and conveying the findings majority (55%) of the mothers were partially satisfied.
Section 5- Findings related to the association of selected factors with utilization of postnatal services.
[Table 10]
| Sl.No. | Selected variables | Utilization pat | Chi-square value | |
|---|---|---|---|---|
| 3 visit | <3 visit | |||
| Mother’s education -Primary & below -Above primary |
32 02 |
44 22 |
5.8* | |
| 2 | Husband’s education -Primary & below -Above primary |
31 03 |
50 16 |
2.7 |
| 3 | Per capita income - < 1095 -> 1096 |
25 19 |
27 29 |
0.6 |
| 4 | No. of living children -1 - >1 |
25 19 |
27 29 |
0.6 |
| 5 | Type of family - Nuclear -Joint |
17 17 |
09 57 |
1.7 |
| 6 | Distance of the nearest health centre from home - < 2km - 2-4km |
15 19 |
27 49 |
0.8 |
Table 10: chi-square value showing the association between numbers of postnatal visit with
selected factors.N=100
Chi square (x2)* df(1)= 3.841, p>0.05
Table 10 reveals that there is significant association of utilization pattern of post natal services with mother’s education at 0.05 level of significance and also there was no significant association of utilization pattern of post natal services with husband’s education level, per capita income, number of living children, type of family and distance of home from nearest health center. [Table 11]
| Sl.No. | Selected variables | Utilization pat | Chi-square value | |
|---|---|---|---|---|
| 3 visit | <3 visit | |||
| 1 | Place of delivery -Institutional -Home |
28 06 |
62 04 |
3.34 |
| 2 | Mode of delivery -Normal -Caesarean |
09 23 |
54 12 |
|
| 3 | Delivery conducted -Health personnel -Dai |
28 06 |
62 04 |
3.34 |
| 4 | Sex of the last child -Male -Female |
18 16 |
23 43 |
30.3* |
| 5 | Condition of last baby at birth -Cried -Not cried |
33 01 |
65 01 |
0.07 |
| 6 | Complications of the last baby -Yes -No |
03 31 |
01 65 |
1.5 |
Table 11: chi-square value showing the association between numbers of postnatal visit with selected factors.
N = 100
Chi square (x2)* df(1)= 3.841, p>0.05
Table 13 reveals that there is significant association of utilization pattern of post natal services with mode of delivery and sex of the last child at 0.05 level of significance and also there was no significant association of utilization pattern of post natal services with place of delivery, delivery conducted by, condition of the last baby at birth, complications of the last baby. [Table 12]
| Sl.No. | Selected variables | Immunization on schedule date | Chi-square value | |
|---|---|---|---|---|
| Received | Not received | |||
| Mother’s education -Primary & below -Above primary |
62 18 |
18 02 |
2.4 | |
| 2 | Husband’s education -Primary & below -Above primary |
67 13 |
14 06 |
5.1* |
| 3 | Per capita income - < 1095 -> 1096 |
51 28 |
18 03 |
4.5* |
| 4 | No. of living children -1 - >1 |
40 40 |
12 08 |
0.6 |
| 5 | Type of family - Nuclear -Joint |
24 56 |
02 18 |
0.02 |
| 6 | Distance of the nearest health centre from home - ≤ 4km- - > 4km- |
38 42 |
11 09 |
0.36 |
Table 12: Chi-square value showing the association between receiving immunization on schedule date with selected factors. N=100
Chi square (x2)* df(1)= 3.841, p>0.05 Table , reveals that there was significant association between receiving immunization on schedule date with husband’s education and per capita income at 0.05 level of significance. The table also reveals that there was no significant relationship between receiving immunization on schedule date with number of living children, type of family and distance of nearest health center from home. [Table 13]
| Sl.No. | Selected variables | Immunization on schedule date | Chi-square value | |
|---|---|---|---|---|
| Received | Not received | |||
| 1 | Place of delivery -Institutional -Home |
73 07 |
17 03 |
0.17 |
| 2 | Mode of delivery -Normal -Caesarean |
48 32 |
17 03 |
2.99 |
| 3 | Delivery conducted -Health personnel -1096 |
73 07 |
17 03 |
0.17 |
| 4 | Sex of the last child -Male -Female |
33 37 |
08 12 |
0.6 |
| 5 | Condition of last baby at birth -Cried -Not cried |
79 01 |
19 01 |
0.031 |
| 6 | Complications of the last baby -Yes -No |
02 78 |
02 18 |
0.047 |
Table 13 reveals that there was no significant association between receiving immunization on schedule date with place of delivery, mode of delivery, delivery conducted by, sex of the last child, condition of the last baby at birth, complications of the last baby [26-30].
Conclusion
The study showed that (10%) deliveries were conducted at home. The study revealed that majority (99%) of the mothers had no knowledge regarding postnatal services & only 1% of the mothers had knowledge about postnatal services. The study also revealed that (99%) of the mothers received post natal services and (1%) did not receive any post natal service. About (81%) of the mothers did not receive any advice on family planning.
References
- Dutta DC (2004) The text book of obstetrics. 6th edi. Calcutta: New Central Book Agency.
- Banerjee B (2006) Maternal Care Rendered at an Urban Health Centre of a Metropolitan City. Indian Journal of Community Medicine 31: 183-184.
- Park K (2009) Park’s textbook of preventive and social medicine. 20th ed. Jabalpur : M/S Banarasidas.
- Annie Mwangi, Charlotte E Warren, Nancy Koskei, Holly Blanchard (2011) Frontiers in Reproductive Health. Strengthening Postnatal Care Services Including Post Partum Family Planning in Kenya.
- Kishore J (2007) National Health Programmes of India’’, 9th edition, New Delhi: Century Publication.
- “Ayushmati Scheme” Health & Family Welfare Department Govt. of West Bengal.
- (2008) WHO Technical Consultation on Postpartum and Postnatal Care,
- Agarwal P, Singh MM , Gargh S (2007) Maternal Health Care Utilization Among Women in Slum in Delhi. Indian Journal of Community Medicine 32: 203-205.
- Chawla M (2009) An Exploratory study to assess common problems after delivery among postnatal mothers at selected hospitals of Indore. Society of Midwives-India 168: 139.
- Thippaiah A, Washington R (2009) ‘Postpartum period’ -The window of opportunity. of Midwives -India 2050: 92.
- Sinha RN, Dasgupta S, Pal D, Mondal NK, Karmakar PR, et al. (2001) Coverage of Maternal care services in the state of West Bengal. Indian J Public Health 1045: 116-124.
- (2011) Maternal Health Division Department of Family Welfare, Ministry of Health and Family Welfare. Guidelines for Antenatal Care and Skill Birth Attendance at Birth by ANMs and LHVs.
- Roy Tk, Espeut D, Bhattacharya B, Lahiri S, Sahu D (2001) National Family Health Survey (NFHS -3)West Bengal.
- Lomoro OA, Ehiri JE, Quian X, Tang SL (2002) Mothers’ perspectives on the quality of postpartum care in Central Shanghai, China, International journal for quality in health care journal of the International Society for Quality in Health Care ISQua . 14(5): 393-402.
- Digambar A, Chimankar I, Harihar S (2011) Factors influencing the Utilization of Maternal Health CareServices in Uttarakhand. Ethno Med 5(3): 209-216.
- Maryan R, Sakineh M, Homa U, Narges R (2011) Postpartum morbidity and help- seeking behaviours in Iran. British Journal of Midwifery 19: 3.
- Rahman MM, Haque SE, Zahan MS (2011) Factors affecting the utilisation of postpartum care among young mothers in Bangladesh. Health Soc Care Community 19(2):138-147.
- John Tingle (2011) Women’s experience of maternity care in England: areas of concern. British Journal of Nursing 20: 14.
- Titaley CR, Dibley MJ, Roberts CL(2009)Factors associated with non-utilisation of postnatal care services in Indonesia. J Epidemiology Community Health 63(10): 827-831.
- Mattias R, Cecilia J, Jerker L, Birgitta E (2009) Social differentiation and embodied dispositions: a qualitative study of maternal care-seeking behaviour for near-miss morbidity in Bolivia. Reproductive Health, 6:13.
- Palas D, Mausumi B, Tikadar T, Biswas GC, Mridha P, et al. (2010) Client Satisfaction on Maternal and Child Health Services in Rural Bengal. Indian J Community Med. 35(4): 478-481.
- Daniela Salas (2009) Poor service utilisation related to childbirth predisposes to high MMR among rural women of South 24 Parganas, West Bengal, India.
- Sengupta M (2009) Utilization Pattern of Postnatal services by the women of a rural community in a selected district of West Bengal. Society of Midwives l: 177.
- Enas D, Rafael T Mikolajczyk, Annette EM, Alexander K (2008) Factors associated with lack of postnatal care among Palestinian women: A cross-sectional study of three clinics in the West Bank. BMC Pregnancy and Childbirth 8:26.
- Abdal H, Sabry A (2008) Utilization of Postnatal Care in Al-Hassa, Saudi Arabia. Middle East Journal of Family Medicine 6(9)
- Nabukera SK, Witte K, Muchunguzi C, Bajunirwe F, Batwala VK, et al. (2006) Use of postpartum health services in rural Uganda: knowledge, attitudes, and barriers. J Community Health 31(2): 84-93.
- Lagro M, Liche A, Mumba T, Ntebeka R, van Roosmalen J (2006)Postpartum care attendance at a rural district hospital in Zambia. Trop Doct 36(4):205-208.
- Bryant AS, Haas JS, McElrath TF, McCormick MC (2006)Predictors of compliance with the postpartum visit among women living in healthy start project areas. Maternal Child Health J 10(6):511-516.
- Bhargava PK Ragni B (2007) Improvement in the Quality of Reproductive Health CareServices: Analyses of RCH Intervention project in one of the backward states of India.
- Matijasevich A, Santos IS, Silveira MF, Domingues MR, Barros AJ, et al. (2009) Inequities in maternal postnatal visits among public and private patients: 2004 Pelotas cohort study. BMC Public Health 335.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Roy MB (2022) Identification of the Factors of Utilization Pattern of Post Natal Services the Mothers and Their Satisfaction Level in a Selected Rural Community, West Bengal. Glob J Nurs Forensic Stud, 6: 205. DOI: 10.4172/2572-0899.1000205
Copyright: © 2022 Roy MB. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 1583
- [From(publication date): 0-2022 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 1240
- PDF downloads: 343