Hypersensitivity: An Overview
Received: 10-Oct-2018 / Accepted Date: 18-Oct-2018 / Published Date: 29-Oct-2018
Keywords: Hypersensitivity; Allergies; Autoimmune reaction; Anaphylaxis
Introduction
The human immune system is an essential part of defense against infection; however the general defending immune system can occasionally produce harmful response to the host [1]. Such responses are identified as hypersensitivity response, as well as the study of these is called immunopathology. This term came from the impression that the persons who have been formerly exposed to an antigen, marked noticeable responses to that antigen later and are consequently supposed to be sensitized [2]. Hypersensitivity responses can be produced through endogenous self-antigens or exogenous antigens. Immune reactions for endogenous or self-antigens effects in autoimmune diseases [3]. On the other hand, immune response may take variety of forms against exogenous antigens such as microbial and non-microbial (i.e. drugs, foods, pollens, chemicals and dust) components. Some of the most common reactions to exogenous antigens cause the group of disease known as allergy which has variety of symptoms ranging from itching, rash, fever, asthma and anaphylaxis.
Hypersensitivity generally results when an inequity happens among the effector mechanisms and the regulator mechanisms that typically function to limit such reactions. The progress of hypersensitivity I responses is related to the inheritance of specific genes. HLA genes and many non-HLA genes have been associated in many infection specific cases. Immunological reactions containing specific T-cells or IgG antibodies can also result hypersensitivity responses. While these effectors support of the immune reaction usually contribute in defending against infection, respond to noninfectious antigens to generate acute or chronic hypersensitivity responses [4]. Due to the complex properties, it is difficult to deliver a complete understanding of all aspects of immunology in this particular article. The purpose of this article is to present a general idea to the main components and properties of hypersensitivity reaction.
Classification Of Hypersensitivity Responses
Gell and Coombs in 1963 classified the identified hypersensitivity responses in four types based on the mechanism of action. Type I hypersensitivity responses are immediate allergic reactions (i.e. anaphylaxis), where type II involves antibody mediated cytotoxic response to particular tissues. Type III hypersensitivity responses are mediated by antibody-antigen complex which causes several types of tissue damage within the body. Type IV hypersensitivity or delayed type hypersensitivity are cell mediated responses that incorporate with sensitized T helper cells. Far ahead a fifth type of hypersensitivity was categorized to describe the stimulation of the endocrine system by immune responses in some autoimmune diseases. An overview of the hypersensitivity responses is summarized in Table 1.
| Type | Antigens | Immune reactant | Reaction |
|---|---|---|---|
| Type I hypersensitivity: Anaphylaxis, Drug allergy, Food allergy, asthma | Drug, food, dust, egg, Insect venoms, nuts, fish | IgE | Inflammation, oedema, Eczema, diarrhea. |
| Type II hypersensitivity: Hemolytic disease of the new born, Good pasture syndrome, drug sensitivity | Rh antigen, acetylcholine receptor | Antibody, IgG, IgM | Paralysis, anemia, nephritis |
| Type III hypersensitivity: Serum sickness, Arthus reaction, Systhemetic lulus erythematosus | Auto-antigen, DNA, mushroom spores | Immune complexes, Basophile, complement | Joint inflammation, nephritis |
| Type IV hypersensitivity: Delayed hypersensitivity | Poison Ivy, proteins, food, dust, chemicals, bacteria | T cells, Macrophages | Skin inflammation |
| Type V hypersensitivity: Graves’ disease | Thyroid stimulating hormone receptor | Antibody | Thyrotoxicosis |
Table 1: Overview of hypersensitivity response.
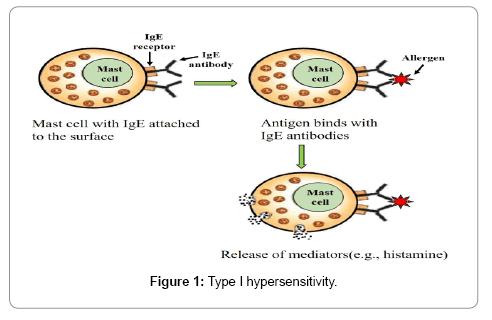
Type I hypersensitivity
Type I hypersensitivity is the immediate hypersensitivity caused by IgE antibody and results anaphylaxis to insect venoms, drug and food. These allergic reactions are systematic or local due to the induction of IgE antibody to allergens [5]. The type I hypersensitivity response is the product of an antigen cross link to membrane-bound IgE antibody of a basophil or mast cell. Histamine releases during the anaphylactic reaction and causes potential tissue damage inside the body (Figure 1).
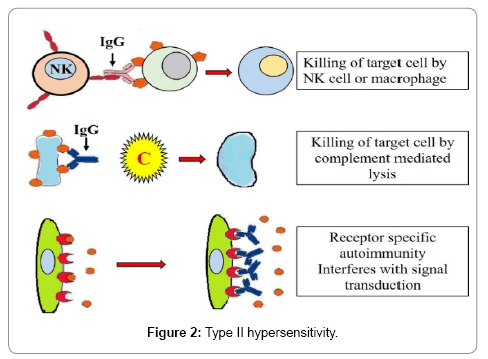
Type II hypersensitivity
Type II hypersensitivity responses are initiated by the toxic properties of antibody attached with antigens on the external of cells. The antibodies can activate complement dependent lysis which leads to tissue damage. In a cytotoxic reaction, the antibody responds right to the antigen which is attached to the cell membrane to activate cell lysis by complement induction [6]. These antigens could be “self ” i.e. autoimmune reactions or “non-self ”. Cytotoxic reactions are intermediated by IgM and IgG. One of the best examples of cytotoxic reactions is the Rh-incompatibility of a newborn. Other examples are blood transfusion reactions, Good pasture’s syndrome and autoimmune (Figure 2).
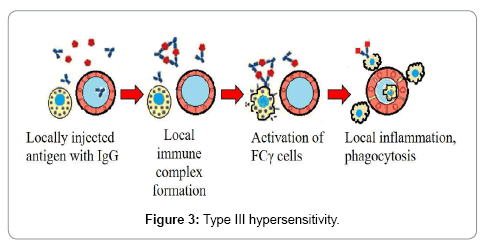
Type III hypersensitivity
Type III hypersensitivity is facilitated by the formation of antigen antibody complexes. IgG and IgM bind antigen, deposit antigenantibody (immune) complexes. This complex stimulates complement, which effects in PMN chemotaxis and initiation [7]. PMNs then discharge tissue damaging enzymes to the cell. One of the most common examples of type III hypersensitivity response in human body is serum sickness (Figure 3).
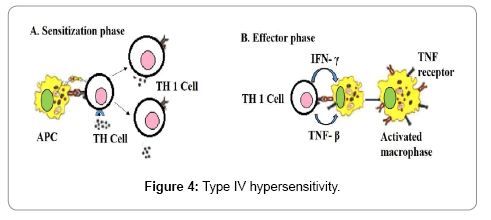
Type IV cell-mediated (delayed hypersensitivity)
Delayed or type IV hypersensitivity was initially described by its period course in which the responses took 12-24 hours of time to progress and persevered for 2-3 days. Cell-mediated responses are introduced by T-lymphocytes and intermediated by effector T-cells and macrophages. This reaction contains the antigens attached to the surface of lymphocytes. The pre-sensitized lymphocytes can induce cytokines, which can damage cells [8]. Many long-lasting diseases, including tuberculosis exhibits delayed type hypersensitivity (Figure 4).
Conclusion
Hypersensitivity reaction to food, insect venom, spore and drugs are not rare. Appreciatively, recent clinical research such as HLA tetramers and microarray techniques are likely to provide clinical application for hypersensitivity reaction.
References
- Silverstein AM (2000) Clemens Freiherr von Pirquet: Explaining immune complex disease in 1906. Nature Immunol 1: 453-455.
- Sampson HA (2005) Symposium on the definition and management of anaphylaxis: summary report. J Allergy Clin Immunol 115: 584-591.
- Basu S, Banik BK (2017) Autoimmune Disease: A Major Challenge for Effective Treatment. Immunol Curr Res 1: 103.
- Coombs RRA (1992) The hypersensitivity reactions - some personal reflections. Clinical and Experimental Allergy 22: 673-680.
- Moon TC, Befus AD, Kulka M (2014) Mast cell mediators: their differential release and the secretory pathways involved. Front Immunol 5: 569.
- Janeway CA, Travers P (1996) Immune responses in the absence of infection. In: Immunobiology. The Immune System in Health and Disease 11.1-11.46.
- Parham, Peter (2009) The Immune System (3rd edn) NY: Garland Science p. 390.
- Kay AB (1997) Allergy and Allergic Diseases. Oxford: Blackwell Science.
Citation: Basu S, Banik BK (2018) Hypersensitivity: An Overview. Immunol Curr Res 2: 105.
Copyright: © 2018 Basu S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 15613
- [From(publication date): 0-2018 - Apr 01, 2025]
- Breakdown by view type
- HTML page views: 14279
- PDF downloads: 1334