Human Infection with Hymenolepis Spp.: Case Reports from East Indonesia
Received: 05-May-2017 / Accepted Date: 30-May-2017 / Published Date: 05-Jun-2017
Abstract
Although rare, cases of hymenolepiasis (infection by Hymenolepis nana and Hymenolepis diminuta) could be found particularly in poor hygienic and sanitation areas. We conducted a community screening for intestinal parasite by stool examination using kato katz technique in Perobatang village, Southwest Sumba, East Indonesia on July 2016 and three cases of hymenolepiasis were found. First case was a 2-year old female child (H. nana) and the remaining two cases were female 32 years old (H. nana) and a male 38 years old (H. diminuta). The three cases were found positive for severe A. lumbricoides and T. trichiura infection. Diagnosis was acquired by history taking, physical examination and stool examination. Laboratory examination through peripheral blood smear was not performed due to the facilities limitation in the village. The 2-year old child came with the complaints of prolonged cough, cold, chronic diarrhea, low body weight and poor feeding. The adults presented with chief complaints of diarrhea and abdominal discomfort. Patients were given triple dose of 400 mg albendazole. The examination was conducted three weeks after the initial intervention found no signs of H. nana, H. diminuta and A. lumbricoides, however positive for mild T. trichiura infection, an improvement from an initial examination. The chief complaints were improved. Perobatang village is an underdeveloped village with difficulties in accessing clean water thus personal hygienic practices such as hand washing habits, uncontaminated food preparation, and bathing habits were substandard. Practice of open defecation is found due to the insufficient latrines. Improving hygienic practices, sanitation and health awareness are required to control cases of hymenolepiasis and other intestinal helminthiasis.
Keywords: H. nana; H. diminuta; Hygiene; Hymenolepiasis; Sanitation; Underdeveloped region
66339Introduction
Hymenolepiasis is cestode infection with Hymenolepis nana (the dwarf tapeworm, adults measuring 15-40 mm in length) and Hymenolepis diminuta (rat tapeworm, adults measuring 20-60 cm in length) as etiologies [1]. These cestodes affect rodents more often than humans. However, cases of human hymenolepiasis are often reported in places with poor hygiene and sanitation.
Hymenolepiasis most frequently occurs in warm, dry regions of the developing world, where exposure to human feces results in hand-tomouth infection. H. nana infects humans, especially in warm climates such as Asia, with the prevalence could be as high as 25% in some areas [2-5]. The prevalence in Indonesia remains unknown with independent sources claiming the rate between 0.3-5.4%, occurring mostly in children between 2-15 [6]. Infection of Hymenolepis sp. occurs following ingestion of insect-contaminated food supplies and hand-to-mouth exposure of contaminated feces which mostly in areas with poor hygiene and sanitation. H. diminuta is commonly found in areas where large amounts of rat’s favored food such as grain and other dry food-stored products [7]. Once the arthropod of the infective stage is ingested by the definitive host such as rodents and humans, it will develop into the adult form in the small intestine and its eggs will be passed in the stool of the host.
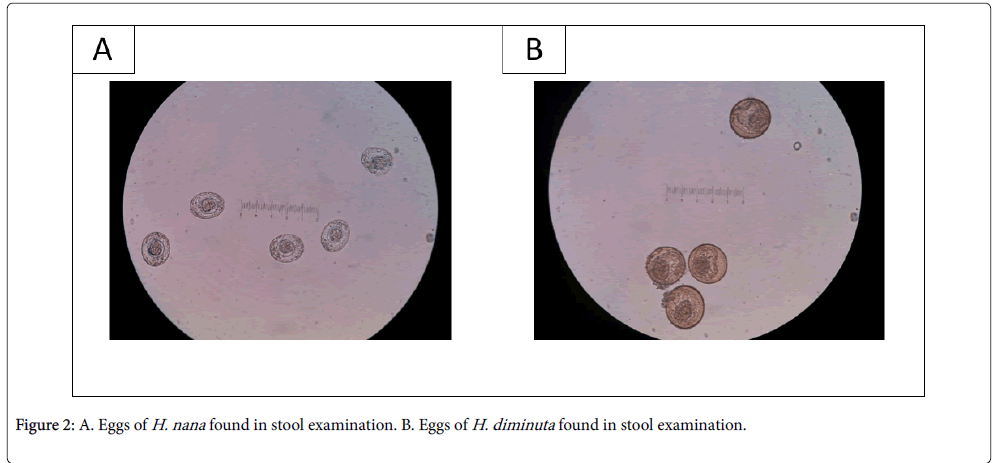
Mild hymenolepiasis is usually asymptomatic and heavy infection occurs usually due to autoinfection. Heavy infection results in headache, dizziness, anorexia, abdominal pain with diarrhea, nausea, vomiting, pruritus, and weight loss. Allergic reaction, such as urticarial, skin eruption, and phlyctenular conjunctivitis, may also occur [7-9]. Diagnosis is confirmed by egg findings in stool samples.
We present cases of hymenolepiasis found in an underdevelop district of Eastern Indonesia, Southwest Sumba. Southwest Sumba suffers from poverty, low education, and poor hygiene. The area lacks of clean water and people are required to walk few kilometers away from their villages to obtain water from public wells. People practice open defecation and rarely wash their hands thus the poor hygiene.
Prevalence of hymenolepiasis has been reported to be low in several developed countries. However, in underdeveloped places with poor hygiene and sanitation such as Southwest Sumba, hymenolepiasis often go undiagnosed. This case report aims to remind the importance of recognizing hymenolepiasis especially in such places.
Case Description
Faculty of Medicine Universitas Indonesia conducted a community health screening for intestinal parasite on July 2016 in Perobatang village, Southwest Sumba. Faecal samples were collected from 424 of 473 inhabitants (age two months to 80 years) of the village, processed with kato katz method and examined under light microscope. The most prevalent parasites were Ascaris lumbricoides 279/424 (65.8%), Trichuris trichiura 256/424 (60.4%) hookworms 227/424 (53.5%), Entamoeba histolytica cysts 76/424 (17.9%) and Giardia lamblia 19/424 (44.5%) [10]. Two cases of H. nana and one case of H. diminuta were found. Other laboratory examination was not performed due to limitation of facilities. As the prevalence of helminthiasis was above 50%, all participants were given triple dose of albendazole 400 mg for three consecutive days as a part of mass eradication according to WHO guideline.
This case report focuses on hymenolepiasis as it is a rare case and its presence indicates extremely poor hygiene and sanitation. Two cases of H. nana were found in two year old child and 32-year old woman while H. diminuta was found in 38-year old male. After these three cases were identified for hymenolepiasis, further history taking and physical examination were conducted.
The two-year old child presented with chronic cough, diarrhea, poor apetite, and mild malnutrition. Patient had been eating regular food for one year, mostly consisting of rice with fish or vegetables. The mother usually prepared food early in the morning to be consumed at breakfast, lunch, and dinner without being reheated in between. The mother did not wash her hands regularly prior to meal preparation and after family meal is usually put on top of the dining table without any lid thus often came in contact with flies and insects. Patient and her family also did not regularly wash their hands prior to meal. Patient underwent medication consisting of triple dose of 400 mg albendazole. After three weeks, patient was re-evaluated and there was no H. nana eggs found. Clinically, patient’s complaints were improved.
The adult patients presented with abdominal discomfort and diarrhea. Physical examinations revealed normal findings. These patients also lived with poor hygiene and sanitation. After treatment of triple dose of 400 mg albendazole, no H. nana and H. diminuta eggs were found in the stool examination. The three weeks evaluation after treatment revealed that patients had no more complaints.
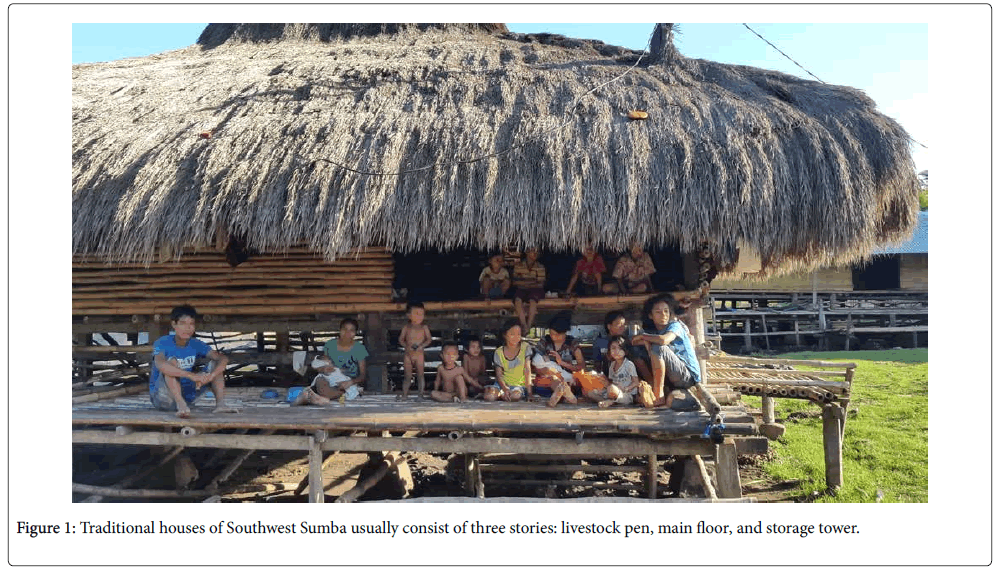
All patients live in similar conditions where houses consisted of three stories; livestock pen, the main floor, and the storage tower. Livestock roam freely in the village and their feces are spread across the lawn inviting flies to wander around. Rats are also common sight in the houses and storage tower where they keep their food supplies. These people also did not possess proper latrine hence their practice of open defecation.
Discussion
Perobatang Village, Southwest Sumba lies on tropical coastline of Indonesia with low rainfall rate and groundwater is hardly accessible without artesian well. To address this issue, the government made several wells however the number was insufficient to fulfill the needs of the villagers. These wells are located far from residential areas, around two to three kilometers. As many of them are poor, vehicles are mainly motorcycles for working purposes. Hence, villagers must walk to these wells to obtain clean water. Due to these reasons, people rarely wash their hands before meals and only bath once a week in these public wells. Water obtained from the wells is used for drinking and cooking purposes. There is no latrine available thus practice of open defecation is a common sight and they had no habit to wash their hands. This poor condition is a suitable breeding site for rodents and insects (Figure 1).
In this case report, we found cases of hymenolepiasis in a community health screening of Perobatang Village. Doctors and patients often do not suspect hymenolepiasis as its clinical manifestations are not specific and often mimic other diseases thus remain undiagnosed. Symptoms severity seems to correlate with increasing worm burden. Among children with clinical infection, symptoms include restlessness, irritability, diarrhea, abdominal pain, anal pruritus, headache, anorexia, vomiting, nausea, bloody diarrhea, hives, extremity pain, headache, dizziness, fatigue dyspepsia behavioral disturbances, and seizures [11]. Aside from rare abdominal tenderness or urticaria, physical examination is typically unrevealing.
The prevalence of hymenolepiasis in Indonesia is still unknown due to the limited epidemiological studies conducted for this disease. H. nana may cause autoinfection which could persist for years and lead to hyperinfection. Hyperinfection may also be achieved by ingesting contaminated grain products by infected insects such as grain beetles. When humans ingest eggs, the oncospheres enclosed in the eggs are released and penetrate into the villi of the small intestine. After maturation is complete (~7 days), they return to the intestinal lumen by rupturing the villi. Tissue immunity is acquired in this process; however, cysticercoids released from the insects could penetrate the intestinal villi more easily because villi do not exhibit tissue immunity conferred by harboring cysticercoids [6,7].
The patient in this case engaged in diet primarily consisted of vegetables. Added with poor hygiene of the residential area and meal preparation, we suspected these were the route of infection [7]. H. nana infection, although rare, still occurs in humans especially in underdeveloped districts in Indonesia due to its poor hygiene. Animal hosts such as rats may act as a reservoir for human infections. Its transmission is associated with environment contaminated with faeces, drinking contaminated water, poor sanitation and personal hygiene as well as infected person living in the same house.
H. diminuta is transmitted via ingestion of its definitive host, arthropods containing cystercoid larvae. Such arthropods are fleas (e.g. larval flea), beetles (e.g. flour beetle, grain beetle), flour moths, meal worms, cockroaches and caterpillars. These arthropods ingested the larvae from rodents’ faeces. Its clinical manifestations include abdominal pain, irritability, pruritus and eosinophilia (Figure 2) [12,13].
Preferred therapy is praziquantel, a bacteriocidal used in a single dose of 25 mg/kgBW in adults and children, effective for all the stages of the parasite. This drug is well tolerated and safe. Tablets should be taken with food and swallowed whole with liquids. Triple doze of 400 mg albendazole could also be used for hymenolepiasis cases with 68% cure rate. In this case, albendazole is used due to unavailability of praziquantel.
The village’s poor sanitation is noticeable from the limited availability of clean water; lack of garbage and human waste disposal; settlement of rats nesting; and presence of insects which could be the intermediate host. Previous study showed that poor hygiene and sanitation, especially when preparing food and covering food from insects are independent risk factors for intestinal parasitic infection [14,15]. The prevention and control of H. nana and H. diminuta infections could be achieved via improvement of environmental hygiene and lifestyle changes. Such efforts are required to break the cycle of disease epidemiology. Government along with medical practitioners are required to collaborate in controlling H. nana and H. diminuta infection.
Conclusion
Presence of hymenolepiasis cases in Perobatang Village, Southwest Sumba indicates extremely poor hygiene and sanitation where humans live closely with rodents and insects. Improvement of environmental hygiene and lifestyle changes are pivotal to control the spread of H. nana and H. diminuta.
References
- Mirdha BR, Samantray JC (2002) Hymenolepis nana: a common cause of paediatric diarrhoea in urban slum dwellers in India. J Trop Pediatr 48:331-334.
- Jacobsen KH, Ribeiro PS, Quist BK, Rydbeck BV (2007) Prevalence of intestinal parasites in young Quichua children in the highlands of rural Ecuador. J Health PopulNutr 25:399-405.
- Diaz E, Mondragon J, Ramirez E, Bernal R (2003) Epidemiology and control of intestinal parasites with nitazoxanide in children in Mexico. Am J Trop Med Hyg 68:384-385.
- Waloch M, Sobolewska A, Dzbenski TH (2010) Evaluation of epidemiological situation of cestode infections in Poland in the years 1997-2006 on the basis of data from sanepid stations. PrzeglEpidemiol 64:533-536.
- Anorital (2014) Literature review on Hymenolepis nana. Indonesian Journal of Biotechnology Medicine 3: 37-47.
- Syadaf HS, Khan SS, Kanwal N, Tasawer BM, Ajmal SM (2013) Review on diarrhea causing hymenolepis nana-dwarf tapeworm. IntRes JPhar 4:32-35.
- Kim BJ, Song KS, Kong HH, Cha HJ, Ock M (2014) Heavy Hymenolepis nana infection possibly through organic foods: report of a case. Korean J Parasitol 52:85-87.
- Di Lernia V, Ricci C, Albertini G (2004) Skin eruption associated with Hymenolepis nana infection. Int J Dermatol 43:357-359.
- Sungkar S, Pohan A, Ramadani A, Albar N, Azizah F, et al. (2015) Heavy burden of intestinal parasite infections in PeroBatangvillage, a rural area in South West Sumba, eastern part of Indonesia: a cross sectional study. BMC Public Health 15:1296.
- Cabada MM, Â Morales ML, Lopez M, Spencer T, Reynolds ST, et al. (2016) Hymenolepis nana impact among children in the highlands of Cusco, Peru: an emerging neglected parasite infection. Am J Trop Med Hyg95:1031-1036.
- Rohela M, Ngui R, Lim Y (2012) A case report of H. diminuta infection in a Malaysian child. Trop Biomed 29:224-230.
- Tena D, Simon MP, Gimeno C, Teresa M, Pomata P, et al. (1998) Human infection with H. diminuta: case report from Spain. J ClinMicrobiol36:2375-2376.
- Al-Mekhlafi AM, Abdul-Gani R, Al-Eryani SM, Saif-Ali R, Mahdy MA (2016) School-based prevalence of intestinal parasitic infection and associated risk factors in rural communities of Sana’a, Yemen. Acta Trop 163:135-141.
- Abdel Hamid MM, Eljack IA, Osman MK, Elaagip Ah, Muneer MS (2015) The prevalence of Hymenolepis nana among preschool children of displacement community in Khartoum state, Sudan: a cross-sectional study. Travel Med Infect Dis 13:172-177.
Citation: Sungkar S, Sianturi I, Kusumowidagdo G (2017) Human Infection with Hymenolepis Spp.: Case Reports from East Indonesia. Arch Parasitol 1: 104.
Copyright: © 2017 Sungkar S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 5857
- [From(publication date): 0-2017 - Apr 11, 2025]
- Breakdown by view type
- HTML page views: 4884
- PDF downloads: 973