Human African Trypanosomiasis in Burkina Faso from 2005 to 2011: Epidemiological, Clinical, Paralytic, Therapeutic and Evolutive Aspects
Received: 28-Oct-2019 / Accepted Date: 12-Nov-2019 / Published Date: 19-Nov-2019 DOI: 10.4172/2332-0877.1000411
Abstract
Purpose: The Goal of this study is to describe the aspects socio-demographic, clinical, diagnostic, therapeutic and evolutionary of African human trypanosomiasis (HAT) cases detected in Burkina-Faso from 2005 to 2011 in the context of major migratory phenomena of populations between Burkina Faso and Ivory Coast: A country where the disease is endemic.
Methodology: This is a descriptive retrospective study of patients with suspected clinical signs of human African trypanosomiasis (January 2005 to December 2011). The Card Agglutination Test for Trypanosomosis (CATT) was performed in first intention when available; it is completed parasitological tests for confirmation of cases.Data collection was based on laboratory consultation records and clinical case records. The management and analysis of the data was carried out using the software Epi info version 3.5.
Results: A total of 26 suspected cases of African human trypanosomiasis were recorded from 2005 to 2011. The mean age of the patients was 25 ± 10.3 years. The majority were males (88.5%) and most worked in the cocoa fields (76.9%). The notion of stay abroad was found in 73% of cases, mainly in Côte d'Ivoire.
At clinical level, clinical signs were somnolence and hypersomnia (34.6%), lymphadenopathy (23.1%), weight loss, pruritus and mood disorders (15.4% for each). Only one patient presented a trypanide.
At Para-clinical level, fifteen (15) cases were confirmed by sero-parasitological examinations of the 26-suspected cases collected, a prevalence of trypanosomiasis cases of 57.6%.
Most of the confirmed cases in Phase 2 were treated with Difluoro-Methyl Ornithine (DFMO) (69.2%). The death occurred in 26.5% of cases.
Conclusion: In Burkina Faso, human African trypanosomiasis remains relevant with the existence of imported cases. The efficient fight against this disease will go through strengthening the monitoring system and the technical platform of care.
Keywords: THA; Imported cases; Parasitological tests; Burkina Faso
Introduction
Human African trypanosomiasis (HAT), also known as sleeping sickness, is a parasitic disease that is transmitted to humans through a vector called hematophagous Glossina, commonly known as the tsetse fly.
It is caused by the two subspecies of the protozoan blood Trypanosoma brucei: Trypanosoma brucei gambiense responsible for 98% of the disease in West and Central Africa and Trypanosoma brucei rhodesiense in East and South Africa [1,2].
Sleeping sickness occurs exclusively in 36 countries in sub-Saharan Africa. In 1998, 40 000 cases of HAT were reported, but the WHO estimated that the number of infected persons reached 300 000 cases, and people at risk to 56 million cases [1]. The control efforts undertaken by WHO and the countries’ concerned has helped to reduce the incidence of the disease. In 2009, the number of reported cases dropped below 10,000 cases for the first time in 50 years, and in 2015, 2804 cases were reported [1,2].
In West Africa, the Ivory Coast reports the most new cases (300 to 500 per year). The disease is endemic in the forest in the Center-West and South-East of the country, planting areas for cash crops (coffee, cocoa, etc.)[3].
In Burkina Faso, historical and empirical data from AOF show that out of a total of 45,000 trypanosomes detected from 1931 to 1934, more than 30,000 came from Burkina Faso [4,5]. The medical and entomological control campaigns and the creation in 1986 of the National Program for the Control of African Human Trypanosomiasis (PNLTHA) then made it possible to progressively stem the epidemics and outbreaks of HAT.
However, the seasonal economic migration phenomena of the populations of Burkina-Faso in Côte d'Ivoire facilitate the circulation of the parasite and the recrudescence of HAT whose diagnosis and treatment are complex and require personnel with special skills. It is in this context that we conducted our study, which goal was to describe the socio-demographic, clinical, diagnostic, therapeutic and evolutionary aspects of trypanosomiasis cases detected in Burkina Faso from 2005 to 2011.
Methodology
This is a retrospective descriptive study of patients with suspected clinical signs of human African trypanosomiasis who were followed at the two sites for diagnosis and management of the national program for the control of human African trypanosomiasis. Burkina Faso. The study covers a period of five years from January 01, 2005 to December 31, 2011.
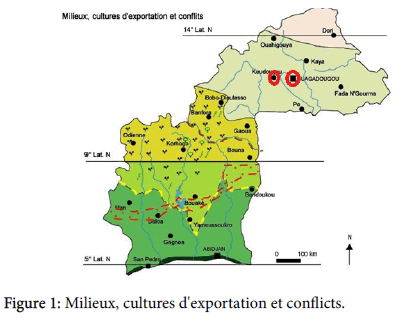
The first site for the diagnosis and management of human African trypanosomiasis in Burkina Faso is located in the city of Ouagadougou: it consists of a laboratory for the diagnosis of HAT and a small hospital room with two beds for the treatment of cases. The second site is located in the city of Koudougou in the Central West Region and the site was the Koudougou Health District Laboratory, located within the compound of the medical center to which must be added, two hospitalization rooms for the treatment of case (Figure 1).
All the patient presenting suspicious signs of HAT received in consultation at the two sites.
Several types of samples are taken according to the clinical presentation (blood, CSF, ganglionary puncture).
The following Para clinical tests are performed
The Card Agglutination Test for Trypanosomosis (CATT), which is made first, when it is present on the various, samples (blood, ganglionic juice and CSF).
The CATT is associated with the mini-Anion Exchange Centrifugation Technique (mAECT) for all CATT subjects whose test was positive at least at 1/4 dilution (CATT pl ≥ 1/4); it is more specific because is an element of certainty of the presence of the parasite. Then the parasitological tests are carried out (thick drop, fresh spreading, ganglionic juice, CSF).
A phase diagnosis is made to allow the choice of treatment by cytorachia and simple centrifugation of cerebrospinal fluid (SC LCR): Subjects in phase 1 (≤ 5 cells/μl LCR) and subjects in phase 2 (>5 cells/ μl LCR). In case of positivity, a treatment is instituted. The drugs used are either: Pentamidine, Arsobal (Melarsoprol), or Eflornithine (DFMO).
The post-treatment follow-up is done by periodic checks at 3 months, 6 months, 12 months and 24 months with resumption of seroparasitic examinations in search of the trypanosome in the blood, ganglionic juice and the CSF. After 24 months of follow-up with no positive result, that the case is declared cured.
NB: The diagnosis and management of HAT are free in Burkina Faso.
The data collection was done from the laboratory consultation records and clinical case records at the two sites and concerned the epidemiological, clinical, paraclinical, therapeutic and evolutionary aspects of the patients.
The management and analysis of the data was carried out using the software Epi info version 3.5
Results
A total of 26 suspected cases of African human trypanosomiasis were recorded from 2005 to 2011. The patients’ age was 25 ± 10, 3 years; the majority were males (88,5%) and most worked in the cocoa fields (76,9%). The notion of stay abroad was found in 73% of cases, mainly in Côte d'Ivoire.
Clinically, the main clinical signs were somnolence and hypersomnia in 34, 6% each followed by lymphadenopathies (23,1%). Weight loss, pruritus and mood disorders were each found in 15, 4% of cases. Only one patient presented a trypanide during our study (Table 1).
| Caractéristiques sociodémographiques | Effectif (%) |
|---|---|
| Age | |
| Average Age: 25 ± 10.3 [7-46] | |
| Sex | |
| Male | 23 (88.5) |
| Female | 3 (11.5) |
| Profession | |
| Planter | 20 (76.9) |
| Student | 5 (19.20) |
| Merchant | 1 (3.8) |
| Origin | |
| Koudougou | 15 (57) |
| Ouagadougou | 3 (11,5) |
| Other Cities | 1 (4) |
| Ivory Coast | 2 (7.5) |
| Concept of stays abroad | |
| Yes | 19 (73) |
| No | 7 (27) |
Table 1: Sociodemographic Characteristics of Patients.
Paraclinically, biological tests were performed using blood samples (34%), cerebrospinal fluid (CSF) (77%) or ganglionic juice (23%). Direct parasitological examination of CSF and sero-immunological test by CATT were the most frequently performed techniques in 57, 6% and 34.6% of cases, respectively. The trypanosome search was positive in the CSF in 64,7% of the cases, in the ganglionic juice in 83,5% of the cases, and 33% for the CATT, only one patient benefited from the mAECT and the test was positive (Table 2).
| Clinical characteristics | Numbers (%) |
|---|---|
| Drowsiness | 9(34,6%) |
| Hypersomnia | 9(34.6%) |
| Lymphadenopathy | 6(23,1%) |
| Emaciation | 4(15,4%) |
| Itching | 4(15,4% |
| Mood disorder | 4(15,4%) |
| Cephalalgia | 1(4%) |
| Trypanides | 1(4%) |
| Edema | 01(4%) |
| Other | 04(15,4%) |
Table 2: Patient distribution according to clinical characteristics.
During our study period, 15 cases were confirmed by seroparasitological examinations of the 26 suspected cases collected, are a prevalence of trypanosomiasis cases of 57,6%.
Most of the confirmed cases in Phase 2 were treated with Difluoro- Methyl Ornithine (DFMO) (69, 2%).
Progression after treatment resulted in death in 26, 5% of cases (Table 3).
| Samples | Test realized | Result | |||
|---|---|---|---|---|---|
| Natural samples | N (%) | Natural Test | N (5%) | Result | N (%) |
| Blood samples | 09 (34.6%) | Test immunological CATT | 09 (34.6%) | Positive | 03 (33.5%) |
| Negative | 6 (66.5%) | ||||
| Freshly spread blood | 04 (15.4%) | Positive | 01 (25%) | ||
| Negative | 03 (75%) | ||||
| Tick drop | 04 (15.4%) | Positive | 01 (25%) | ||
| Negative | 03(75%) | ||||
| mAECT | 01(03%) | Positive | 01 (100%) | ||
| Negative | 0 | ||||
| Puncture of LCR | 20 (77%) | LCR trypanosome search | 17 (57,6%) | Positive | 11 (64.7%) |
| Negative | 06 (35.3%) | ||||
| Ganglionic puncture | 06 (23%) | Trypanosome Research Ganglionic Suc | 06 (23%) | Positive | 05 (83.4%) |
| Negative | 01 (16.6%) | ||||
| Suspected case of trypanosomiasis | Cas positive | 15 (57.6%) | |||
| Cas negative | 10 (38.4%) | ||||
| Unspecified | 01 (4%) | ||||
Table 3: Distribution of patients according to the biological diagnosis of HAT.
Discussion
From 2005 to 2011, 15 cases of HAT in Trypanosoma brucei gambiense were confirmed in 26 suspected cases at the two national HAT control centers, a prevalence of 57, 6%. Men were predominantly more affected than women (sex ratio (M/F) at 7.7). This male predominance has also been described in Côte d'Ivoire and Guinea [6-8]. The average age is 25 ± 10.3 years [07 to 46 years].
Generally, mostly active young men are more susceptible to tsetse bites due to their farming and planting activities [3,5,6]. The majority of our patients had stayed abroad mainly in Côte d'Ivoire, a country in West Africa that reports the most cases of HAT. The disease is endemic and the contamination of our patients during their stay in Côte d'Ivoire is more than likely. It would therefore be an imported case of the disease. Kambiré et al. [9] demonstrated the epidemiological link between the Ivory Coast and Burkina Faso, in their study, all cases of trypanosomiasis found in Burkina Faso between 2010 and 2011 were cases imported from the Ivory Coast, in in addition, Meda et al. [7] showed that most cases of trypanosomiasis in Ivory Coast were either allogeneic or immigrants from other neighboring countries, particularly Burkina Faso, who came mainly to grow coffee and cocoa.
The Semiology signs observed in our patients were dominated by signs found in the meningoencephalic phase of HAT. The same symptomatology has been described by Courtin et al. [4] and Meda et al. [7] in Côte d'Ivoire as well as Camara et al. [8] in Guinea.
Thus, somnolence and daytime hypersomnia were present in 34.6% of cases followed by lymphadenopathy in 23,1%. The diagnosis was late for our patients received in consultation at the stage of meningoencephalitis and will be explained by the inaccessibility of the care services to planters who are in the forest areas far from the cities on the one hand and on the other hand by financial difficulties to return to Burkina Faso.
Unfortunately, it is only much later on their return that they consult the health structures and are diagnosed. Also, it should be emphasized that ignorance of the disease by some health workers could be a source of diagnostic wandering as well as customary beliefs and religious (witchcraft) constitute a barrier to screening for the disease [4,7,10,11].
During the study period, serological tests were performed poorly (CATT, MAECT). CATT was only available at a treatment site because of the expensive cost of the reagent, and the short lifespan of the reconstituted antigen (<7 days). It was systematically done before any other examination but frequent stock-outs were noted by the program. Thickness and fresh spreading were achieved only in 4 patients; because of the low sensitivity of these techniques, they are more and more abandoned [9]. The mAECT was only done in 1 patient. It is a sensitive technique but it is not systematically carried out in passive detection rather in the active search for cases.
Also due to the late signs presented by the cases, the trypanosome was sought directly in the CSF; anyway, any suspect case should benefit from a serological and parasitic test especially that the combination of the tests makes it possible to increase the sensitivity [12,13]; Positivity was 83% high in our patients who had lymphadenopathy.
The likelihood of finding trypanosome in the presence of lymphadenopathy was greater, only lymphadenopathy is not a common reason for consultation in our setting. Trypanosome screening in CSF was positive in 64.6% of patients with late-stage diagnosis of the disease in our setting; this technique allows not only the diagnosis of the disease, but also allows the diagnosis of the phase of the disease [9,11]. In our study, all our patients were in phase 2 of the disease.
Although some parasitological techniques allow a diagnosis of certainty, they offer less chance of finding the parasite, hence the need to perform combinations of techniques to increase the chances of finding the trypanosome [9,14]. In our study, the combination of techniques among the suspects was low (30, 7%).
Miezan et al. [13] showed that examination of combined ganglion juice and blood testing techniques increased sensitivity.
They demonstrated that with two techniques, the most sensitive was ganglionic juice-mAECT; and with three techniques, the most sensitive was ganglionic juice-mAECT-LCR double centrifugation. In our work context the mAECT is neither accessible nor available.
Due to numerous false-positive CATT results, Jamonneau's 2010 trypanolysis test (TL) is now used in trypanosomiasis control strategies in Burkina Faso since 2011. It allows identification among HIVpositive subjects in CATT but negative for parasitological tests, those must be considered as potential carriers of Trypanosoma brucei gambiense [11,15-19].
It is an indispensable tool for monitoring parasite circulation in West Africa.
Therapeutically, the majority of our patients were treated with DFMO which is being often diagnosed at the late stage of the disease (phase 2). Also for the last five years, the Arsobal molecule effective at all stages of the disease is abandoned, because of the frequency of reported relapses and its high toxicity (occurrence of encephalopathy in 05 to 10% of cases, fatal in 10 to 50%) of cases [6,7,9]. Thus, in Côte d'Ivoire, subjects in phase 2 which were treated with Arsobal (short 10- day regimen) are now treated with NECT (therapeutic combination of nifurtimox and eflornithine) since the end of 2010 [9].
On the evolutionary level, of the positive patients treated, most were cured (73,5%), but it should be emphasized that the lethality was important (26,5% of cases).
This high lethality could be explained by the delay in the diagnosis of the disease as evidenced by two cases of deaths noted before the start of treatment.
Conclusion
In Burkina Faso, human African trypanosomiasis is current; there is indeed an upsurge of cases imported from Cote d'Ivoire where the disease is hypo-endemic. It remains a disease of rural populations and remains a significant threat to working populations on plantations exposed to the bite of the tsetse fly. The diagnosis unfortunately is usually done at a late stage and is associated with high lethality. Strengthening surveillance, upgrading the technical platform for diagnosis and management and collaboration between the two trypanosomiasis control programs (Côte d'Ivoire and Burkina-Faso) are necessary for a good fight against sleeping sickness.
References
- WHO. African trypanosomiasis (sleeping sickness) WHO Media centre (2010).
- WHO. Control and surveillance of African trypanosomiasis. Report of a WHO Expert Committee. WHO Technical Report Series, 1998, 881.
- Pepin J, Meda HA (2001) The epidemiology and control of human african trypanosomiasis. Advances in Parasitology 49: 71-132.
- Courtin F, Jamonneau V, Kambire R, Solano P (2010) Crise ivoirienne et rapatriés burkinabés : Évaluation et vérification du risque de réémergence de la maladie du sommeil au Burkina Faso. Médecine Tropicale 70: 490-496.
- Courtin F, Rayaissé JB, Tamboura I, Serdébéogo O, Koudougou Z, et al. (2010) Updating the Northern Tsetse Limit in Burkina Faso (1949–2009): Impact of Global Change. International Journal of Environmental Research and Public Health 7: 1708-1719.
- Kaba D (2001) Situation épidémiologique et entomologique de la THA dans le foyer de Sinfra, deux ans après la campagne de lutte. Implication pour l’évolution du foyer. Thèse Médecine Université d’Abidjan-Cocody 2801: 156.
- Meda AH, Laveissiere C, Demuynck A (1993) Les facteurs de risque de la T.H.A. dans les foyers endémiques de côte d’Ivo i re. Med Trop 53: 83-92.
- Camara M, Kaba D, Kagbadouno M, Sanon JR, Ouendeno FF, et al. (2005) La trypanosomose humaine africaine en zone de mangrove en république de guinée : Caractéristiques épidémiologiques et cliniques de deux foyers voisins. Med Trop 65: 155-161
- Kambire R, Lingue K, Courtin F, Sidibe I, Kiendrébéogo D, et al. (2012) Human African trypanosomiasis in Côte d'Ivoire and Burkina Faso: optimization of epidemiologic surveillance strategies. Parasite 19: 389-396.
- Courtin F, Jamoneau V, Kambire R, Solano P (2010) Ivory Coast uprising and returning Burkinabe immigrants: evaluation of the risk for reemergence of sleeping sickness in Burkina Faso. Med Trop (Mars) 70: 490-496.
- Jamonneau V, Bucheton B, Kabore J, Ilboudo H, Camara O, et al. (2010 Revisiting the immune trypanolysis test to optimise epidemiological surveillance and control of sleeping sickness in West Africa. PLoS Negl Trop Dis 4: 917.
- Kiendrebeogo D, Kambire R, Jamonneau V, Lingue K, Solano P, et al. (2012) History of an epidemiological route between Ivory Coast and Burkina Faso: The case of the Koudougou sleeping sickness foci. Parasite 19: 397-406.
- Miezan TW, Meda AH, Doua F (1994) Evaluation des techniques parasitologiques utilisées dans le diagnostic de la trypanosomose humaine à trypanosoma Gambiense en Côte d’Ivoire. Bull Soc Path 87: 101-104.
- Carme B, Janin J, Eozonou P (1990) La Trypanosomiase Humaine Africaine. Editions Techniques, Encycl Med Chir, Maladie infetieuse 3: 14.
- Gentilini M, Duflo B, Carbon C Les Trypanosomiases Humaines. Médecine Tropicale, Maladies parasitaires Flammarion Médecine-Science 1972: 45-58.
- Penchenier L, Sanou SJR, Laveissiere C (2000) Manuel de lutte contre la maladie du sommeil en Afrique centrale et occidentale : Traitement OCEAC Yaoundé (Cameroun), IRD, Institue Pierre Richet Bouaké (Côte d’Ivoire) 2: 42.
- Jamot E (1933) Contribution à l’étude de la maladie du sommeil en Afrique Occidentale Française (Ouagadougou). Doc Tech OCCGE 492.
- Penchenier L, Laveissiere C (2000) Manuel de lutte contre la maladie du sommeil en Afrique centrale et occidentale : Généralités OCEAC Yaoundé (Cameroun), IRD. Institue Pierre Richet Bouaké (Côte d’Ivoire) 1: 66.
- Laveissiere C, Hervouet JP (1991) Trypanosomiase Humaine en Afrique de l’Ouest : Epidémiologie et contrôle. ORSTOM ed, collection Didactique, Paris 157.
Citation: Apoline KS, Déla-dem ATS, Jacques JZ, Arsène GO, Adama Z, et al. (2019) Human African Trypanosomiasis in Burkina Faso from 2005 to 2011: Epidemiological, Clinical, Paralytic, Therapeutic and Evolutive Aspects . J Infect Dis Ther 7: 411. DOI: 10.4172/2332-0877.1000411
Copyright: © 2019 Apoline SK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3269
- [From(publication date): 0-2019 - Nov 02, 2025]
- Breakdown by view type
- HTML page views: 2388
- PDF downloads: 881