Research Article Open Access
How Do Patients with Cognitive Impairment Communicate During Discharge Meetings? Evaluation of Participation Using Talking Mats
Liv Thalén1,2*, Ove Almkvist3,4 and Ing-Mari Tallberg1,21Department of Speech and Language Pathology, Karolinska University Hospital, Stockholm, Sweden
2Department of Clinical Science, Intervention and Technology, Karolinska Institutet, Sweden
3Department of Neurobiology, Care Sciences and Society Karolinska Institutet, Sweden
4Department of Psychology, University of Stockholm, Sweden
- *Corresponding Author:
- Liv Thalén
Karolinska University Hospital
Barngatan 69, Stockholm, Sweden
Tel: +46 70 99 811 81
Fax: +46 8 58 58 15 05
E-mail: liv.thalen@ki.se
Received date: February 04, 2016; Accepted date: March 18, 2016; Published date: March 26, 2016
Citation: Thalén L, Almkvist O, Tallberg ML (2016) How Do Patients with Cognitive Impairment Communicate During Discharge Meetings? Evaluation of Participation Using Talking Mats. J Speech Pathol Ther 1:106. doi: 10.4172/2472-5005.1000106
Copyright: © 2016 Thalen L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Speech Pathology & Therapy
Abstract
Objective: Individuals with dementia experience a declining capacity for communication, negatively affecting their ability to participate in discharge meetings. Communication problems might be obvious. Nevertheless patients often lack a structuralized support. The aim of this study was to investigate if communication could be facilitated by preparing patients for their discharge meetings using Talking Mats (TM), a visual communication-supporting device.
Methods: A pilot study was conducted, in which twenty patients participated, randomized to use TM prior their discharge meeting (Talking Mats Group, TMG) or to follow the ward’s usual procedure (Control Group, CG). Persons attending discharge meetings (patients, close acquaintances, nurses, and social care workers) at a geriatric ward rated on Visual analogue scale how well they perceived the patient participated in communication. They also rated to which extent utilizing TM had helped them.
Results: Our main finding was an interaction effect regarding how the four groups of persons attending the meeting (patients, close acquaintances, nurses, and social care workers) rated the three different statements regarding communication and participation; knowing the patient before the meeting affected the ratings of the patient’s communicative participation. A majority using TM rated that it had been beneficial during the discharge meetings. Comparison between groups yielded the contradicting result that in CG communication was rated as more well-functioning than in TMG.
Conclusion: Understanding each other is not a given in discharge meetings, especially when a patient has cognitive impairment, but the use of TM was rated as a communication facilitator by the persons attending. Having knowledge of a patient affected ratings of communication, and we conclude it is desirable to have the person utilizing the mat with the patient also attending the discharge meeting.
Keywords
Communication; Dementia care; Discharge planning; Patient care planning; Participation; Talking mats; Cognitive impairment; Dementia
Abbreviations
CG: Control Group; MMSE: Mini-Mental State Examination; TM: Talking Mats; TMG: Talking Mats Group
Introduction
Dementia is a disorder that is characterized by a decline in cognitive functions. Due to the resulting behavioral changes and reduced capacity to engage in everyday life activities, it is a major cause of dependency among elderly people [1]. Previous research has pointed out that the progressing impaired communication makes it challenging for the interlocutors to understand what people with cognitive impairment mean [2], along with making it more difficult for the patients to understand the possible risks and benefits of their different choices [3].
In spite of their eventual communicative and/or cognitive impairments, patients need to make healthcare decisions, and in order to have good compliance and treatment outcomes, it is important to engage the patient in the decision-making process [4-6]. Decisions within health care may include important and ethically complicated situations, such as choosing between treatments or joining a clinical trial, or it may involve changes to everyday life, such as the need for home care service. It is of ethical importance for staff to secure that a patient’s autonomy and independence at all times are promoted, but this might be in conflict with keeping the patient’s safety intact. Communicative problems might be obvious; nevertheless patients lack a structuralized support from personnel regarding their communication difficulties. It is not always known how providing such support can best be accomplished [7].
Talking mats (TM) is a low-technology visual framework that facilitates communication and decision-making and is used when a specific topic needs to be discussed. It consists of a small doormat on which picture cards with written expressions are manipulated to indicate the user’s responses. This method allows people with different communicative and/or cognitive impairments to express their views in a more understandable way by giving the opportunity to convey opinions on a picture-based scale. Previous research has examined how TM increases communication efficiency, showing an increase in how persons with dementia are able to express their views and participate in conversations [8]. The cognitive burden seems to be reduced using TM, facilitating the expression of opinions [9]. Furthermore, it enhances involvement in, as well as satisfaction with, discussions regarding everyday living [8,10].
At geriatric wards in Sweden, it is routine to hold a discharge meeting (also called joint meeting or patient care planning) at the end of hospitalization. The patient and a close acquaintance (if applicable) have a meeting with staff from the ward and a social care worker from the municipality. The purpose of the discharge meeting is to focus on the patient’s need for assistance when hospitalization ends, and to ensure that help is provided from the municipality after discharge by establishing a health plan [7]. Topics discussed during discharge meetings include establishing day-to-day routines (e.g., food delivery or cleaning) as well as handling major changes such as moving to a residential care unit. The patient’s expressed wishes along with his/her needs should serve as guidelines for the help that is provided by the municipality.
This pilot study’s aim was to explore communication and the potential benefit of preparing patients with cognitive impairment for their discharge meetings utilizing TM. We wanted to investigate how the patients’ communication in discharge meetings is perceived by the persons attending it, rated on the Visual Analog Scale (VAS). Differences in rated participation are compared between patients using TM (Talking Mats Group, TMG) and a Control Group (CG) [11].
Methods
Study design and sample
Patients were recruited from a geriatric ward at the Karolinska University Hospital. This ward gives priority to patients who need a multifaceted investigation of the factors affecting their memory and are not able to undertake the investigation at an open memory ward, as well as to patients with dementia and behavioral problems. Recruitment of patients in the project was consecutive and took place over the course of one year, from June 2013 to June 2014. The three inclusion criteria were (1): a diagnosis of clinical dementia or documented cognitive impairment, (2) the ability to talk Swedish (including sufficient hearing), and (3) the ability to use TM (including sufficient vision to see the pictures used). The ability to use TM was ensured by offering a training session using the TM framework (on the topic of ‘Activities’).
Approximately 300 patients were hospitalized at the ward during the recruitment time of the study. There were 40 patients who fulfilled the inclusion criteria and were scheduled for a discharge meeting. Of these, 20 consented to participate and were randomly assigned to one of two groups-the TMG (n=12) or the CG (n=8). Please see Ethical Considerations below regarding the consenting approach used for the study. As previous research have compared interview with TM with structuralized interview and non-structuralized interview [11], we chose to only use TM and a control group.
The comparability of the two groups was analyzed with regard to median age and median Mini–Mental State Examination (MMSE) score. MMSE is a cognitive screening test with a max score of 30 (indicating cognitive capacities are well functioning) which gives a rough measure of the dementia severity when the score is lower than maximum [12]. The mean age for the TMG was 76.8 (range 58-86, n=12) and their MMSE scores (obtained from medical records) had a mean value of 21.4 (range 13-27, n=9). For the CG the mean age was 70.8 (range 63-84, n=8) and their mean MMSE score was 20.3 (range 8-27, n=8). No statistically significant differences were found among the groups’ median ages (p>0.05) or their median MMSE scores (p>0.05), according to the Mann-Whitney U test. Calculations were also made to check for any correlations between MMSE and VAS ratings, but no significant correlations were found using Spearman’s correlation coefficient (two-tailed).
At each discharge meeting, the patient was asked to perform a selfevaluation, and the other persons attending were requested to evaluate the patient’s communication and participation, using statements with VAS. This resulted in ratings from four groups of persons attending: patients, close acquaintances, nurses, and social care workers.
Intervention
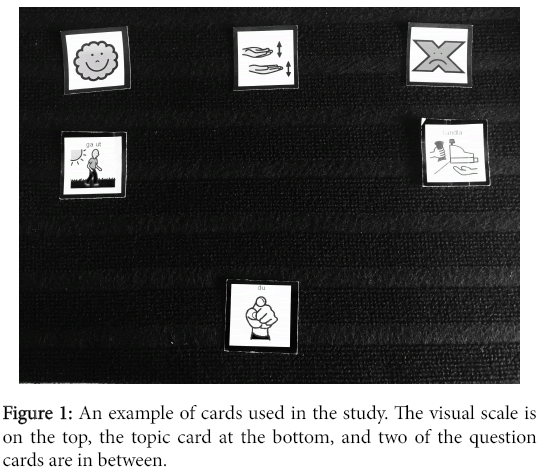
A standard set of cards with a picture and a corresponding expression on each were constructed in Boardmaker (a Mayer-Johnson software program). The cards measured 6.2 × 6.2 cm with a small Velcro tape piece on the back. Besides the top scale’s cards (‘functioning,’ ‘sometimes functioning/sometimes not,’ and ‘malfunctioning’) and the topic card (‘you’), there were 26 cards covering themes often discussed during discharge meetings. Of these 26, 5 regarded more abstract themes (e.g. ‘feeling safe’) and 21 regarded more concrete themes (e.g. ‘cleaning’). The patients were also given the opportunity to add written expressions or pictures on blank cards. The layout of the cards followed what has been described in previous studies regarding TM and dementia [10]. The selected cards were placed on a textured mat measuring 38 × 57 cm. See figure 1 for an example of the cards used.
Patients in TMG had a TM session prior to their discharge meeting to talk via the mat about themselves and their abilities (topic ‘you’). Each conversation took no longer than half an hour to complete. The completed mats were brought to the discharge meetings. The CG had their discharge meeting in accordance with the usual standards of the ward; no formalized conversation about potential topics took place before the discharge meeting. Discharge meetings typically included a summary of the patient’s hospitalization from the nurse (regarding diagnosis, treatment, observed behaviors and skills), and the social care worker provided information regarding any previously granted assistance. They also included a discussion about what assistance the patient needs, resulting in an application from the patient to the municipality regarding home care service.
Measures
After the discharge meetings all persons attending (patients, close acquaintances, nurses, and social care workers) were asked to rate three statements (on a 100 mm VAS), regarding perceived participation and communication on a scale, where 0 = I do not agree at all and 100 = I totally agree. All persons attending received the same statements, differing only in terms of point of view in relation to the patient: 1) I have understood what we have been talking about/I perceive that my close acquaintance/the patient understood what we have been talking about; 2) My views have been clearly expressed/I understood what my close acquaintance’s/the patient’s views were; 3) I thought the communication went well. The VAS was formulated inhouse since no standardized Swedish questionnaire for people with cognitive impairment with this focus exist to our knowledge. The questions used were clinically best practice for evaluating the communication abilities and participation in daily life activities of cognitively impaired individuals. Statement two and three are a Swedish somewhat modified translation from the English ‘Involvement Measure Questions’ previously used in research regarding communication and participation in people with cognitive impairment [8]. A picture was added at each end point of the patients’ scales. The two pictures were the same as used for expressing approval or disapproval in the TM session. Of the in total 74 ratings, there were 12 missing responses on statement 1 and 3, and 11 missing responses on statement 2.
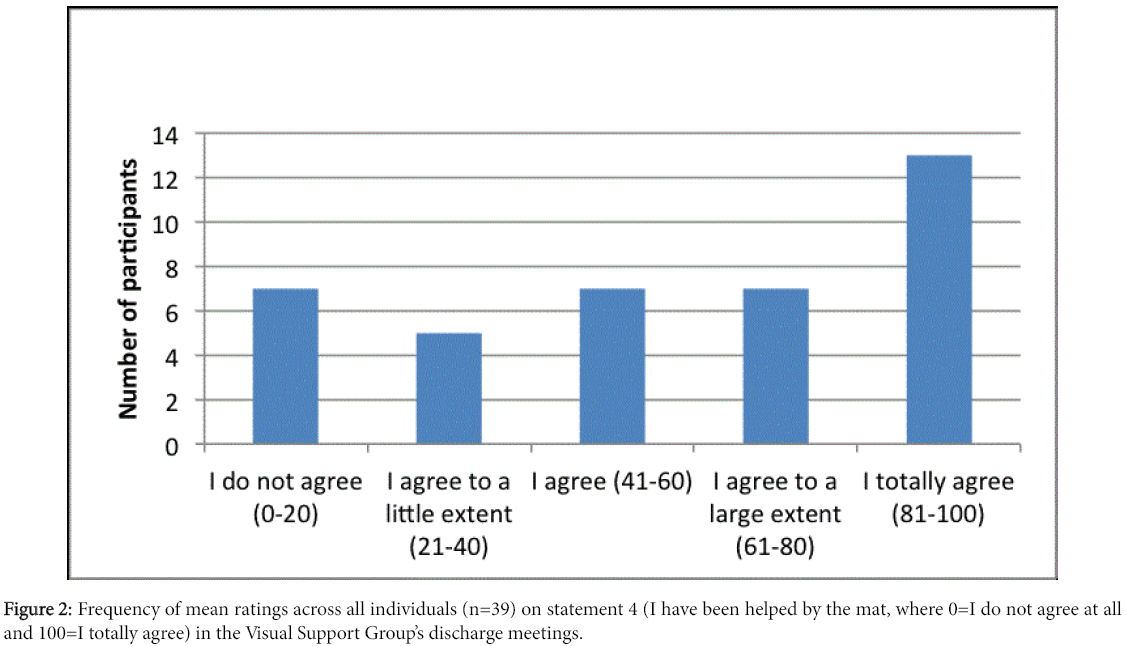
An extra statement regarding the mat was added for TMG: 4) I think the Talking Mat has helped the communication. For this statement there were 7 missing responses (of 38 ratings).
Ethical considerations
The Regional Ethics Committee in Stockholm approved the study protocol (diary number 2013/167-31/1), and the participants gave their informed consent to participate in the study. The voluntarism was stressed. Since individuals with cognitive impairment might have difficulty understanding information given to them, and may not realize the potential consequences of different choices [3], the test leader was watchful for any signs that a patient may not want to participate (signs of restlessness, fatigue, non-verbal cues etc).
Results
On average the patients talked (i.e., utilized) about 16 prepared cards along with 1 optional blank card. Abstract themes (e.g., spirit and feeling safe) were more seldom discussed than concrete (e.g., washing and going out). A majority in TMG rated in their discharge meetings that they thought the mat had been helpful; twenty-eight (of forty) ratings indicated a positive experience of TM (fourth statement); see figure 2.
Communication and participation during discharge meetings
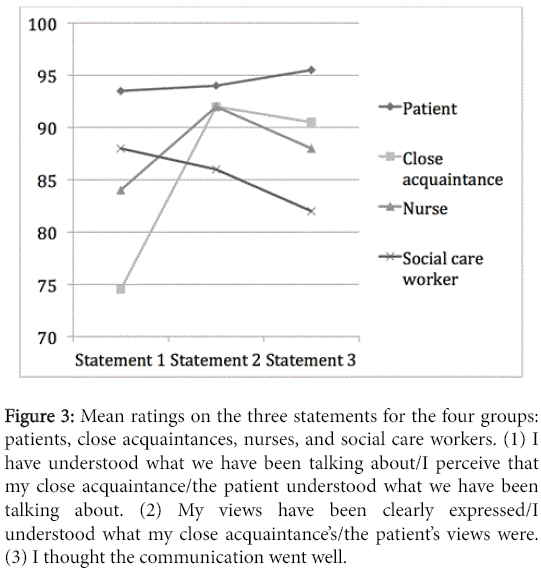
The main research question was to investigate if the four groups of persons attending discharge meetings (patients, close acquaintances, nurses, and social care workers) differed with regard to the ratings of patients’ participation and communication. Ratings on the first three statements (see Measures) were summarized as mean values. A one way (4 groups) ANOVA on the mean ratings did not reach significance (F=1.25, df=3, p>0.05, η2=0.06), although the mean values across groups varied considerably (M ± SD; 88.0 ± 15.0, 76.2 ± 20.9, 76.1 ± 25.5 and 75.0 ± 23.4; patients, close acquaintances, nurses, and social care workers; respectively). This finding indicates that the groups of persons attending the meetings did not rate the statements on patients’ communication differently.
The differences between the four groups of persons attending the discharge meeting and the three statements on VAS ratings were analyzed using a two-way ANOVA with statement as within factor and group as between factor. The main effect of statement was significant (F=3.37, df=2/58, p<0.05, η2=0.10), indicating that the statements did differ in mean level of ratings across groups. The main effect of group was not significant (p>0.05, η2=0.05), indicating that which role the person had in the discharge meeting belonged to did not statistically affect how they rated the statements. The interaction effect between group and statement was significant (F=2.44, df=6/118, p<0.05, η2=0.11), indicating that the separate groups rated each of the three statements in a different pattern. The patients rated their perceived communication and participation higher than the other groups did. The social care workers rated the patients’ communication somewhat lower than the patients themselves but their pattern of ratings was similar to that of the patients. Both close acquaintances and nurses rated statement 1 lower than patients and social care workers but rated statements 2 and 3 higher than social care workers (Figure 3). A posthoc t-test showed that the pairwise comparisons did not reach statistical significance (all p>0.1), although some differences were substantial (e.g., the difference between patients and close acquaintances on statement 1).
Figure 3: Mean ratings on the three statements for the four groups: patients, close acquaintances, nurses, and social care workers. (1) I have understood what we have been talking about/I perceive that my close acquaintance/the patient understood what we have been talking about. (2) My views have been clearly expressed/I understood what my close acquaintance’s/the patient’s views were. (3) I thought the communication went well.
Comparing communication between TMG and CG
The pilot study regarded comparing the TMG with the CG to analyze if there were any differences regarding the ratings of the patients’ communication and participation on a group level. A comparison of the patients’ communication in CG and TMG using mean VAS ratings (averages of statements 1, 2, and 3) of all persons attending the discharge meeting, showed the two groups differed significantly (t=2.10, df=62, p<0.05, Hedges’ g=0.49) according to a ttest (M ± SD; 85.2 ±1 5.4, 74.2 ± 24.3). In the CG discharge meetings persons rated on average the patients’ participation and communication as 85.2 on the 100 mm VAS, while the persons in the TMG rated on average the participation as 74.2.
Discussion and Conclusions
The aim of this study was to explore communication and the potential benefit of preparing patients with cognitive impairment for their discharge meetings utilizing TM. Ratings showed that TM was perceived as a communication facilitator during the meetings. Comparison with CG did however not show benefits for TM.
Our main finding was that ratings on the statements aggregated across the four groups of persons attending the discharge meetings (patients, close acquaintances, nurses, and social care workers) showed similar mean levels. A comparison between these groups showed that the perceived levels of communication functioning and participation differed between the different persons attending the meeting. The patients’ ratings were found to be higher compared to other groups, which might reflect a lack of insight regarding own abilities or be an expression of the patients’ state of dependency. It is interesting that the close acquaintances and nurses, who knew and had met the patients previously, showed similar patterns to each other in their ratings (Figure 2), while the social care workers differed from this. The fact that people in these two groups knew the patients may have given them a deeper understanding of their communicative skills. The statements, which aimed to capture the patients’ communicative functioning and the impact on participation (see Measures), were deliberately formulated in easy, comprehensible syntax and short sentences, with the downside being that it may have opened the door for potential bias and confounders. The number of missing responses on each of these statements (11-12 each) may also have influenced the results.
Our results further showed that TM was appreciated as a valuable tool for a majority of persons in TMG (Figure 3). In accordance with previous research, geriatric patients with cognitive impairment were able to use the TM framework, despite some patients having considerable cognitive impairment as shown by their low MMSE scores [10-16]. Abstract themes were discussed less, probably reflecting the fact that more complicated issues might exceed people with cognitive impairments’ abilities [17].
The result that TM helped communication (Figure 3) was in some way contradicted by the fact that persons in the CG rated on average the patients’ participation and communication in discharge meetings unexpectedly somewhat higher than persons in the TMG. A reason for this could be that the introduction of a communication-supporting device drew attention to the fact that communication skills might be affected, thereby stimulating awareness and critical reflection. This leads us to believe that ratings by persons attending the meeting may not be the best way to capture the patients’ actual communication and participation during discharge meetings. Recorded observations of how the completed mats were used during the meetings (e.g., through video recordings and an objective analysis of the communication) could add valuable information with which to investigate how patients are able to communicate their views and in what way it affects their participation. Another possible explanation could be that the speech and language pathologist utilizing TM with the patient was not present during the meeting. The patient may lack the ability to raise his/her views even if a prepared mat is present, as participation during a discharge meeting is not a given for any geriatric patients [6]. To ensure that the patient’s opinions are conveyed optimally in clinical practice, we suggest that the personnel (for example a nurse) who utilize the mat with the patient should have previous well knowledge of her/him and be present during the discharge meeting. The personnel can thus take an active role in promoting the patient’s views.
An important function for speech and language pathologists is to find ways of facilitating communication and decision-making in order to enhance participation and autonomy among hospitalized geriatric patients with cognitive impairment. This may not always be best accomplished by direct intervention, but by instructing other personnel regarding ways of facilitating communication. Making decisions and feeling self-empowered are important aspects of wellbeing [13-15]. Decreases in one’s abilities to understand, to express oneself, and to make well-grounded decisions occur over the progression of dementia [3]. The ability to communicate becomes more and more of a challenge, making assistance in this area all the more crucial. It is important that patients transitioning to life outside of the hospital are able to influence the outcome of that process, and the staff can have an important role in facilitating the patients’ communication skills.
Making health care decisions might be an ethical issue when involving patients with cognitive impairment. Persons attending discharge meetings rated the use of TM as facilitating communication. It is desirable to have the person preparing the mat with the patient also attending the discharge meeting, in order to help the patient reach his or her full capacity to participate.
Acknowledgement
The authors thank all participants in the study for making it possible as well as anonymous reviewers for constructive comments.
This work was supported by the Stockholm County Council [ALF Project 2013]; and Stockholm County Council fund for Care Development at the Karolinska University Hospital [2014].
References
- World Health Organization (2002) Active ageing: a policy framework. Geneva, Switzerland: World Health Organization.
- Bayles, KA, Tomoeda CK, Trosset MW (1992) Relation of linguistic communication abilities of Alzheimer's patients to stage of disease. Brain Lang 42: 454-472.
- Tallberg IM, Storemoen S, Almivist O, Erikksdotter M, Sundstrom E (2013)Investigating medical decision-making capacity in patients with cognitive impairment using a protocol based on linguistic features.Scand J Psychol 54: 386-392.
- Ekdahl AW, Hallestorm I, Andersson L, Freidrichsen M (2012) Too complex and time-consuming to fit in! Physicians' experiences of elderly patients and their participation in medical decision making: a grounded theory study. BMJ Open: 2:
- Ekdahl AW, Andersson L, Friedrichsen M (2010) "They do what they think is the best for me. "Frail elderly patients' preferences for participation in their care during hospitalization. Patient Educ Couns 80:233-240.
- Efraimsson E, Sandman PO, Hydén LC, Holritz Rasmussen B(2006) How to get one's voice heard: the problems of the discharge planning conference. J Adv Nurs 53: 646-655.
- The National Board of Health and Welfare (2007)Inventeringavutskrivningsklarapatienterochvårdplaneringisamband med utskrivning : undersökning [Overview of discharge eligible patients and discharge-related care planning. Investigation 2007]. Stockholm: Socialstyrelsen.
- Murphy J, Gray CM, Cox S (2007) Communication and dementia: Talking Mats - helping people with dementia to express theIr views. Joseph Rowntree Foundation.
- Murphy JF, (2009) Talking mats : A study of communication difficulties and the feasibility and effectiveness of a low-tech communication framework. S.l.
- Murphy J, Oliver T (2013) The use of Talking Mats to support people with dementia and their carers to make decisions together. Health Soc Care Community 21: 171-180.
- Murphy J Gary CM (2007) Using ‘Talking Mats’ to help people with dementia to communicate. Full Report, Joseph Rowntree Foundation.
- Folstein MF, Folstein SE, McHugh PR (1975) "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12: 189-198.
- The National Board of Health and Welfare (2014) Demenssjukdomarnas samhällskostnaderi Sverige 2012. Stockholm: Socialstyrelsen.
- Logsdon RG, McCurry S, Teri L (2007) Evidence-Based Interventions to Improve Quality of Life for Individuals with Dementia. Alzheimers care today. 8: 309-318.
- Savundranayagam MY, Hummert ML Montgomery RJV (2005) Investigating the Effects of Communication Problems on Caregiver Burden. S48-S55.
- Murphy J, Oliver TM, Cox S (2010) Talking Mats and involvement in decision making for people with dementia and family carers. Full Report, Joseph Rowntree Foundation.
- Emery VOB (2000) Language Impairment in Dementia of the Alzheimer Type: A Hierarchical Decline? The International Journal of Psychiatry in Medicine. 30: 145-164.
Relevant Topics
- Stuttering therapy
- Active listening
- Aphasia
- Articulation disorders:
- Autism Speech Therapy
- Bilingual Speech pathology
- Clinical Linguistics
- Communicate Speech pathology
- Interventional Speech Therapy
- Late talkers
- Medical Speech pathology
- Spectrum Pathology
- Speech and Language Disorders
- Speech and Language pathology
- Speech Impediment / speech disorder
- Speech pathology
- Speech Therapy
- Speech Therapy Exercise
- Speech Therapy for Adults
- Speech Therapy for Children
- Speech Therapy Materials
Recommended Journals
Article Tools
Article Usage
- Total views: 14986
- [From(publication date):
March-2016 - Apr 14, 2025] - Breakdown by view type
- HTML page views : 14036
- PDF downloads : 950