How CX3CR1+ Macrophages Regulate Gut Homeostasis
Received: 06-Apr-2017 / Accepted Date: 20-Jun-2017 / Published Date: 25-Jun-2017
Abstract
Colonic mucosa is a very peculiar immunological site daily exposed to a huge amount of harmless antigens. It is important for the immune system to be able to recognize this innocuous antigens from pathogens. Among all the immune cells, CX3CR1+ macrophages exploit this critical role. In this commentary on our recent publication on Immunobiology we want to highlight the crucial and unique role of these macrophages in order to maintain homeostasis and avoid the rise of aberrant inflammation and tissue damage.
Keywords: CX3CR1; Macrophages; Colonic mucosa; Colitis; Homeostasis
17291Case Report
The intestine is an exclusive tissue able to maintain balance between the immune system activation and the tolerance against the very huge amount of harmless antigens that are in contact with the intestinal lumen, including food antigens and microflora.
It is fundamental for our health that our immune system is able to respond with a robust and appropriate response to potential dangerous antigens; but the same reaction against harmless antigens, like commensal bacteria or dietary proteins, could be very dangerous and could give rise to allergies or chronic inflammation that, in the end, can lead to tissue damage or cancer development. Many immune cells participate in the maintenance of the homeostasis in gut, with the role of understanding how an antigen is a potential danger for the organism and being silenced in response to commensal bacteria and food antigens. This complex landscape includes T and B lymphocytes, natural killer cells, innate lymphoid cells, eosinophil and mononuclear phagocytes: dendritic cells and macrophages.
Among the latter, monocyte-derived macrophages, expressing the CX3CR1 receptor, constitute the most abundant population [1]. The manuscript by Marelli et al. [2], is focused on the role of CX3CR1+ macrophages in both steady state and acute colitis. In the last few years intensive research has been performed in order to clarify the role of these immune cells in the maintenance of homeostasis, but still, contrasting results have been reported regarding their role in the control of inflammatory response in the intestine [3,4]. Considering this confused landscape, our paper aimed to clarify the role of CX3CR1+ cells in the development of acute colitis. By using mice lacking the receptor (CX3CR1GFP/GFP mice) we demonstrated that the absence of CX3CR1 on gut macrophages leads to a more severe degree of DSS-induced colitis, higher colon infiltration of inflammatory macrophages and Th17 lymphocytes and higher expression of inflammatory cytokines.
Macrophages in the intestinal mucosa are considered mononuclear phagocytes that originate from a common myeloid progenitor which can differentiate also into dendritic cells [5]. In contrast to others resident macrophages, they are continuously replenished from blood stream Ly6C+ monocytes, independently from the CX3CR1 receptor [6]. This issue caused considerable misunderstanding in the past, generating the belief that these cells were dendritic cells [7,8]. However, today it is recognized that Ly6Chi monocytes are recruited in the mucosa and there, in few days, they differentiate in mature macrophages, progressively loosing Ly6C and starting to express typical markers, such as F4/80, CD64, MHCII and CX3CR1 [6]. As highlighted before, different authors investigated the role of CX3CR1+ gut macrophages with controversial outcomes.
CX3CR1+ macrophages are supposed to maintain homeostasis in the gut [9]. In accordance with this concept, our data revealed an exacerbated intestinal inflammation with a huge accumulation of macrophages in CX3CR1-KO mice. As reported also by different authors, [3,10] the natural consequence of the accumulation of macrophages is an increased production of cytokines, and hence a higher recruitment of immune cells in the colon, in particular T lymphocytes of the Th17 subset. On the contrary, other authors [4] suggested that the lack of the receptor impairs macrophages accumulation in the lamina propria. Moreover they suggested that the engagement of the receptor by its unique ligand (Fracktalkine/ CX3CL1) resulted in an intensification of iNOS production, an inflammatory enzyme. Our data, instead, clearly demonstrate that the absence of the receptor increases the level of iNOS and of many other pro-inflammatory cytokines. This is a tissue-specific competence of the intestine, being colonic resident macrophages an exemption from the rules. Indeed, in other tissues, the expression of CX3CR1 receptor is associated with a pro-inflammatory phenotype [11,12]. In support of our data it is important to underline that, in the gut, CX3CR1 macrophages are fundamental to bring antigens and present them to DC in order to establish oral tolerance. When this mechanism is missing due to the lack of the receptor, the immune system is activated and this results in an acute inflammatory response [8].
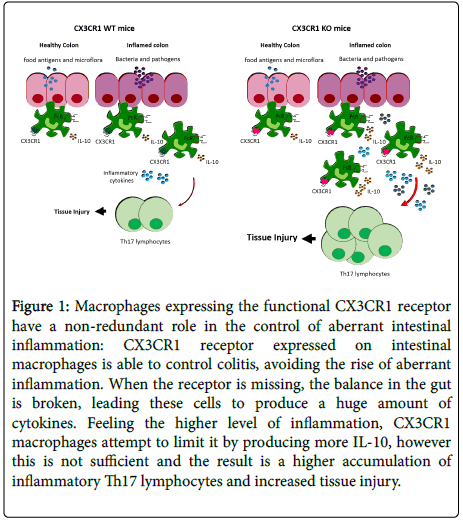
We have shown in Marelli et al. that if the CX3CR1 receptor is lacking, the ability of these cells to control inflammation is lost. Of note, CX3CR1-KO macrophages try counter-balance this aberrant situation by producing more IL-10, a major immune-suppressive and anti-inflammatory cytokine. In spite of this increase, IL-10 is not sufficient to control the inflammatory disease and mice have an exacerbated colitis (Figure 1).
Figure 1: Macrophages expressing the functional CX3CR1 receptor have a non-redundant role in the control of aberrant intestinal inflammation: CX3CR1 receptor expressed on intestinal macrophages is able to control colitis, avoiding the rise of aberrant inflammation. When the receptor is missing, the balance in the gut is broken, leading these cells to produce a huge amount of cytokines. Feeling the higher level of inflammation, CX3CR1 macrophages attempt to limit it by producing more IL-10, however this is not sufficient and the result is a higher accumulation of inflammatory Th17 lymphocytes and increased tissue injury.
Overall, with our study we wanted to propose a definitive protective and anti-inflammatory role of CX3CR1+ macrophages during the processes of acute colitis; this concept may shed light also on the role of these cells in other pathological conditions of the gut associated with persistent inflammation. Our study established that macrophages expressing the functional CX3CR1 receptor have a non-redundant role in the control of aberrant intestinal inflammation, a harmful condition that may lead to tissue injury.
References
- Zigmond E, Jung S (2013) Intestinal macrophages: well educated exceptions from the rule. Trends Immunol 34: 162-168.
- Marelli G, Belgiovine C, Mantovani A, Erreni M, Allavena P (2017) Non-redundant role of the chemokine receptor CX3CR1 in the anti-inflammatory function of gut macrophages. Immunobiology 222: 463-472.
- Medina-Contreras O, Geem D, Laur O, Williams IR, Lira SA, et al. (2011) CX3CR1 regulates intestinal macrophage homeostasis, bacterial translocation, and colitogenic Th17 responses in mice. J Clin Invest 121: 4787- 4795.
- Kostadinova FI, Baba T, Ishida Y, Kondo T, Popivanova BK, et al. (2010) Crucial involvement of the CX3CR1-CX3CL1 axis in dextran sulfate sodium-mediated acute colitis in mice. J Leukoc Biol 88: 133-143.
- Fogg DK, Sibon C, Miled C, Jung S, Aucouturier P, et al. (2006) A clonogenic bone marrow progenitor specific for macrophages and dendritic cells. Science 311: 83-87.
- Bain CC, Scott CL, Uronen-Hansson H, Gudjonsson S, Jansson O, et al. (2013) Resident and pro-inflammatory macrophages in the colon represent alternative context-dependent fates of the same Ly6Chi monocyte precursors. Mucosal Immunol 6: 498-510.
- Niess JH, Brand S, Gu X, Landsman L, Jung S, et al. (2005) CX3CR1-mediated dendritic cell access to the intestinal lumen and bacterial clearance. Science 307: 254-258.
- Mazzini E, Massimiliano L, Penna G, Rescigno M (2014)Â Oral tolerance can be established via gap junction transfer of fed antigens from CX3CR1(+) macrophages to CD103(+) dendritic cells. Immunity 40: 248-61.
- Zigmond E, Bernshtein B, Friedlander G, Walker CR, Yona S, et al. (2014) Macrophage-restricted interleukin-10 receptor deficiency, but not IL-10 deficiency, causes severe spontaneous colitis. Immunity 40: 720-733.
- Kurmaeva E, Bhattacharya D, Goodman W, Omenetti S, Merendino A, et al. (2014) Immunosuppressive monocytes: possible homeostatic mechanism to restrain chronic intestinal inflammation. J Leukoc Biol 96: 377-389.
- Li L, Huang L, Sung SS, Vergis AL, Rosin DL, et al. (2008) The chemokine receptors CCR2 and CX3CR1 mediate monocyte/macrophage trafficking in kidney ischemia-reperfusion injury. Kidney Int 74: 1526-1537.
- Mionnet C, Buatois V, Kanda A, Milcent V, Fleury S, et al. (2010) CX3CR1 is required for airway inflammation by promoting T helper cell survival and maintenance in inflamed lung. Nat Med 16: 1305-1312.
Citation: Marelli G, Allavena P (2017) How CX3CR1+ Macrophages Regulate Gut Homeostasis. J Mucosal Immunol Res 1:102.
Copyright: ©2017 Marelli G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 4694
- [From(publication date): 0-2017 - Apr 06, 2025]
- Breakdown by view type
- HTML page views: 3689
- PDF downloads: 1005