Research Article Open Access
Hospital Admissions of Cancer Patients in Brazil: Analysis of Palliative Care Needs
Cledy Eliana dos Santos1*, José Manuel Peixoto Caldas2, José Américo Serafim3, Newton Barros4 and Altamiro da Costa Pereira51Community Health Service and Palliative Care Service, Hospital Nossa Senhora da Conceição – GHC (Conceição Hospital Group), Brazil
2Department of Education and Medical Simulation, University of Porto- Portugal; Visiting Professor of Post-Graduate Program in Collective Health from UNIFOR, Brazil
3Information Technology, Department of the Brazilian Health System-SUS (DATASUS), Ministry of Health, Brazil
4Palliative Care Service, Hospital Nossa Senhora da Conceição – GHC, Brazil
5Director of the CINTESIS–FMUP, Brazil
- *Corresponding Author:
- Cledy Eliana dos Santos
Family and Palliative Care M.D., Conceição Hospital Group
Pain and Palliative Care Service, Francisco Trein, 596, Cristo Redentor
Porto Alegre, RS 91350200, Brazil
Tel: +555133572140
Fax: +555132551744
E-mail: cledy.eliana@gmail.com
Received date: April 19, 2016; Accepted date: May 23, 2016; Published date: May 27, 2016
Citation: Santos CD, Caldas JMP, Serafim JA, Barros N, Pereira AC (2016) Hospital Admissions of Cancer Patients in Brazil: Analysis of Palliative Care Needs. J Palliat Care Med 6:263. doi:10.4172/2165-7386.1000263
Copyright: © 2016 Santos CD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Background: Cancer figures among the leading causes of morbidity and mortality in Brazil, with approximately 576,000 new cases and around 200,000 cancer-related deaths in 2013. According to the Brazilian National Oncological Policy, cancer control must include health promotion, prevention, diagnosis, treatment, rehabilitation, and palliative care, following the Brazilian Health System (SUS) guiding principles of Universality, Equity, and Integrality of health care. Aims: 1) Outline the hospital admissions of patients for the treatment of clinical cancer intercurrences in the Brazilian Health System (SUS) between 2008-2013; 2) Estimate the number of cancer patients with palliative care needs. Methods: Quantitative methods were employed, through the analysis of descriptive, exploratory, retrospective, and observational studies of hospitalized cancer patients. Data was collected from the Hospital Information System of Brazilian Health System (SIH/SUS) in the database of the Health Information Department (DATASUS). Results: Between 2008 and 2013, there were almost 4 million hospitalizations (3,701,409) of patients with cancer in Brazil. Of all the hospital admissions of cancer patients, 978,322 (26.4%) were related to clinical intercurrences (complications) of the disease and/or for treatment. In the same period, approximately 7 million deaths were reported to the Brazilian Mortality Information System (SIM), 15.9% (1,091,837) of cancer. The average rate of hospital mortality of clinical cancer intercurrences was three times (21.4%) higher than the mortality of patients admitted for treatment of clinical cancer in general (7.7%). The hospital length of stay (LOS) of general cancer patients was 5.7 days against 7.9 days of clinical cancer intercurrence patients. It was verified that approximately 90% of those admissions registered in the procedure "Treatment of Clinical Intercurrences of Cancer Patient” in Brazil were related to palliative care of terminally ill patients. Conclusion: The analysis of the morbidity and mortality profile of cancer patients suggests that palliative care services should be considered as criteria for the treatment of clinical cancer intercurrences. Further study of the hospital procedure “Treatment of clinical complications of cancer patient” should be considered as a parameter for scaling palliative care services in Brazil.
Keywords
Cancer; Palliative care; Non-communicable diseases; Clinical cancer intercurrences; Hospital admissions of cancer patients.
Introduction
Brazil is a country with a rapidly aging population. With the improvement of living conditions, life expectancy increased 25.4 years between 1960 and 2010, rising from 48 to 73.4 years old. It is estimated that by 2050 this indicator will increase to 81.29 years. This process followed a significant reduction in mortality due to the control of infectious-contagious diseases and the decrease of cardiovascular conditions [1,2].
The report “Preventing chronic diseases: a vital investment”, from the Pan American Health Organization (PAHO), expects that by 2020, 32 million elderly Brazilians will die of cancer, against 840 thousand deaths from the same disease in Latin America and the Caribbean. PAHO adverts that palliative care is not properly valued in the therapeutic process and that it should be part of the treatment for the initial diagnostic stage [3-5].
Most individuals with cancer only seek the public health system in the advanced stages of the disease. It becomes, therefore, imperative to improve the quality of care, facilitate access to palliative care, and promote equity in services [6,7].
It has been a difficult task to assess the necessary resources and to define the specific criteria to structure and adapt palliative care services in countries whose health policies do not anticipate this approach [8-13]. Such is the case of Brazil. The task is even more complicated when we consider the criteria used to understand the differences between curative and palliative attention.
The chronic non-communicable diseases (NCDs) were the cause of approximately 74% deaths. This obstacle presents a new challenge for health administrators. The impact is stronger if we consider the life quality of the affected individuals, and the greater chance of premature death, besides the adverse economic effects for families, communities and society [14].
The four most prevalent chronic diseases highlighted by World Health Organization (WHO) [15] accounted for 52% of deaths in the period between 2008 and 2013. Cardiovascular diseases account for most NCD deaths, followed by cancer, diabetes and respiratory diseases.
Within the framework of chronic diseases, cancer deserves a differentiated approach, for its high prevalence, consumption of large amounts of financial resources, and its significant institutional and social burden [16-18].
According to the Brazilian National Oncological Care (Decree GM/MS 2.439/2005) cancer control, like any other chronic disease, must include all possible actions available in the Brazilian Health System (SUS): health promotion, prevention, diagnosis, treatment, rehabilitation and palliative care [19]. It is necessary to improve the quality of life, relieve physical suffering, cater for the psychological, spiritual and social needs of people with severe and advanced diseases, as well as to provide support to families and caregivers. It is indispensable to consider the existing models of health care if we want to achieve these goals. The inclusion or expansion of palliative attention meets the size, nature and severity of the needs of cancer patients.
The incidence of cancer in Brazil, as in the rest of the world, has grown, accompanying the aging, and the increased life expectancy of the population. In the period spanning from 2008 to 2013, the incidence of cancer increased by 11%. This increase was the direct result of significant global transformations in the last decades, such as the accelerated urbanization, new lifestyles, and new consumption patterns, changing the situation of people’s health [16-18].
In recent years, we have seen an increased number of hospital admissions of patients presenting late diagnosis of cancer, adding to pre-existing comorbidities. These cases show the need for basic care to prevent or treat complications related to cancer.
The complications of cancer may be related to the itself, systemic manifestations of the disease or treatment side effects [20].
The expression clinical cancer intercurrence is related to an acute complication of the disease due to cancer itself or its treatment, requiring hospitalization in specialized, general or in day hospitals [21].
From the retrospective analysis of hospital admissions data gathered from the Hospital Information System of Brazilian Health System (SIH-SUS), it was verified that approximately 90% of those admissions registered in the procedure "Treatment of Clinical Intercurrences of Cancer Patient” in Brazil were related to palliative care of terminally ill patients [22].
Parameters for healthcare coverage, planning, and control as well as the evaluation of palliative care requirements do not exist in Brazil. Until now, we have estimated these needs based on international practices, such as the one employed by the United Kingdom National Health System which offers fifty beds for every million inhabitants. In the Brazilian situation, there is a need for 9,000 hospital beds for palliative care patients, and 600 to 900 units for hospitalization [23].
The World Health Organization (WHO) consider that for every 1 million people, 1,000 require palliative care every year. Considering the Brazil’s population of 200 million, the situation becomes even more delicate, requiring necessary services to meet its needs every year [12,23-27].
This study investigates the distribution of hospital admissions for the treatment of clinical intercurrences of cancer of patients registered in the Brazilian Health System (SUS) between the years of 2008 and 2013.
Methods
Descriptive, exploratory, retrospective, and observational studies of hospitalized cancer patients were analyzed for the purpose of this research study, which employs a quantitative methods approach.
Data was obtained from the database of the Health Information Department of Brazilian Health System (DATASUS), collected from the Hospital Information System of Brazilian Health System (SIH/ SUS).
The entire process of the Hospital Information System of Brazilian Health System (SIH/SUS) is based on the Hospital Admission Authorization (AIH), which includes patient and hospitalization data, the description of hospital morbidity and mortality; the benchmarking of hospital assistance; epidemiological surveillance; as well as the validation of other health information systems [28-30].
With the advantage of providing diagnostic, demographic, and geographic information for each patient admitted to hospitals, the Hospital Admissions Authorization (AIH) forms, have expanded the availability of epidemiological data.
The systems commonly used for gathering data are the Information System on Live Births (SINASC), Reportable Diseases System (SINAN), Mortality Information System (SIM), Primary Care System (SIAB), Outpatient Information System of Brazilian Health System (SIA-SUS), and Hospital Information System of Brazilian Health System (SIH-SUS).
Incidence data on cancer was obtained from population-based cancer registers of the National Cancer Institute [31].
Hospital morbidity data was collected from the Hospital Information System of Brazilian Health System (SIH/SUS) in the database of the Health Informatics Department (DATASUS) from the Ministry of Health [32].
Mortality data (2008-2013) was gathered from the mortality information system database of DATASUS [33].
Data from 3.7 million registered hospitalizations of cancer patients, spanning from 2008 to 2013, was collected and processed through a system (syntaxes) using Tabwin and SPSS programs [34,35].
Results
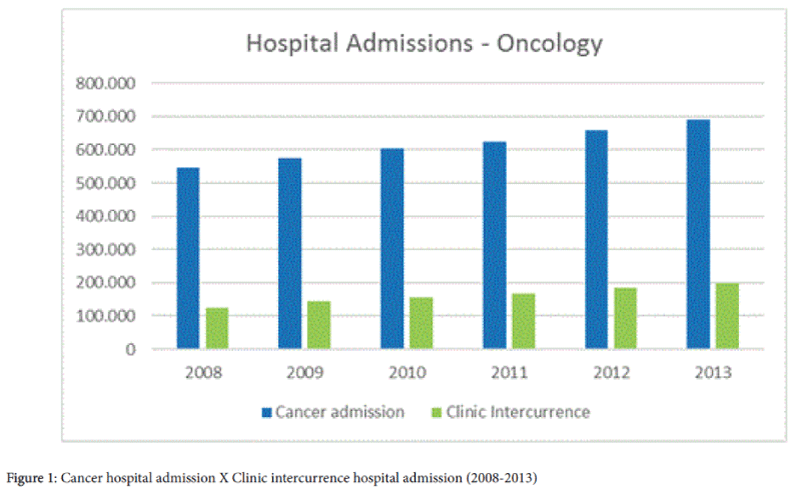
From 2008 to 2013, the Brazilian Health System recorded 66.8 million hospitalizations, including all age groups. Of the total admissions registered in the period, there were 3.7 million admissions of cancer patients to Brazilian public hospitals. In the same period, we observed a variation of 4.2% in the total number of SUS hospitalizations. There was an increase of 26.7% in hospitalizations related to cancer as a whole and 48.1% of hospital admissions for clinical cancer intercurrence (Table 1).
| Year | Hospital admission (all diseases) - Brazil | Cancer hospital admission | Cancer Clinic Intercurrence – hospital admission | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Freq | % | Deaths | % | Freq | % | Deaths | % | |
| 2008 | 10,743,603 | 545,863 | 5.1% | 39,168 | 7.2% | 125,605 | 23.01% | 27,911 | 21.7% |
| 2009 | 11,128,809 | 575,371 | 5.2% | 44,129 | 7.7% | 144,302 | 25.08% | 32,450 | 22.4% |
| 2010 | 11,357,965 | 604,809 | 5.3% | 46,937 | 7.8% | 155,512 | 25.71% | 33,991 | 21.7% |
| 2011 | 11,281,571 | 624,035 | 5.5% | 49,026 | 7.9% | 167,564 | 26.85% | 35,991 | 21.3% |
| 2012 | 11,092,589 | 659,788 | 5.9% | 51,984 | 7.9% | 185,406 | 28.10% | 38,774 | 20.8% |
| 2013 | 11,197,160 | 691,543 | 6.2% | 55,340 | 8.0% | 199,933 | 28.91% | 37,936 | 20.7% |
| Total | 66,801,697 | 3,701,409 | 5.5% | 286,584 | 7.7% | 978,322 | 26.43% | 207,053 | 21.4% |
Table 1: Hospital admissions in Brazil (2008-2013).
Of the total number of hospital admission of cancer patients recorded between 2008 and 2013 in the Hospital Information System of Brazilian Health System (SIH-SUS), 26.1% (978,322) were admitted for treatment of clinical intercurrence of cancer (Figure 1).
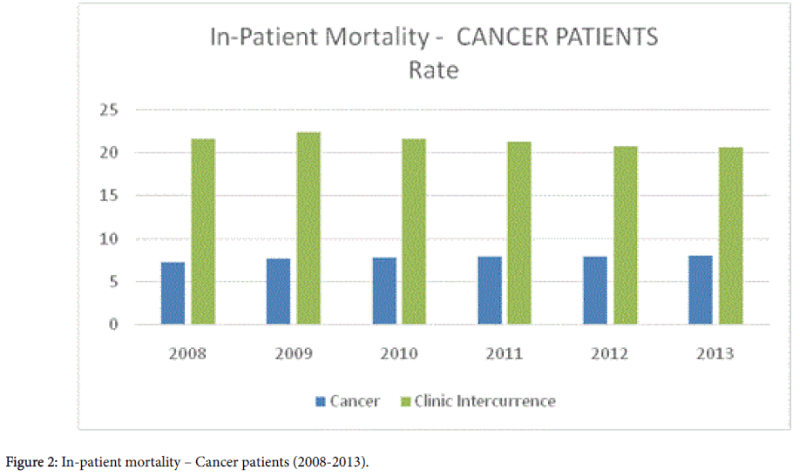
Hospital mortality of cancer patients, as seen in Table 1, was analyzed in terms of frequency and rate. In the period of 2008 and 2013, of the total number of cancer patients admitted to hospitals, the mortality rate was 7.7 for general cancer and almost three times higher for patients admitted for treatment of clinical intercurrence (21.4) (Figure 2).
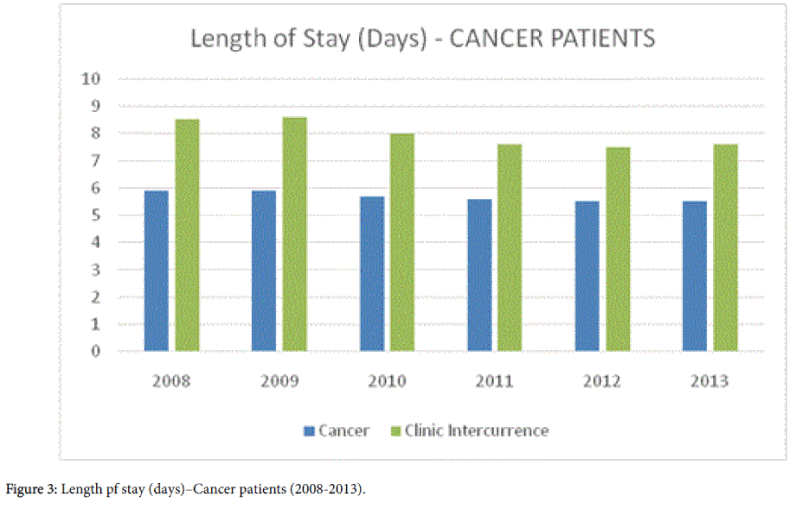
The length of stay (LOS), as seen in Table 2, of cancer patients as a whole was 5.7 days, against 7.9 days of hospitalization for patients admitted for treatment of clinical cancer intercurrences (Figure 3).
| Length Of Stay (Days)-Cancer Patients | ||
|---|---|---|
| Year | Cancer | Clinic intercurrence |
| 2008 | 5.9 | 8.5 |
| 2009 | 5.9 | 8.6 |
| 2010 | 5.7 | 8.0 |
| 2011 | 5.6 | 7.6 |
| 2012 | 5.5 | 7.5 |
| 2013 | 5.5 | 7.6 |
| Total | 5.7 | 7.9 |
Table 2: Hospitalization of Cancer Patients–Length of Stay-Days(LOS).
Discussion
The hospital admission data shows that each year we have an average of 146,748 cancer patients requiring palliative care. Despite the existing Primary Care Program (Family Health since 1996), the National Policy on Pain and Palliative Care, launched in 2002, and the 2005 National Cancer Policy, which makes some reference to palliative care, Brazil does not have yet effective strategies to integrate palliative care into the Brazilian Health System (SUS) network [36].
To determine the palliative care needs, the structure of services and the qualified staff are significant challenges for the Brazilian public health system, making it difficult to assess the health services, including the number of available hospital beds.
Even with the implementation of international strategies to scale the needs for palliative care in Brazil, we are far from achieving the same organization and structure of countries with a long tradition in this health care area. According to the National Academy of Palliative Care (ANCP), 9,500 hospital beds for palliative care, and between 663 to 950 inpatient units, each one with 10 to 15 beds are needed. Currently, there are around 100 palliative care services in Brazil [23].
This study seeks to improve our understanding of how hospital admission and discharge data can be used to identify cancer patients in need of palliative care, and to propose parameters fitting our country’s dimension and regional diversity.
The appropriate use of Brazil’s health information systems allows us to learn and evaluate the process of health management, the planning of actions, the training of health professionals, as well as to assess health services organizations.
As it contains demographic, morbidity, mortality and financial data, the Hospital Information System of Brazilian Health System (SIH/SUS) has been increasingly exploited by health professionals, mainly due to its agility and access facility.
Even though the use of inpatient data was aimed at the provision and control of hospital spending, it is the only inpatient data source for most Brazilian states and municipalities.
Considering Brazil’s territorial and population dimensions, it is necessary to define criteria of health coverage to people in need of palliative care.
The analysis of cancer hospital admission and discharge data can assist policy makers and researchers to understand the amount and nature of palliative care needs in the Brazilian health care sector.
Conclusion
At present the quality of the final phase of life is an important issue for society, and its relevance has made that approach as a public health problem. In the last century the improvement in the determinants of health has resulted in a remarkable decrease in mortality rates, and now death occurs at later ages, frequently after long-term illness and a prolonged final phase technological advances. The quality of care at this stage is considered a subject worthy of study and intervention in public health because it shares the three criteria set priorities in public health, magnitude, high impact and potential to prevent suffering associated with the disease [37].
Further study of the hospital procedure “Treatment of clinical complications of cancer patient” should be considered as a parameter for scaling palliative care services in Brazil.
The analysis of the population morbidity and mortality profiles is necessary to the establishment of possible parameters to be employed for the assistance in palliative care such as hospital admissions for the treatment of clinical intercurrences in cancer patients [22].
In addition to hospital beds and palliative care teams, there is a need for out-patient treatment structures such as hospices and home care services as part of a national policy for the care of clinical cancer intercurrence patients and their families.
Regarding the health system response to the continuity of care given at the end of life it is essential to adopt new paradigms and models of care that understand the importance of palliative care and promote a favorable attitude towards them [38].
References
- Osvaldo Cruz Foundation ( 2012) Health in Brazil in 2030 : guidelines for the strategic exploration of the Brazilian health system. Fiocruz, Rio de Janeiro, Brazil .
- Brazilian Institute of Geography and Statistics (2010 ) Brazil: Tábua full of Mortalidade - 2010. IBGE.
- World Health Organization (2011) Noncommunicable diseases country profiles 2011. WHO, Geneve, Switzerland.
- World Health Organization (2005) Preventing chronic diseases: a vital investment: WHO global report. WHO, Geneva, Switzerland.
- Pan American Health Organization (2007) Regional strategy and plan of action on an integrated approach to the prevention and control of chronic diseases, including diet, physical activity, and health. PAHO, Washington, DC.
- Santos CE, Mattos LF (2011) palliative care and general practitioner . In: Santana F, editor. Palliative care: guidelines, humanization and relief of symptoms pp: 17-24.
- Sinsuwan W, Pairojkul S, Gomutbutra P, Kongkum K, Kosuwon W (2016) A Retrospective, Single Center, Observational Study, Comparing the Direct Cost of End-Of-Life Care Patients with Advanced Cancer Care: Palliative Care versus Usual Care. J Palliat Care Med 6: 243.
- Figueiredo TA (2006) Reflections on palliative care in Brazil. Prat Hosp 47: 36-40.
- Ling J (2010) Ranking palliative and end-of-life care. Int J PalliatNurs 16: 367.
- Wright M, Wood J, Lynch T, Clark D (2006) Mapping levels of palliative care development: a global view. University of Lancaster, Lancaster.
- Shetty P (2010) The parlous state of palliative care in the developing world. Lancet 376: 1453-1454.
- Gomez -Batiste X , Porta -Sales J, Tuca A, Stjernsward J (2005 ) Organization cuidadospaliativos services and programs.
- Twycross R (2003) Palliative care (2nd ed) Climepsi, Lisboa.
- Ministry of Health (2005) Monitoring, control and prevention of chronic noncommunicable diseases: NCDs in the context of the Single System of Brazilian health.
- De Lima L, Wenk R, Krakauer E, Ferris F, Bennett M, et al. (2013) Global framework for noncommunicable diseases: how can we monitor palliative care? J Palliat Med 16: 226-229.
- World Health Organization (2013) Health topics: chronic diseases. WHO, Geneva.
- Pan American Health Organization (2014) Plan of action for the prevention and control of noncommunicable diseases in the Americas: 2013-2019.
- World Health Organization (2014) Global status report on noncommunicable diseases. WHO, Geneva.
- Ministry of Health (2005) Ordinance GM.
- Lorite JCP (2009) Handling serious complications in cancer patients. Service of Obstetrics and Gynecology, University Hospital Virgen de las Nieves, Granada .
- Ministry of Health (2013 ) Technical bases Oncology Manual.
- Ministry of Health (2015 ) Technical bases Oncology Manual - SIA / SUS - Outpatient Information System.
- Maciel MGS (2009 ) Organization of palliative care services . In: National Palliative Care Academy. Palliative Care Manual pp: 72-85.
- Stjernswärd J, Foley KM, Ferris FD (2007) The public health strategy for palliative care. J Pain Symptom Manage 33: 486-493.
- McNamara B, Rosenwax LK, Holman CD (2006) A method for defining and estimating the palliative care population. J Pain Symptom Manage 32: 5-12.
- Bittencourt SA, Camacho LA, Leal Mdo C (2006) [Hospital Information Systems and their application in public health]. Cad SaudePublica 22: 19-30.
- World Health Organization (2007) Cancer control: knowledge into action: WHO guide for effective programmes: module 5. WHO, Geneva.
- Amaral TCL (2002) Mortalidadehospitalarnarede SUS: espelho dos óbitosocorridosnapopulaçãobrasileira? [thesis]. Universidade do Estado do Rio de Janeiro, Rio de Janeiro, Brazil.
- Sanches KRB, Camargo Junior KR, Coeli CM, Smudge AM (2003 ) System health information. Epidemiology pp: 337-359.
- National Cancer Institute José Alencar Gomes da Silva (2016 ) Cancer Statistics . INCA , Brasilia, DF , Brazil.
- http://www2.datasus.gov.br/DATASUS/index.php?area=02.
- Brazil. Ministry of Health (2013) SIHSUS : hospital information systems. DATASUS, Brasília, DF, Brazil.
- Maciel MGS, Rodrigues LF, Naylor C, Bettega R, Barbosa SM, et al. (2006) Quality criteria for palliative care in Brazil. Diagraphic, Rio de Janeiro, Brazil.
- Gragnolati M, Lindelow M, Couttolenc B (2013) Twenty years of health system reform in Brazil: an assessment of the Sistema Único de Saúde. The World Bank 1: 786.
- InstitutoBrasileiro de Geografia e Estatística (2016) Sistema de informações de mortalidade (SIM). IBGE, Rio de Janeiro.
- Floriani CA (2008) Palliative care in Brazil: a challenge to the health care system. Palliative Care Res Treat 2: 19-24.
- Rao JK, Anderson LA, Smith SM (2002) End of life is a public health issue. Am J Prev Med 23: 215-220.
- Dunlop R (2001) Specialist palliative care and non-malignant diseases. In: Addington-Hall J, Higginson I. Palliative care for non-cancer patients (chapter 15). Oxford University Press, Oxford.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 11378
- [From(publication date):
May-2016 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 10491
- PDF downloads : 887