HIV Positive Breast-Feeding MothersâCompliance with the Ministry of Health Recommended Infant and Young Child Feeding Options in Mukono District, Uganda
Received: 30-Jun-2022 / Manuscript No. JIDT-22-68113 / Editor assigned: 04-Jul-2022 / PreQC No. JIDT-22-68113 (PQ) / Reviewed: 19-Jul-2022 / QC No. JIDT-22-68113 / Revised: 26-Jul-2022 / Manuscript No. JIDT-22-68113 (R) / Published Date: 03-Aug-2022
Abstract
Background: Mother To Child Transmission (MTCT) of HIV is a threat in resource limited countries like Uganda where breastfeeding is the largest source of HIV transmission in children below the age of 5 years. The study was done to assess the compliance of HIV positive breast-feeding mothers to the Ministry of Health (MoH) recommended Infant and Young Child Feeding (IYCF) options to prevent MTCT of HIV in Mukono district.
Methodology: This study enrolled a total of 380 HIV positive mothers of age 17 to 44 years with infants aged four years and below attending Naggalama hospital, Mukono COU hospital, and Mukono Municipality health centre IV and Kojja health centre IV.
Results: The results of the study revealed that 62.11% of the respondents complied with the recommended MoH IYCF options while the rest did not. 25.69% mothers had HIV positive children. Mothers who had babies aged between 13-24 months and mothers with secondary education were 2.55 and 2.29 times respectively more likely to comply with IYCF options. Mothers who practiced mixed feeding after 6 months; exclusive replacement feeding after 6 months and having HIV positive children were 0.002; 0.02 and 0.13 times respectively less likely to comply with IYCF options.
Conclusion: Age of child and education of the HIV positive mother, the feed type practiced by the mother after six months and the HIV test result of children were all found to be predictors of mothers’ compliance with the recommended IYCF options.
Keywords: Mother to child transmission; HIV; Uganda
Introduction
The Human Immunodeficiency Virus (HIV) pandemic is one of the most serious health crises the world faces today. Globally, 1.4 million pregnant women are living with HIV in low and middle income countries [1,2]. Women currently represent the population with the fastest increase in HIV infection rates; in the hardest hit countries of Sub-Saharan Africa, more than 60% of all new HIV infections are occurring in women, infants, and young children. 330,000 children were infected in 2011 worldwide [3]. Most children living with HIV acquire the infection through Mother-To-Child Transmission (MTCT), which can occur during pregnancy, labour and delivery or during breastfeeding.
The risk of HIV transmission through breastfeeding poses a dilemma for infant feeding, particularly in a developing country like Uganda [4,5], where the HIV infection prevalence of 7.3% remains a public health concern, and where breastfeeding is the norm and is critical for child survival. Balancing this risk of infants acquiring HIV through breast milk with the higher risk of death from malnutrition, diarrhea and pneumonia among non-breastfed infants is a challenge [6]. Protecting the infant from the risk of death from these causes is as important as avoiding HIV transmission through breastfeeding. Replacement feeding unquestionably prevents all postnatal transmission but has been associated with increased risk of death from other causes.
The recognition of this challenge at global level led to the consultative meeting which was held in October 2006 by the World Health Organization [7] in order to review the substantial body of new evidence and experience that has been accumulating regarding Prevention of Mother to Child Transmission (PMTCT) of HIV and infant feeding [8]. At the national level, efforts have been directed to the promotion, protection and support of optimal IYCF, spearheaded by the Ministry of Health (MoH) in collaboration with its partners and stakeholders [9,10]. These programs have been shown to be feasible, acceptable, and cost-effective. However, they have not been implemented widely in resource-constrained settings and in particular, the provision of IYCF counseling, support, and follow up for HIV positive mothers.
The study was done to assess the compliance of HIV positive breast- feeding mothers to the MoH recommended infant and young child feeding options to prevent Mother to Child Transmission of HIV in Mukono district hospitals and health centre IVs. The study was done with specific focus on: the knowledge of HIV positive breast feeding mothers as regards the MoH recommended IYCF options; the counseling done on IYCF options to HIV positive breast feeding mothers; the capacity of the PMTCT facilities in hospitals and health centre IVs of Mukono district in the provision of the MoH recommended IYCF services, and the IYCF practices by HIV positive breast feeding mothers.
Methodology
This was a cross-sectional descriptive study combining quantitative and qualitative methods. This study enrolled a total of 380 HIV positive mothers of reproductive age 17 to 44 years with infants aged four years and below attending hospitals of Mukono district and the two health centre IVs found in Mukono district where PMTCT services were being provided. These were Naggalama hospital, Mukono COU hospital, Mukono Municipality health centre IV and Kojja health centre IV. Information was collected from the mothers using a standard pre-tested semi-structured questionnaire alongside Focus Group Discussions (FGDs), and Key informant interviews.
Data analysis
Quantitative data was analyzed in Stata 10 while for qualitative data, Content analysis or analysis by theme was used as the method of analysis as well as the use of quotes in some instances. For univariate analysis, all independent variables and the outcome variable were analyzed on their own. Results obtained were presented in form of frequency tables computing means and medians for continuous data. For Bivariate analysis each independent variable was analyzed against the outcome. The data on the variable was tested for statistical significance between the dependent and the independent variables in question. In multivariate analysis, basing on bivariate analysis, all the variables that had a P value (p < 0.05) were considered for multivariate logistic regression models and stepwise elimination method was used to remove all the non-significant variables with p >0.05.
Ethical considerations
The proposal for this study was submitted for review and clearance to the International Health Sciences University Research and Ethics committee. Permission to carry out the study in the Health facilities was sought from the Chief Administrative Officer (CAO) for Mukono district and the District Health officer (DHO) accompanied by an introduction letter from the School of Health Sciences Research regulation authorities. Informed consent was sought from health officers in charge of these health facilities and the mothers before any enrolment and data collection was done. This study ensured no risk to the human subjects participating in the study.
Results
This section highlights the findings, analysis, and interpretation of the study results by objective at univariate, bi-variate, and multi-variate levels for all the variables. The results have been presented in form of tables, charts, and graphs. Inferential statistics, statistical significance between dependent and independent variables was established using binary logistic regression in bivariate analysis and multivariate analysis to obtain odds ratios, confidence intervals and p-values to establish by objective the association between each of the variables and the HIV positive mother’s compliance to the recommended IYCF options in Mukono district. In this study, we had a response rate of 99.7%, where we left out the responses of one mother who was realised later that had mental challenges, which may have influenced her responses.
Socio-demographic characteristics of the respondents
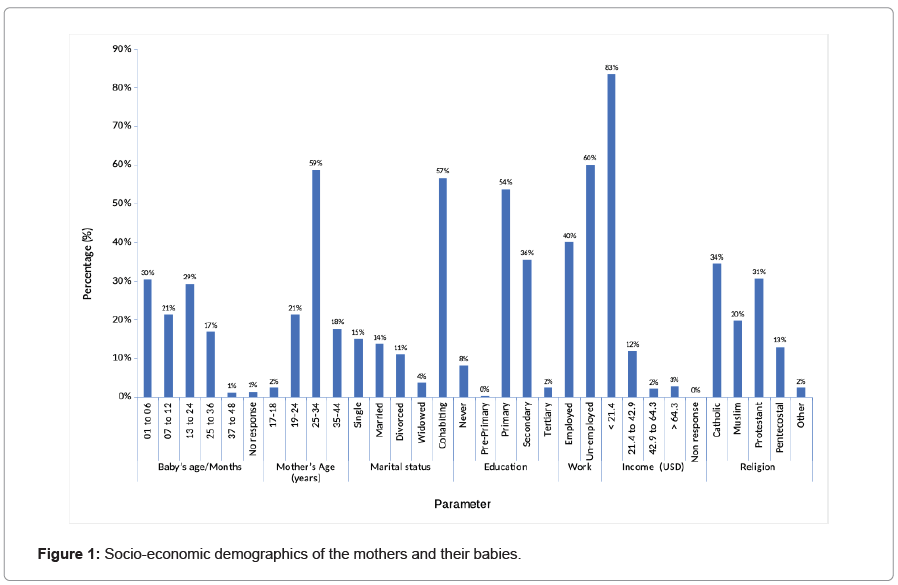
Figure 1 indicates that 30.26% of the infants were aged 1-6 months while 1.05% was of ages (37-48 months). Secondly 58.68% of the mothers were aged 25-34 years while only 2.37% were of ages (13-18) years. Out of the 380 total numbers of women, 56.58% were cohabiting, 15.00% were single, 13.68% were married, and 11.05% were divorced or separated while only 3.68% were widowed. Of the respondents, only 0.26% had attended pre-primary school, 53% had attended primary school, 36% had attended secondary, while 2.37% had attended tertiary. However, 8% had never attended school at all. Of the respondents, 60 % were unemployed. 83.42% were earning less than 75, 000/=ugx. The Catholics accounted for 34.47% while only 2.37% were seventh day Adventist.
At bivariate analysis (Table 1), baby’s age was found to be a significant influencing factor of compliance to IYCF options and specifically mothers with babies aged 13 to 24 months being 0.39 times less likely to comply to IYCF options (C.I, 0.22-0.68, p=0.001) while other age categories showed no statistical significance.
| Variable | Compliance | Non-Compliance | OR | 95% CI | p-value | ||
|---|---|---|---|---|---|---|---|
| N=236 | % | N=144 | % | ||||
| Baby’s Age/Months | |||||||
| 1-6 | 84 | 73.04 | 31 | 26.96 | 0 | Reference | 0000 |
| 7-12 | 55 | 67.90 | 26 | 32.10 | 0.78 | 0.42-1.45 | 0.435 |
| 13-24 | 57 | 51.35 | 54 | 48.65 | 0.39 | 0.22-0.68 | 0.001* |
| 25-36 | 39 | 56.52 | 30 | 43.48 | 0.48 | 0.26-0.90 | 0.022* |
| 37-48 | 1 | 25.00 | 3 | 75.00 | 0.12 | 0.01-1.23 | 0.074 |
| Mother’s Age | |||||||
| 13-18 | 6 | 66.67 | 3 | 33.33 | 0 | Reference | 0000 |
| 18-24 | 49 | 60.49 | 32 | 39.51 | 0.77 | 0.18-3.28 | 0.719 |
| 25-34 | 144 | 64.57 | 79 | 35.43 | 0.91 | 0.22-3.74 | 0.898 |
| 35-44 | 37 | 55.22 | 30 | 44.78 | 0.62 | 0.14-2.67 | 0.518 |
| Marital status | |||||||
| Single | 32 | 56.14 | 25 | 43.86 | 0 | Reference | 0 |
| Married | 31 | 59.62 | 21 | 40.38 | 1.15 | 0.54-2.47 | 0.714 |
| Divorced/Separated | 28 | 66.67 | 14 | 33.33 | 1.56 | 0.68-3.57 | 0.291 |
| Widowed | 6 | 42.86 | 8 | 57.14 | 0.59 | 0.18-1.91 | 0.375 |
| Cohabiting | 139 | 64.65 | 76 | 35.35 | 1.43 | 0.78-2.58 | 0.238 |
| Highest Education level attained | |||||||
| Never | 16 | 51.61 | 15 | 48.39 | 0 | Reference | 0 |
| Pre-Primary | 0 | 0 | 1 | 100.00 | 0 | 0 | 0 |
| Primary | 120 | 58.82 | 84 | 41.18 | 1.34 | 0.63-2.86 | 0.45 |
| Secondary | 96 | 71.11 | 39 | 28.89 | 2.31 | 1.04-5.12 | 0.04* |
| Tertiary | 4 | 44.44 | 5 | 55.56 | 0.75 | 0.17-3.33 | 0.705 |
| Employment Status of mother | |||||||
| Employed | 96 | 62.67 | 56 | 37.33 | 0 | Reference | 0 |
| Un-employed | 140 | 61.40 | 88 | 38.6 | 0.95 | 0.62-1.45 | 1.45 |
| Average Income of mother | |||||||
| < 75,000/= | 193 | 60.88 | 124 | 39.12 | 0 | Reference | 0 |
| 75,001 to 150,000/= | 33 | 73.33 | 12 | 26.67 | 1.77 | 0.88-3.55 | 0.110 |
| 150,001 to 225,000/= | 4 | 50.00 | 4 | 50.00 | 0.64 | 0.16-2.62 | 0.537 |
| > 225,000/= | 6 | 60.00 | 4 | 40.00 | 0.96 | 0.27-3.48 | 0.955 |
| Religion of mother | |||||||
| Catholic | 76 | 58.02 | 55 | 41.98 | 0 | Reference | 0 |
| Muslim | 48 | 64.00 | 27 | 36.00 | 1.286 | 0.72-2.31 | 0.399 |
| Protestant | 77 | 66.38 | 39 | 33.62 | 1.428 | 0.85-2.39 | 0.177 |
| Pentecostal | 28 | 57.14 | 21 | 42.86 | 0.965 | 0.49-1.87 | 0.916 |
| Other | 7 | 77.78 | 2 | 22 | 2.533 | 0.51-12.66 | 0.258 |
Note: *Statistically significance for independent variable and compliance to IYCF with p-Value ≤ 0.05.
Table 1: Social demographic characteristics of the respondents and compliance to infant and young child feeding.
The highest level of education attained was also a significant influencing factor of IYCF options with mothers whose highest level of secondary education being 2.31 times more likely to comply to IYCF options as compared to those who had never gone to school (OR=2.31, p=0.04, C.I 1.04-5.12). Mothers’ age categories, marital status, employment status and religion did not show any statistical significance.
Knowledge of PMTCT/IYCF for the respondents
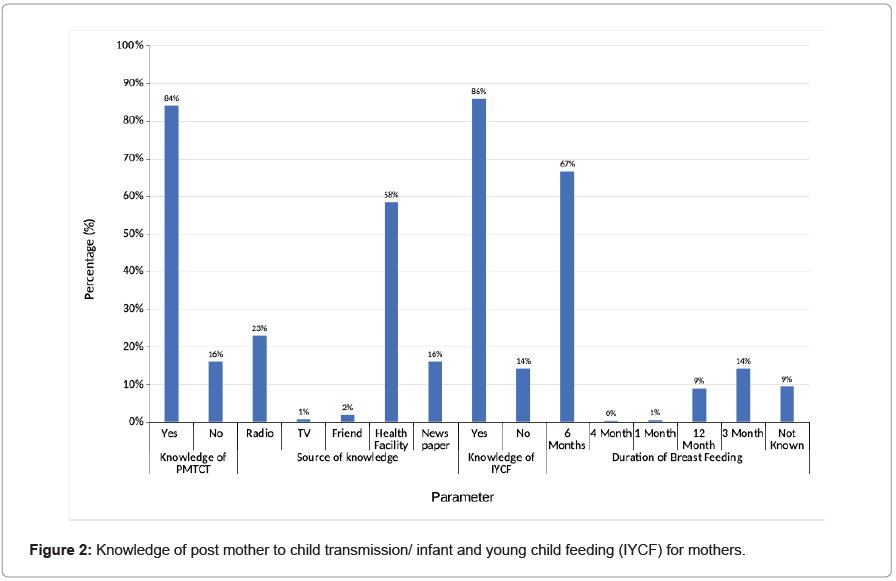
Figure 2 indicates that 83.95% of the mothers interviewed knew about PMTCT and IYCF while 16.05% did not. Most of these mothers (58.42%) reported to have got this information from the health facility while 22.89% had got information from the radio. Out of the total number of respondents, 66.58% had been informed that an HIV positive mother should breastfeed for only 6 months while 14.21% had been told that breast feeding should last for 3 months and 9.47% did not know what to do.
At bivariate analysis (Table 2), knowledge on PMTCT was found to be a significant influencing factor of compliance with IYCF options with mothers without the knowledge on PMTCT being 0.49 times less likely to comply with IYCF options. (95% C.I, 0.28-0.85, p=0.011). However, on multivariate analysis, knowledge on PMTCT was found not to be a statistically significant influencing factor of mother’s compliance to the IYCF options.
| Variable | Compliance | Non-Compliance | OR | 95% CI | p-value | ||
|---|---|---|---|---|---|---|---|
| N=236 | % | N=144 | % | ||||
| Knowledge on PMTCT | |||||||
| Yes | 207 | 64.89 | 112 | 35.11 | 0 | Reference | 0 |
| No | 29 | 47.54 | 32 | 52.46 | 0.49 | 0.28-0.85 | 0.011* |
| Knowledge on IYCF | |||||||
| Yes | 207 | 63.50 | 119 | 36.5 | 0 | Reference | 0 |
| No | 29 | 53.70 | 25 | 46.3 | 0.67 | 0.37-1.19 | 0.171 |
| Source of knowledge | |||||||
| Radio | 52 | 59.77 | 35 | 40.23 | 0 | Reference | 0 |
| TV | 2 | 66.66 | 1 | 33.33 | 1.34 | 0.11-15.42 | 0.811 |
| Friend | 6 | 85.71 | 1 | 14.29 | 4.03 | 0.46-35.01 | 0.205 |
| Health facility | 147 | 66.22 | 75 | 33.38 | 1.32 | 0.79-2.19 | 0.288 |
| News paper | 29 | 47.54 | 32 | 52.46 | 0.6 | 0.32-1.18 | 0.142 |
| Duration on Breast Feeding | |||||||
| 6 Months | 167 | 66.01 | 86 | 33.99 | 0 | Reference | 0 |
| 4Months | 0 | 0 | 1 | 100 | 0 | 0 | 0 |
| 1 Month | 0 | 0 | 2 | 100 | 0 | 0 | 0.25 |
| 12 Months | 19 | 55.88 | 15 | 44.12 | 0.65 | 0.32-1.35 | 0.35 |
| 3 Months | 32 | 59.26 | 22 | 46.74 | 0.74 | 0.41-1.37 | 0.06 |
| I don’t know | 18 | 50.00 | 18 | 50.00 | 0.51 | 0.25-1.04 | 0 |
Note: Association between the independent variable and compliance to IYCF with p-0.05
Table 2: Knowledge on post mother to child transmission/infant and young child feeding (IYCF) of the respondents and compliance to IYCF.
Each of the numbers 629,455 (approximately 63% of the population) and 829,003 (approximately 83% of the population) is a herd immunity threshold without any intervention. It must be called ‘potential (natural) herd immunity’ to distinguish it from the herd immunity suggested by the SIR model. Although potential herd immunity could be achieved sooner than expected, it is surely achieved only at the cost of so many infected individuals with so much death.
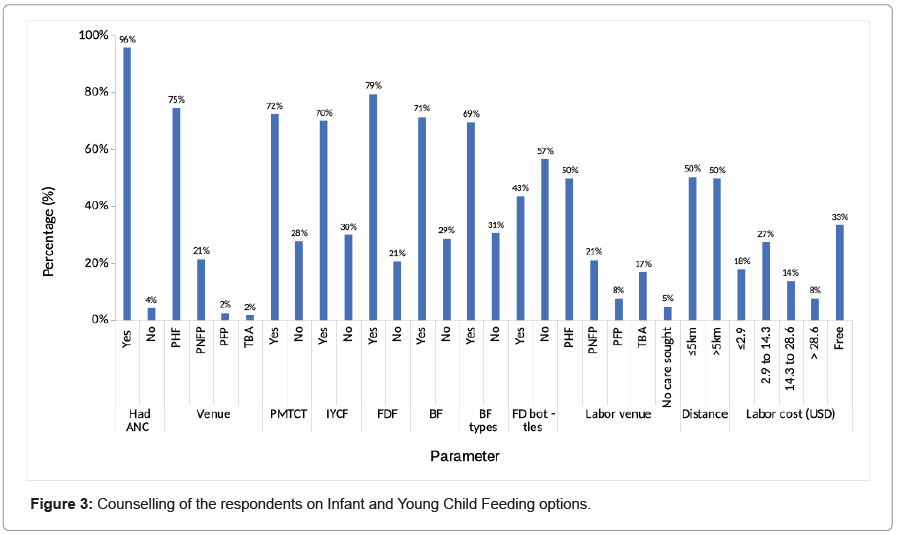
Counseling of the respondents on IYCF
Figure 3 shows that 96% of mothers attended ANC, 75% of which was at PHF, 21% at PNFP, while close to 2% were each at PFP and TBA. Of the respondents, 72% knew about PMTCT, 70% were informed about IYCF, 79% participated in PDF, 71% were aware of BF while 57% didn’t know about FD bottles. At the bivariate analysis, mothers’ attendance of ANC was found to be a significant influencing factor of IYCF options with mothers who had not attended ANC being 0.35 times less likely to comply to IYCF options (95% C.I=0.12-0.98, p=0.046), (Table 3). Also counseling on PMTCT and IYCF Were found to be significant influencing factors of IYCF options with the mothers who were counseled being 1.85 times and 1.95 times more likely to comply to IYCF options. (95% C.I=1.117-2.92, p=0.008), (95% C.I=1.25-3.65, p=0.003) respectively.
| Variable | Compliance | Non-Compliance | OR | 95% CI | p-value | ||
|---|---|---|---|---|---|---|---|
| ANC Attendance | N=236 | % | N=144 | % | |||
| Yes | 230 | 63.19 | 134 | 36.81 | 0 | Reference | 0 |
| No | 6 | 37.5 | 10 | 62.50 | 0.35 | 0.12-0.98 | 0.046* |
| Place of attendance | N=230 | N=135 | |||||
| PHF | 171 | 62.87 | 101 | 37.13 | 0 | Reference | 0 |
| PNFP | 48 | 61.54 | 30 | 38.46 | 0.95 | 0.56-1.58 | 0.831 |
| PFP | 8 | 88.89 | 1 | 11.11 | 4.72 | 0.58-38.33 | 0.146 |
| TBA | 3 | 50.00 | 3 | 50.00 | 0.59 | 0.12-2.98 | 0.524 |
| Counselling on PMTCT | N=236 | N=144 | |||||
| Yes | 54 | 51.43 | 51 | 48.57 | 1.85 | 1.17-2.92 | 0.008* |
| No | 182 | 66.18 | 93 | 33.82 | 0 | Reference | 0 |
| Counselling on IYCF | N=236 | N=138 | |||||
| Yes | 58 | 50.88 | 50 | 49.12 | 1.95 | 1.25-3.65 | 0.003* |
| No | 178 | 66.92 | 88 | 33.08 | 0 | Reference | 0 |
| Variable | Compliance | Non-Compliance | OR | 95% CI | p-value | ||
| N=179 | % | N=88 | % | ||||
| Counselling on F/D Interactions | |||||||
| Yes | 151 | 71.23 | 61 | 28.77 | 2.387 | 1.30-4.37 | 0.005* |
| No | 28 | 50.91 | 27 | 49.09 | 0 | Reference | 0 |
| Variable | Compliance | Non-Compliance | OR | 95% CI | p-value | ||
| Counselling on BF benefits | N=236 | % | N=144 | % | |||
| Yes | 179 | 66.05 | 92 | 33.95 | 0.563 | 0.36-0.88 | 0.013* |
| No | 57 | 52.29 | 52 | 47.71 | 0 | Reference | 0 |
| Counselling on BF types | |||||||
| Yes | 180 | 68.18 | 84 | 31.82 | 0 | Reference | 0 |
| No | 56 | 48.28 | 60 | 51.72 | 0.435 | 0.28-0.68 | 0.000* |
| Counselling on feeding bottles | |||||||
| Yes | 111 | 67.27 | 54 | 32.73 | 0.676 | 0.44-1.03 | 0.07 |
| No | 125 | 58.14 | 90 | 41.86 | 0 | Reference | 0 |
| Place mother delivered | |||||||
| PHF | 125 | 66.14 | 64 | 33.86 | 0 | Reference | 0 |
| PNFP | 52 | 65.00 | 28 | 35.00 | 0.950 | 0.55-1.65 | 0.857 |
| PFP | 21 | 72.41 | 8 | 27.59 | 1.344 | 0.56-3.20 | 0.505 |
| TBA | 29 | 45.31 | 35 | 54.69 | 0.424 | 0.24-0.76 | 0.004* |
| No care | 9 | 50.00 | 9 | 50.00 | 0.512 | 0.19-1.35 | 0.177 |
| Distance from place | |||||||
| ≤5 km ˃5KM |
127 109 |
66.49 57.67 |
64 80 |
33.51 42.33 |
0 0.687 |
Reference 0.45-1.04 |
0 0.077 |
| Cost for labour | |||||||
| <10,000 | 47 | 69.12 | 21 | 30.88 | 0 | Reference | 0 |
| 10,001-50,000 | 63 | 60.58 | 41 | 39.42 | 0.68 | 0.36-1.31 | 0.255 |
| 50,001-100,000 | 33 | 63.46 | 19 | 36.54 | 0.77 | 0.36-1.67 | 0.515 |
| 0ver 100,000 | 16 | 55.17 | 13 | 44.83 | 0.54 | 0.22-1.35 | 0.190 |
| Free | 77 | 60.63 | 50 | 39.37 | 0.68 | 0.37-1.28 | 0.242 |
Note: *Association between the independent variable and compliance to IYCF with p-0.05
Table 3: Counselling of the respondents on infant and young child feeding (IYCF) of the respondents and compliance to IYCF options.
Counseling on food and drug interactions as well as breastfeeding types were also found to be significant influencing factors to mothers’ compliance to IYCF options with mothers counseled on food and drug interactions being 2.387 times more likely to comply to IYCF options, 95% C.I=1.30-4.37, p=0.005) while those mothers who were not counseled on breast feeding types were 0.435 times less likely to comply to IYCF options. (95% C.I=0.28-0.68, p=0.000).
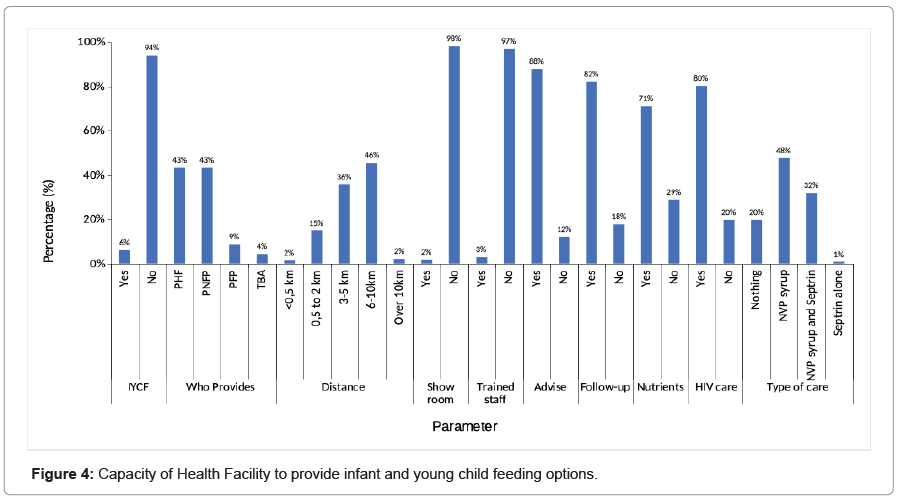
Capacity of HF to provide IYCF
Figure 4 indicates only 6.05% of the respondent reported presence of IYCF services in their community. A key informant (HIV counselor- Mukono Municipality HCIV) and 93.95% of the mothers reported absence of IYCF services. Of the mothers interviewed, 45.53% reported that they travel between 6 to10 kilometers to the health facilities. 98.16% of the respondents reported absence of IYCF demonstration rooms as well as the absence of specific trained IYCF trained personnel. It was also reported by key informant (PMTCT facilitator-Kojja HCIV) that; “we do not go for outreaches on such things”. Out of the total number of respondents, 87.80% had been advised on follow-up of their children. 71.05% had got micronutrient supplements while 80.26% had received support for their HIV exposed children. Also 80.26% of the respondents had received NVP syrup and Septrin while 19.75% had received nothing. This was confirmed by four key informants claiming to make phone calls to the mothers who disappear or delay returning for follow-up.
At Bivariate analysis (Table 4), advise on follow-up as well as following-p of the HIV exposed children were found to be significant influencing factors to mothers’ compliance to IYCF options with mothers who were not given advise on follow-up being 0.483 times less likely to comply to IYCF options (95% C.I (0.26-0.89), p =0.021). The mothers who were not followed-up were also 0.595 times less likely to comply to IYCF options (95% C.I, 0.36-0.98), p=0.04. The type of support given to the mother was also found to be a significant factor influencing compliance to IYCF options with mothers given NVP syrup being 1.513 times more likely to comply to IYCF options as compared to those who were not given anything, (95% C.I1.12-2.13). p=0.006, Mothers who were also given both NVP syrup and Septrin were 3.321times more likely to comply, 95% C.I (2.17-5.06 p=0.000).
| Variable | Compliance | Non-Compliance | OR | 95% CI | p-value | ||
|---|---|---|---|---|---|---|---|
| N=236 | % | N=144 | % | ||||
| Presence of IYCF services | |||||||
| Yes | 14 | 60.87 | 9 | 39.13 | 0 | Reference | 0 |
| No | 222 | 62.18 | 135 | 37.82 | 1.06 | 0.44-2.51 | 0.900 |
| Distance from facility | |||||||
| <1/2km | 4 | 66.67 | 2 | 33.33 | 0 | Reference | 0 |
| 1/2km—2km | 39 | 68.42 | 18 | 31.558 | 1.08 | 0.18-6.46 | 0.93 |
| 3-5km | 83 | 61.03 | 53 | 38.97 | 0.78 | 0.13-4.4 | 0.78 |
| 6-10km | 103 | 59.54 | 70 | 40.46 | 0.73 | 0.13-4.13 | 0.72 |
| 0ver 10km | 7 | 87.5 | 1 | 12.50 | 3.5 | 0.24-51.9 | 0.36 |
| Availability of demonstration room | |||||||
| Yes | 6 | 85.71 | 1 | 14.29 | 0 | Reference | 0 |
| No | 230 | 61.66 | 143 | 38.34 | 3.73 | 0.44-31.3 | 0.225 |
| Presence of trained personnel | |||||||
| Yes | 8 | 72.73 | 3 | 27.27 | 0 | Reference | 0 |
| No | 228 | 61.79 | 141 | 38.21 | 1.649 | 0.43-6.31 | 0.465 |
| Advise on follow-up | |||||||
| Yes | 221 | 66.17 | 113 | 33.83 | 0 | Reference | 0 |
| No | 15 | 32.61 | 31 | 67.39 | 0.483 | 0.26-0.89 | 0.021* |
| Follow-up on infant | N= 235 | N = 144 | |||||
| Yes | 210 | 67.31 | 102 | 32.69 | 0 | Reference | 0 |
| No | 25 | 37.31 | 42 | 62.69 | 0.595 | 0.36-0.98 | 0.040* |
| Micronutrient provided | N= 236 | N =144 | |||||
| Yes | 188 | 69.63 | 82 | 30.37 | 0 | Reference | 0 |
| No | 48 | 43.64 | 62 | 56.36 | 0.774 | 0.53-1.12 | 0.183 |
| Provided with Vitamin A | |||||||
| Yes | 191 | 69.45 | 84 | 30.55 | 0 | Reference | 0 |
| No | 45 | 42.86 | 60 | 57.14 | 0.75 | 0.51-1.10 | 0.145 |
| Support for HIV exposed child | |||||||
| Yes | 205 | 67.21 | 100 | 32.79 | 0 | Reference | 0 |
| No | 31 | 41.33 | 44 | 58.67 | 0.704 | 0.44-1.12 | 0.135 |
| Type of support | |||||||
| Nothing | 31 | 41.33 | 44 | 58.67 | 0 | Reference | 0 |
| NVP syrup | 109 | 60.22 | 72 | 39.78 | 1.513 | 1.12-2.03 | 0.006* |
| NVP & Septrin | 93 | 76.86 | 28 | 23.14 | 3.321 | 2.17-5.06 | 0.000* |
| Septrin | 3 | 100.0 | 0 | 0 | 0 | 0 | 0 |
Note: *Association between the independent variable and compliance to IYCF with p-0.05.
Table 4: Capacity to of health facility to provide infant and young child feeding (IYCF) of the respondents and compliance to IYCF options.
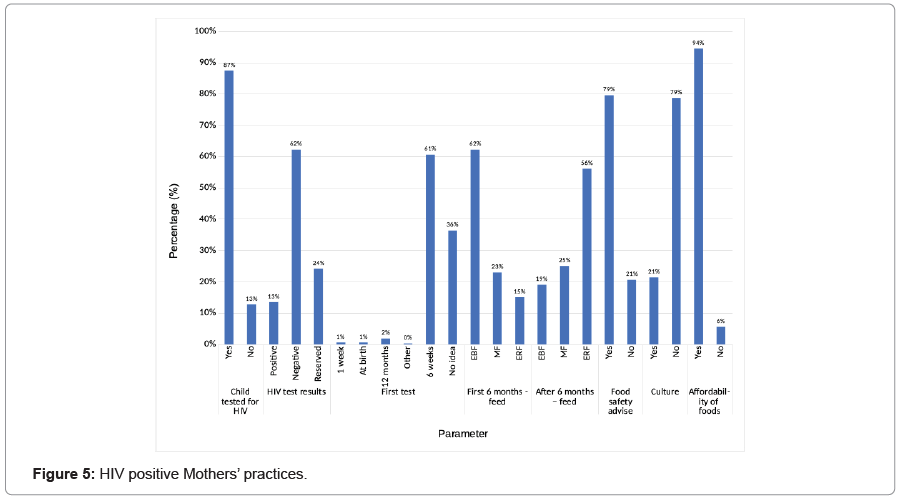
HIV positive mothers’ practices
Figure 5 shows that a majority (87.37%) of the mothers had their children tested for HIV. Out of the 380 respondents with infants, 13.42% had their children HIV positive. 62.11% were HIV negative while 24.05% did not wish to say.
Furthermore, Figure 5 also indicates that 62.11% of the respondents practiced EBF for the first six months, 22.89% practiced MF while 15% had practiced ERF. After six months, 56.05% opted for ERF while 25% used for MF and 18.95% continued with EBF. 79.47% had received advice on replacement food safety, 78.68% did not have any cultural barriers regarding replacement foods while 94.47% could afford to buy replacement feeds.
At Bivariate analysis (Table 5), the HIV test result of the child was found to be a significant to influence the mother’s compliance to IYCF option with the HIV positive test result being 0.14 times less likely to comply to IYCF options (95% C.I0.06-0.29, P=0.000).
| Variable | Compliance | Non-Compliance | OR | 95% CI | p-value | ||
|---|---|---|---|---|---|---|---|
| N=236 | % | N=144 | % | ||||
| Baby tested for HIV | |||||||
| Yes | 202 | 60.84 | 130 | 39.16 | 0.64 | 0.33-1.23 | 0.185 |
| No | 34 | 70.83 | 14 | 29.17 | 0 | Reference | 0 |
| HIV test Results | |||||||
| I don’t Know | 68 | 73.12 | 25 | 26.88 | 0 | Reference | 0 |
| Negative | 154 | 65.25 | 82 | 34.75 | 0.69 | 0.41-1.17 | 0.172 |
| Positive | 14 | 27.45 | 37 | 72.55 | 0.14 | 0.06-0.29 | 0.000* |
| Time for first HIV test of child | |||||||
| 1 Week | 1 | 50 | 1 | 50.00 | 0 | Reference | 0 |
| Birth | 1 | 50 | 1 | 50.00 | 1 | 0.19-50.39 | 1.000 |
| 12 Months | 6 | 85.71 | 1 | 14.29 | 6 | 0.18-196.3 | 0.314 |
| Others | 0 | 0 | 1 | 100.00 | 0 | 0 | 0 |
| 6 Weeks | 162 | 70.43 | 68 | 29.57 | 2.38 | 0.14-38.64 | 0.541 |
| I don’t know | 66 | 47.83 | 72 | 52.17 | 0.91 | 0.56-14.95 | 0.951 |
| Feed type after 6 months | |||||||
| EBF | 71 | 98.61 | 1 | 1.39 | 0 | Reference | 0 |
| MF | 21 | 22.11 | 74 | 77.89 | 0.283 | 0.17-0.46 | 0.000* |
| ERF | 144 | 67.61 | 69 | 32.39 | 2.086 | 1.56-2.78 | 0.000* |
| Advise on replacement foods safety | |||||||
| Yes | 200 | 66.23 | 102 | 33.77 | 0.857 | 0.55-1.33 | 0.497 |
| No | 36 | 46.15 | 42 | 53.85 | 0 | Reference | 0 |
| Cultural/Social barriers to RF | |||||||
| Yes | 48 | 59.26 | 33 | 40.74 | 0.858 | 0.52-1.42 | 0.552 |
| No | 188 | 62.88 | 111 | 37.12 | 0 | Reference | 0 |
| Affordability of Replacement feeds | |||||||
| Yes | 230 | 64.07 | 129 | 35.93 | 4.46 | 1.68-11.76 | 0.003* |
| No | 6 | 28.57 | 15 | 71.43 | 0 | Reference | 0 |
Note: *Association between the independent variable and compliance to IYCF with p-0.05.
Table 5: Differences Mother’s practices and compliance to infant and young child feeding options.
Feed type after six months was also found to be a significant factor to influence compliance to IYCF options with the mothers who practiced mixed feeding being 0.283 times less likely to comply to IYF options (95% C.I (0.17-0.46, p=0.000). Those mothers who practiced exclusive replacement feeding were 2.086 times more likely to comply with IYCF options, (95% C.I, 1.56-2.78, p=0.000).
Affordability of replacement feeds was also significant factor to influencing compliance to IYCF options with those mothers who and the ones who could not afford replacement feeds being 4.46 times more likely to comply to IYCF options, (95% C.I(1.68-11.76, p=0.003).
Discussion
In social demographic characteristics
Age of baby and mother’s compliance with the IYCF options: The age of the baby and the age of the mother can be a predictor of the mother’s compliance with the recommended IYCF options in Uganda. In this study, there was a statistically significant association (OR=2.55, 95% C.I (1.25-5.19) between the age of the baby (13-24 months) and compliance to IYCF options. These mothers of babies aged 13-24 months were 2.55 times more likely to comply to IYCF options while there was no association between the age of the mother and compliance with IYCF. This was contrary to a study in Bangladesh which found mothers over 35 years of age 2.3 more times likely to use bottle feeding than the recommended breast-feeding practices [11]. This implies that age of the mother in the Ugandan setting as compared to that in Bangladesh cannot be based on alone to influence their compliance to the recommended IYCF options and therefore, other factors must be put in consideration as is discussed later [12-14,10].
Marital status of mother and her compliance with the IYCF options
One of the known influencing factors to PMTCT interventions such as IYCF in Uganda is marital status of the mother. However, in our study, marital status was found not to be a predictor of mother’s compliance to IYCF options since there was no association particularly in Mukono district. This implies that in Ugandan setting, marital status of the mother cannot be based on to influence their compliance with the recommended IYCF options [13,15-17].
Mother’s place of residence and her compliance with the IYCF options
Mother’s place of residence was found not to be a predictor of mother’s compliance to IYCF options in our study since there was no association. This implies that in Mukono district, mother’s compliance with the recommended IYCF options cannot be based on their place of residence [18].
Mothers’ level of education and her compliance with the IYCF options
The education level of the mother can be a predictor of the mother’s compliance with the recommended IYCF options in Uganda. In our study, there was a statistically significant association between mothers with secondary education and compliance with recommended IYCF options (OR=2.29, 95% C.I (1.23-4.28) p=0.004) [19].
These mothers were 2.29 times more likely to comply to IYCF options as compared to those who had never gone to school, after adjusting for follow-up of the child. This agreed with the findings of the cross-sectional study done in Eastern Uganda that found well educated mothers breast feeding for a substantially shorter time than their less educated peers [20]. This implies that education level of the mother in Ugandan setting particularly in Mukono district can be based on to influence their compliance to the recommended IYCF options [21].
Mother’s level of income and her compliance with IYCF options
Mother’s level of income was found not to be a predictor of mother’s compliance to IYCF options in our study since there was no association. This implies that in Ugandan setting, mother’s level of income in Mukono district cannot be based on to influence their compliance with the recommended IYCF options. This is contrary to the findings of a study in Ghana where all the mothers were found confident that they would use infant formula if distributed free of charge [22].
Mother’s knowledge on PMTCT and IYCF and her compliance to IYCF options
Knowledge on PMTCT, IYCF, BF and EBF and mother’s compliance to IYCF options: Knowledge of the mother on PMTCT, BF and EBF can be a predictor of mother’s compliance to recommended IYCF options. In our study, there was a statistically significant association between knowledge of the mother on PMTCT, BF, ERF, and compliance to IYCF at Bivariate analysis where mothers without the knowledge on PMTCT were 0.49 times less likely to comply to IYCF options (95% C.I, 0.28-0.85, p=0.011).
However, on multivariate analysis, knowledge on PMTCT was found not to be a significant influencing factor of mother’s compliance to the IYCF options. This was contrary to findings of similar studies in Southwestern Kenya which concluded that MTCT knowledge influences the choice of alternative feeding option [23]. This implies that knowledge of the mother on PMTCT, BF and ERF in the Ugandan setting as compared to that in Southwestern Kenya cannot be based on to influence their compliance to the recommended IYCF options and therefore, other factors must be put in consideration [23].
Counseling of the mother on IYCF options and her compliance to IYCF options
Site where mother attends ANC and her compliance to IYCF options: The site where mothers attend ANC was found not to be a predictor of mother’s compliance to IYCF options in our study since there was no association. This implies that in Mukono district, site where mothers attend ANC cannot be based on to influence their compliance with the recommended IYCF options. This is contrary to the findings of a South African study where it was reported that the risks associated with formula feeding varied from place to place [24].
Counseling during ANC, PMTCT, ART
Mothers’ attendance of ANC can be a predictor of mother’s compliance to recommended IYCF options. In our study, there was a statistically significant association between mother’s attendance of ANC and compliance with IYCF at Bivariate analysis where mothers who had not attended ANC were 0.35 times less likely to comply to IYCF options (95% C.I (0.12-0.98), p=0.046). This study also found that mothers who were counseled on PMTCT were 1.85 times more likely to comply to IYCF options (95% C.I (1.117-2.92, p=0.008) while those who were counseled on IYCF were 1.95 times more likely to comply to IYCF options. (95% C.I (1.25-3.65), p=0.003). Mothers who were counseled on food and drug interactions were 2.387 times more likely to comply to IYCF options, 95% C.I (1.30-4.37, p=0.005) while those mothers who were not counseled on breast feeding types were 0.435 times less likely to comply to IYCF options (95% C.I(0.28-0.68, p=0.000).
However, on multivariate analysis, counseling on the above- mentioned factors was found not to be statistically significant at influencing compliance with IYCF options. This was contrary to the findings of the descriptive cross-sectional study in Kibera Nairobi where infant feeding counseling was found to be important in influencing infant feeding practices [25]. This implies that counseling on the above-mentioned factors in the Ugandan setting particularly in Mukono district as compared to that in Kibera Nairobi cannot be based on to influence their compliance to the recommended IYCF options and therefore, other factors must be put in consideration.
Capacity of PMTCT facilities and mother’s compliance to IYCF options
Availability of demonstration rooms at the facilities and the mother’s compliance to IYCF: The availability of demonstration rooms was found not to be a predictor of mother’s compliance to IYCF options in our study because there was no association. Since there was no association between availability of demonstration rooms and mother’s compliance with the recommended IYCF options, availability of demonstration rooms cannot be based on to influence mother’s compliance with the IYCF options in Mukono district, [26-29].
Availability of well-trained medical personnel and mother’s compliance with IYCF options
The availability of well-trained medical personnel was found not to be a predictor of mother’s compliance to IYCF options in our study because there was no association. Since there was no association between well trained medical personnel and mother’s compliance with the recommended IYCF options, in Ugandan setting, availability of well-trained medical personnel cannot be based on to influence mother’s compliance with the IYCF options [13,30,31].
Capacity to follow-up HIV exposed infants and mother’s compliance to IYCF options
Advice on follow-up can be a predictor of mother’s compliance to recommended IYCF options. In our study, there was a statistically significant association between advice on follow-up as well as following- up of the HIV exposed children and compliance to IYCF options at Bivariate analysis where mothers who were not given advise on follow- up were 0.483 times less likely to comply to IYCF options (95% C.I (0.26-0.89), p=0.021). The mothers whose children were not followed- up were also 0.595 times less likely to comply to IYCF options (95% C.I, 0.36-0.98, p=0.04).
Type of support given to the mother can also be a predictor of mother’s compliance with IYCF options. In our study, mothers who were given NVP syrup were 1.513 times more likely to comply with IYCF options as compared to those who were not given anything, (95% C.I 1.12-2.13). p=0.006, Mothers who were also given both NVP syrup and Septrin were 3.321times more likely to comply with IYCF options, (95% C.I, 2.17-5.06, p=0.000).
However, on multivariate analysis, the above factors were found not to be significant in influencing compliance to IYCF options. This is contrary to the research findings in Mexico and Bangladesh where infant feeding practices improved after implementing specifically designed follow-up home based interventions [32]. This implies that in the Ugandan setting, advice on follow-up and type of support given to the child cannot be based on to influence the mother’s compliance to the recommended IYCF options and therefore, other factors must be put in consideration.
HIV positive mother’s practices and her compliance to IYCF options
Exclusive Breast Feeding and compliance to IYCF options: Exclusive Breast Feeding for the first six months can be a predictor of mother’s compliance to recommended IYCF options. In our, study most mothers were practicing EBF (62.11%) (236/380) before six months as recommended by the guidelines. This was consistent with the findings of a study done in Southern Ghana about factors influencing the choices of infant feeding in HIV positive mothers where 62% of the mothers were practicing exclusive breast feeding [22].
The results of our study also revealed that of the 144 mothers who did not practice only EBF for the first six months, 25.69% mothers had infected their children with HIV. Exclusive Breast Feeding for the first six months [33,34] therefore formed the measure of compliance in our study based on the MoH IYCF guidelines and has been seen to be a predictor of mother’s compliance with recommended IYCF options in Ugandan setting.
Mixed feeding, exclusive replacement feeding and mother’s compliance with IYCF options
Mixed Feeding and Exclusive Replacement Feeding can be predictors of mothers’ compliance with recommended IYCF options in Uganda [1]. In our study, 95/380 children had received mixed feeding after six months and of the 95 children, 26 had been infected with HIV (27.37%) consistent with the findings of a South African study where 36% of the babies who received mixed feeding were reported infected with HIV [13].
In our study, there was a statistically significant association between the mothers who practiced mixed feeding and they were 0.002 times less likely to comply to IYCF options even after adjusting for time at which first test of the child is taken, advise on follow-up of the child and cost of replacement feeds with (95% C.I, <0.000- 0.0000; p=0.000). The Mothers who practiced Exclusive Replacement feeding were 0.02 times less likely to comply with IYCF (95% C.I, <0.000-0.0000, p=0.000). This implies that mixed feeding and exclusive replacement feeding in the Ugandan setting can be based on to influence mothers’ compliance to the recommended IYCF options [35].
HIV Test result of children and the mother’s compliance with IYCF options
HIV Test result of children can also be a predictor of mother’s compliance with the recommended IYCF options in Uganda. In our study, there was a statistically significant association between the mothers whose children tested positive and compliance to IYCF options. These mothers were 0.13 times less likely to comply with IYCF options (95% C.I (0.04-0.43) p=0.001) [36]. This implies that HIV test result of children in the Ugandan setting can be based on to predict the mother’s compliance to the recommended IYCF options.
Conclusion
The study focused on HIV positive breastfeeding mothers and their compliance to the Ministry of Health recommended feeding options. The predictors of mothers’ compliance to the recommended IYCF options were found to be:
• Age of the HIV exposed baby,
• Education level of the HIV positive mother,
• Feed type practiced (either ERF, MF or EBF) by the mother after six months and
• The HIV test result of children was all found to be.
More work needs to be done by the Ministry of Health especially community sensitization and teaching mothers the best ways to avoid infecting their babies with HIV.
Ethics Approval and Consent to Participate
The proposal for this study was submitted for review and clearance to the International Health Sciences University Research and Ethics committee. Permission to carry out the study in the Health facilities was sought from the Chief Administrative Officer (CAO) for Mukono district and the District Health officer (DHO) accompanied by an introduction letter from the School of Health Sciences Research regulation authorities. Informed consent was sought from health officers in charge of these health facilities and the mothers before any enrolment and data collection was done. This study ensured no risk to the human subjects participating in the study.
Consent for Publication
All the co-authors give the IBFJ to their consent to publish this paper.
Availability of Data and Materials
All the data associated with this research has been provided.
Competing Interests
The authors declare no competing interest.
Funding
Not applicable
Authors’ Contributions
Ketra Nakayenga did the research and participated in the manuscript writing. Peter Kirabira supervised the research and proofread the article. Antony Nyombi compiled the entire article including statistical analysis. Daniella Birungi and Joel Kimera contributed in data analysis and interpretation
Acknowledgements
We thank the Institute of Health Policy and Management of International Health Sciences University for the logistical support given to the study.
References
- Atashili J, Kalilani L, Seksaria V, Sickbert-Bennett EE (2008) Potential impact of infant feeding recommendations on mortality and HIV-infection in children born to HIV-infected mothers in Africa: a simulation. BMC Infect Dis 8:66.
[Crossref] [Google Scholar] [PubMed]
- UNICEF (2012) Preventing mother-to-child transmission (PMTCT) of HIV.
- Centres for Disease Control (2012) Mother-to-child transmission of HIV and syphilis globally.
- World Health Organization (WHO) (2008) HIV transmission through breastfeeding: a review of available evidence: 2007 update.
- Nabwera HM, Jepkosgei J, Jepkosgei KW, Amin SH, Molyneux CS, et al. (2017) What influences feeding decisions for HIV-exposed infants in rural Kenya? Int Breastfeed J 12:31.
[Crossref] [Google Scholar] [PubMed]
- WHO/UNAIDS (1998) HIV and infant feeding guidelines for decision-makers.
- WHO/UNAIDS (2006) HIV and infant feeding : update based on the technical consultation held on behalf of the Inter-agency Team (IATT) on Prevention of HIV Infections in Pregnant Women, Mothers and their Infants.
- Chinkonde JR, Hem MH, Sundby J (2012) HIV and infant feeding in Malawi: public health simplicity in complex social and cultural contexts. BMC Public Health 12:700.
[Crossref] [Google Scholar] [PubMed]
- UNICEF/Uganda Ministry of Health (2021) Guidelines on maternal, infant, young child and adolescent nutrition.
- WHO/Uganda Ministry of Health (2007) Policy Guidelines on infant and young child feeding.
- Mihrshahi S, Kabir I, Roy SK, Agho KE, Senarath U, et al. (2010) Determinants of infant and young child feeding practices in Bangladesh: Secondary data analysis of demographic and health survey 2004. Food Nutr Bull 31:295-313.
[Crossref] [Google Scholar] [PubMed]
- Zabinah N, Frank K, Zainah N, Ivan K, Agbele AT (2018) Mothers’ adherence to optimal infant and young child feeding practices in Uganda: a cross-sectional study. F1000Research 7:877.
- WHO/Uganda Ministry of Health (2009) Policy guidelines on infant and young child feeding.
- National Guide on Nutrition Care and Support for PLHAs (2003) Question and answer guide on infant and young child feeding (IYCF) for health care providers. A reference tool for health care workers of PMTCT and MCH program in Tanzania.
- Yeshalem MD, Tadese ET, Dereje BA (2017) Infant and young child feeding practice among mothers with 0-24 months old children in Slum areas of Bahir Dar City, Ethiopia. Int Breastfeed J 12:26.
[Crossref] [Google Scholar] [PubMed]
- Kamau AN (2013) Assessment of mothers compliance with national infant and young child feeding recomendations amongst children aged 0-24 months in nakuru municipality, Kenya.
- Stephen KA, Mahama S, Florian F, Alexander K (2020) Association between infant and young child feeding (IYCF) Indicators and the nutritional status of children (6-23 Months) in Northern Ghana. Nutrients 12:2565.
[Crossref] [Google Scholar] [PubMed]
- IFE (2017) Infant and young child feeding in emergencies: operational guidance for emergency relief staff and programme managers.
- Scott BI, Taylor EH, Valerie LF (2015) Maternal literacy, facility birth, and education are positively associated with better infant and young child feeding practices and nutritional status among ugandan children. J Nutr 145:2578-2586.
[Crossref] [Google Scholar] [PubMed]
- Fadnes L, MS I, Engebretsen, Henry W, Jonathan W (2009) Need to optimize infant feeding counselling: a cross-sectional survey among HIV-positive mothers eastern Uganda. BMC Paedriatics 9:2.
[Crossref] [Google Scholar] [PubMed]
- Yeshalem MD (2017) Factors associated with mothers’ knowledge on infant and young child feeding recommendation in slum areas of Bahir Dar City, Ethiopia: cross sectional study. BMC Res Notes 10.
[Crossref] [Google Scholar] [PubMed]
- Suuk AL, Veloshnee G (2011) Factors influencing the choices of infant feeding of HIV positive mothers in Southern Ghana: The role of counselors, mothers, families and socio-economic status. J AIDS HIV Res 3:129-137.
- Omwega A, Oquta T, Sehmi JK (2006) Maternal knowledge on mother- to-child transmission of HIV and breast milk alternatives for HIV positive mothers in Homo Bay District Hospital, Kenya. East Afr Med J 83:10-18.
[Crossref] [Google Scholar] [PubMed]
- Tomlinson C (2012) Infant feeding: TAC’s position.
- Wycliffe Ayieko (2007) Determinants of infant and young child feeding practices among HIV Positive mothers in Kibera, Nairobi, Kenya.
- CK Mishra (2017) National guidelines on lactation management centres in public health facilities.
- Potential impact of infant feeding recommendations on mortality and HIV-infection in children born to HIV-infected mothers in Africa: a simulation
- MCI-CAH WHO/AFRO (2003) Information package on infant and young child feeding activities.
- Tina S, Luann M, Nemat H, Teweldebrhan HA, Yewelsew A, et al. (2013) Strengthening systems to support mothers in infant and young child feeding at scale. Food Nutr Bull 34:156-168.
[Crossref] [Google Scholar] [PubMed]
- European Union (2014) Infant and young children feeding in emergencies: guidance for programming.
- World Vision (2017) Infant & Young Child Feeding in Emergencies (IYCF‐E) and why it Matters.
- Ameena EG, Tanya D, Debra JJ, David S, Mark C, et al. (2012) Infant feeding practices at routine PMTCT sites, results of a prospective observational study amongst HIV exposed and unexposed infants birth to 9 months. Int Breast Feed J 7:4.
[Crossref] [Google Scholar] [PubMed]
- Kasinga F, Mogotlane SM, Van Rensburg GH (2008) Knowledge of pregnant women on transmission of HIV infection through breast feeding. Curationis 31:21-26.
[Crossref] [Google Scholar] [PubMed]
- Olorunfemi SO, Dudley L (2018) Knowledge, attitude and practice of infant feeding in the first 6 months among HIV-positive mothers at the Queen Mamohato Memorial hospital clinics, Maseru, Lesotho. African J Prim Heal Care Fam Med 10:e1-e12.
[Crossref] [Google Scholar] [PubMed]
- UNHCR (2015) Infant and young child feeding practices: Standard Operating Procedures for the Handling of Breast milk Substitutes (BMS) in Refugee Situations for children 0-23 months.
- Muluye D, Woldeyohannes D, Gizachew M, Tiruneh M (2012) Infant feeding practice and associated factors of HIV positive mothers attending prevention of mother to child transmission and antiretroviral therapy clinics in Gondar Town health institutions, Northwest Ethiopia. BMC Public Health 12:240.
[Crossref] [Google Scholar] [PubMed]
Citation: Nakayenga K, Kirabira P, Nyombi A, Birungi D and Kimera J (2022) HIV Positive Breast-Feeding Mothers’ Compliance with the Ministry of Health Recommended Infant and Young Child Feeding Options In Mukono District, Uganda. J Infect Dis Ther S5:003.
Copyright: © 2022 Nakayenga K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1715
- [From(publication date): 0-2022 - Nov 23, 2024]
- Breakdown by view type
- HTML page views: 1491
- PDF downloads: 224