Research Article Open Access
HIV Infection Complications during Childhood
Daniela Pereira1, Marina Oliveira Martins2, Laura Hora Marques3 and Humberto S Machado1,4,5*
1Instituto de Ciências Biomédicas Abel Salazar, Universidade do Porto, Portugal
2USF Tornada, ARS Lisboa e Vale do Tejo, Portugal
3Serviço de Pediatria, Centro Hospitalar Universitário do Porto, Portugal
4Serviço de Anestesiologia, Centro Hospitalar Universitário do Porto, Portugal
5Centro de Investigação Clínica em Anestesiologia, Centro Hospitalar Universitário do Porto, Portugal
- *Corresponding Author:
- Machado HS
Serviço de Anestesiologia
Centro Hospitalar Universitário do Porto
Portugal, Portugal
Tel: 351935848475
E-mail: hjs.machado@gmail.com
Received date: March 28, 2017; Accepted date: April 13, 2017; Published date: April 18, 2017
Citation: Pereira D, Martins MO, Gonçalves LE, Machado HS (2017) HIV Infection Complications during Childhood. J Preg Child Health 4:313. doi:10.4172/2376-127X.1000313
Copyright: © 2017 Pereira D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
According to the World Health Organization (WHO), about 2.1 million children under the age of 15 were infected with the Human Immunodeficiency Virus (HIV) in 2015. The introduction of combined antiretroviral therapy (CART) has changed the natural history of Patients infected with HIV. Chronic diseases associated with HIV infection have taken a more prominent role in relation to acute infections. This literature review aims to systematize the complications associated with HIV infection in the pediatric age (defined by the WHO as that between birth and 19 years) in two large groups: infectious diseases and non-infectious diseases. In the group of infectious diseases, it is intended to emphasize the most prevalent infections in the pediatric age, while in the group of non-infectious diseases we aim to present the main complications by organs and systems. The search engine used to conduct the search was the PubMed and The Pediatric Infectious Disease Journal. In this paper, HIV infection is treated as a systemic infection, with the direct consequences of infection per se and the indirect consequences associated with the introduction of CART. The main complications are infectious, mucocutaneous, cardiovascular, respiratory, neurological, nephrological, gastrointestinal, otorhinolaryngological, ophthalmologic, endocrinological and neoplastic, as well as immune reconstitution syndrome associated with CART. In conclusion, the pediatric complications associated with HIV infection vary with the immunosuppression state, the transmission route, the age at infection contraction and at the introduction of CAR and the geographical location of the infected children. CART decreased the incidence of opportunistic infections and neoplasms, but paradoxically is associated with an increased incidence of immune reconstitution syndrome, cardiovascular diseases, metabolic syndrome and lipodystrophy. Early detection of complications improves the quality of life of the pediatric population. Thus, the research and training of health professionals who accompany them is crucial.
Keywords
HIV; AIDS; Paediatric age; Opportunistic infections; Metabolic syndrome; Stunting; Lipodystrophy
Introduction
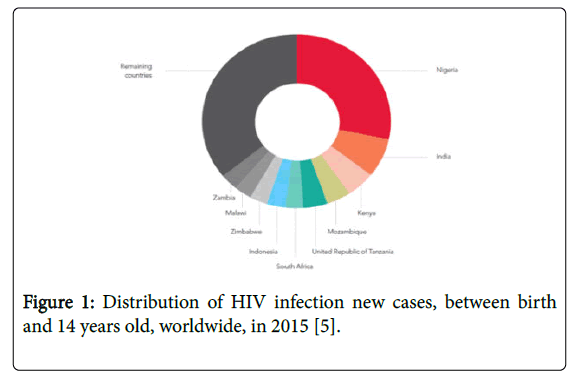
According to the World Health Organization (WHO), about 36.7 million people were infected with the Human Immunodeficiency Virus (HIV) in 2015, with 2.1 million corresponding to new cases. In that year, the number of HIV-infected pediatric patients (HIV-IPP) under the age of 15 was 3.2 million, 150,000 of which were new cases. [1,2] It should be noted that 90% of the infected pediatric population is in Sub-Saharan Africa [3,4] and that a quarter of all new cases were registered in Nigeria (Figure 1) [5].
The main route of transmission at the pediatric age is mother-tochild transmission (90%) and may occur during pregnancy, childbirth (50-70%), or breastfeeding. Other routes of transmission are blood transfusion and sexual pathways [4,6-8].
HIV infection acquired at the pediatric age, by affecting an immature immune system, is associated with distinct chronic complications and bigger morbidity [3,9].
HIV infection prenatal diagnosis, introduction of prophylaxis with combined antiretroviral therapy (CART) in seropositive mothers and preventive measures during child-birth have enabled the reduction of vertical transmission of HIV infection [3,6,10]. Besides, medical follow-up of children with in uterus exposure to HIV infection also allows the early diagnosis and treatment, improving their survival rates [3,9,11,12].
If the diagnosis of HIV infection is obtained during the child medical follow-up due to exposure to HIV infection during pregnancy, its presentation is usually asymptomatic. However, the diagnosis can also be done based on the diseases that affect these children or adolescents. The most common is that HIV-IPP present with common infections of their age group, but with higher frequency, severity, recurrence and those infections may be more treatment-refractory than in non HIV-infected pediatric patients (NHIV-IPP) [6,9].
In the absence of TARC, there is a group of patients that presents a slow progression of the disease and that can remain asymptomatic until adolescence, that contrasts with the group of patients with early development of acute infections or illnesses associated with immunodeficiency in the first year of life or in the school age [3,9].
Thanks to the introduction of CART, HIV infection has become a chronic disease [13-18] and the pediatric population infected reaches adulthood and therefore the survival and prevalence of HIV-IPP have increased [3,19]. Mortality associated with chronic multisystem diseases related to both HIV infection and CART has increased, whereas mortality associated with acute opportunistic infections and AIDS-defining illnesses has progressively decreased since the introduction of CART [9,13-16,18,20].
This literature review aims to describe the systemic complications associated with HIV infection in the pediatric age (defined by the WHO as that between birth and 19 years [19]), namely, direct ones, caused by infection per se and indirect ones, associated with the introduction of CART. This will be structured in 3 large groups: infectious complications, non-infectious complications and immune reconstitution syndrome (IRS). In the group of infectious complications, the aim is to emphasize the most prevalent infections in the pediatric age, in the group of non-infectious complications we intend to present the main complications by organs and systems and in the latter group we intend to characterize the IRS.
Methods
A search was performed on PubMed, using the following formula of words MesH("HIV"[Mesh] OR "Acquired Immunodeficiency Syndrome"[Mesh]) AND ("Child"[Mesh] OR "Infant"[Mesh] OR "Infant, New-born"[Mesh] OR "Child, Preschool"[Mesh] OR "Adolescent"[Mesh]) AND ("AIDS-Related Opportunistic Infections"[Mesh] OR "Opportunistic Infections"[Mesh] OR "Chronic Disease"[Mesh] OR "Cardiovascular Diseases"[Mesh] OR "Endocrine System Diseases"[Mesh] OR "Vitamin D Deficiency"[Mesh] OR "Respiratory Tract Diseases"[Mesh] OR "Respiration Disorders"[Mesh] OR "Urologic Diseases"[Mesh] OR "Hematologic Diseases/ epidemiology"[Mesh] OR "Gastrointestinal Diseases/diagnosis"[Mesh] OR "Gastrointestinal Diseases/epidemiology"[Mesh] OR "Bone Diseases"[Mesh] OR "Nervous System Diseases"[Mesh] OR "Kidney Diseases"[Mesh] OR "Muscular Diseases/diagnosis"[Mesh] OR "Muscular Diseases/epidemiology"[Mesh] OR "Immune System Diseases"[Mesh]); And in The Pediatric Infectious Disease Journal, using the free term "HIV."
Inclusion criteria included studies, review articles or case reports; written in English, Portuguese and Spanish; published between 31 July 2008 and 31 July 2016; whose population is at least 19 years old, that assessed the direct complications of HIV infection per se, or indirect complications associated with CART. Were excluded opinion articles, studies regarding socio-economic profiles of HIV-IPP with no reference to the associated outcomes, studies on molecular genetics of HIV-1 and HIV-2 virus, on risk factors and behaviors associated with HIV transmission, on socioeconomic profile and resistance profile to CART, on knowledge of young people about HIV infection, on cultural aspects of HIV and on complications in HIV-negative children exposed to HIV during pregnancy.
The pediatric age used is the one defined by WHO [19]. The epidemiological data about HIV infection used originated from WHO publication and from the Joint United Nations Programme on HIV/ AIDS (UNAIDS) [1,2,5].
Results
A total of 324 articles were identified from which 74 articles were selected that met all inclusion criteria. Figure 2 represents the article selection flowchart.
Based on the selected articles, the relevant information was collected for the review and was organised according to the type of complication (infectious vs. non-infectious) as to compose the body of the review.
Body of the Review
Infectious complications
In the absence of TARC, in early childhood, particularly in the first year of life, HIV infection is associated with rapid progression and typically presents with serious bacterial and viral infections and AIDSdefining diseases, including extra pulmonary or disseminated tuberculosis, Pneumocystis jirovecii (PJ) pneumonia, HIV-associated encephalopathy and refractory candidiasis [3,6,9]. The incidence of pneumonia by PJ is highest between 3 and 6 months [9]. Most of older HIV-IPP remain asymptomatic, or present common infections in their age group, but more severe, recurrent and refractory to treatment than in non-HIV-IPP. [3,6,9]. According to a Chilean study of HIV-IPP, 66% of the infected children had a respiratory pathology that raised suspicion of HIV infection, namely, high respiratory tract infection, repetitive bronchopneumonias, persistent pneumonitis [6]. Opportunistic infections prevalent in adolescence are more similar to those of HIV-infected adults than those of infancy [3].
Although the introduction of CART has altered the natural course of HIV infection [13-16], HIV-IPPs continue to be more susceptible to develop severe opportunistic infections (Table 1) [9,21]. Lower respiratory tract infections (LRTI), for example, are still more frequent in HIV-IPPs than in non-HIV-IPPs [10,22]. In addition, LRTIs in HIVIPPs are associated with longer hospital stays and higher mortality rates than LRTIs in non-HIV-IPP [10,22]. A UK study showed that CART delays the first presentation of LRTI and decreases the number of total cases per year (46.1 cases of LRTI/patient-years in non-CART HIV-IPP compared with 6.4 cases of LRTI/patient-years in HIV-IPP under CART) [21].
| Type of Infections | Main Agents Reported in the Literature |
|---|---|
| Respiratory Tract | Streptococcus pneumoniae, Pneumocystis jirovecii, Mycobacterium tuberculosis [9,10,13,21,23] |
| Cytomegalovirus [6] | |
| Cryptococcus neoformans, Cryptococcus gattii [30,31] | |
| Non-tuberculous mycobacteria (Mycobacterium avium) [6, 32] | |
| Mucocutaneous | Dermatophytosis: Tinea cosporis e capitis [26] |
| Scabies (Sarcoptes scabiei var. hominis) [10] | |
| Herpes simplex virus (HSV), Herpes zoster virus (HZV) [10,26] | |
| Human papiloma virus (plantar warts) [26] | |
| Vírus do molusco (molluscum contagiosum) [25,26] | |
| Candida spp. (C. albicans, C. glabrata, C. parapsilosis e C. tropicalis) [7,8,26,33] | |
| Leishmania donovani Complex [34] | |
| Gastrointestinal | Protozoa: Cryptosporidium spp., Entamoeba spp., Giardia lamblia [9,10,33,35,36] |
| Helminths: Ascaris lumbricoides, Schistosoma mansoni, Trichuris trichiura [35] | |
| Escherichia coli enteroagregativa, enterotoxigénica e enteropatogénica [36] | |
| Candida spp. (C. albicans, C. glabrata, C. parapsilosis e C. tropicalis) [7,8,26,33] | |
| Isospora belli [6] | |
| Cytomegalovirus, HSV [33] | |
| Hepatitis A, B, C virus [10] | |
| Otorhinolaryngological | Proteus vulgaris, Pseudomonas aeruginosa [25] |
| Nervous System | Toxoplasma gondii [6,9,37,38] |
| Cryptococcus neoformans, Cryptococcus gattii [30,31] | |
| Measles vírus [39] | |
| Human lymphotropic virus type 1 [40] | |
| Cytomegalovirus, HSV [38] | |
| Mycobacterium tuberculosis [41] | |
| Urologic and Nephrological | Cryptococcus neoformans, Cryptococcus gattii [30,31] |
| Schistosoma haematobium [42] | |
| Hepatitis B, C virus, Tuberculose [43,44] | |
| Ophthalmological | Citomegalovírus, Vírus Herpes simplex (lesões retinianas) [29] |
| Hematological | Epstein-Barr vírus [45] |
| Malaria [46] |
Table 1: Major infectious complication in HIV-IPP.
The main agents referred to as etiologic causes of LRTIs in HIV-IPP are Streptococcus pneumoniae (SP), Pneumocystis jirovecii (PJ) and Mycobacterium tuberculosis (MT) [10,13,21,23]. HIV-IPPs present risk of LRTI by Bordetella pertussis when compared to non-HIV-IPP [24]. CMV infection is pointed out by Elba Wun as the main etiological cause of bronchopneumonia [6].
At the Nossa Senhora da Glória State Children's Hospital, a cohort study, which included 177 children with AIDS, found that 47.4% had recurrent bacterial infection and that 64.2% experienced at least one episode of invasive bacterial infection (pneumonia, acute bacterial meningitis or septicemia) [9].
HIV-infected adolescents are at increased risk for vaccinepreventable infections, such as rubella, hepatitis B and measles [3,21]. A retrospective cohort study conducted in the USA, which included 79 adopted HIV infected children, mostly from Africa, showed that they had inadequate immunity for measles and/or tetanus, which may be justified by lack of vaccination, inadequa, inappropte handling or storage of vaccines and by inappropriate immune response [10]. In factriate serological responses and progressive decrease of antibodies are more common in HIV-IPPs [3,10,21].
According to Taipale et al. in the Pediatric Hospital of Luanda, chronic suppurative otitis media is more prevalent in HIV-IPP, mainly between 0 and 2 years. (24%) and Proteus vulgaris (53%) and Pseudomonas aeruginosa (24%) were the main agents isolated [25]. There are references in the literature to acute otitis media and recurrent bacterial sinusitis in HIV-IPP [9].
Mucocutaneous infections are more prevalent in HIV-IPP and their severity varies with the immune status, so the most serious manifestations occur in HIV-infected patients who are more immunodepressed [26].
The main infections are impetigo; molluscum contagiosum; plantar warts associated with Human papiloma virus (HPV) infection; dermatophytosis (Tinea corporis and capitis); and herpes infections by HSV and VHZ [6,9,10,21,25,26] The presence of multiple body lesions due to dermatophytosis or tinea unguium may be indicative of a state of severe immunodeficiency [26].
HIV-IPPs often present oropharyngeal lesions caused by HSV [6,27]. HSV2 and HIV co-infection is associated with increased recurrence. [9,28] In addition, there is a reference to retinal HSV and CMV infections [29].
Candidiasis is common in HIV-IPPs with CD4 cell counts (CD4cc) <400 cells/mL and appears to be one of the first manifestations of HIV infection [7,8]. The main agent isolated is Candida albicans , but C. glabrata , C. parapsilosis and C. tropicalis have also been isolated [7]. Oral candidiasis is associated with elevated viral load and may progress to esophageal and/or systemic candidiasis if not diagnosed early [7,8,26,30-33] Furthermore, it is generally a recurrent infection and therefore requires oral systemic antifungal treatment [8,26].
Noma (cancrum oris) is described by Masipa et al. in an HIVinfected 6 year old boy with no CART, referred to Polokwane Hospital in Limpopo for destructive mid-facial injury. Noma is characterized by being necrotizing and disfiguring and is associated with high mortality in the absence of treatment. Anaerobic bacteria are the responsible agents and their pathogenesis in HIV-IPPs needs investigation [34-47].
In VIH-IPP parasite infections are associated with chronic gastrointestinal pathologies, contrasting with the immunocompetent children, who usually present acute and self-limited episodes. [6,10,35,36] The main protozoa are Cryptosporidium spp., Entamoeba spp., Giardia lamblia [10,35,36] and the main helminths are Ascaris lumbricoides , Schistosoma mansoni , Trichuris trichiura [35].
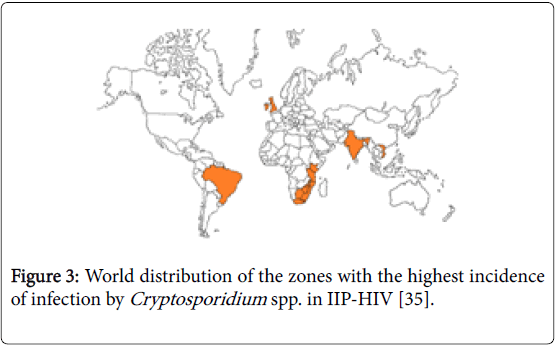
Chronic giardiasis is common in HIV-IPP with suppression of the immune response and is associated with malabsorption and, consequently, with non-therapeutic levels of CART and so giardiosis should be screened in all HIV-IPPs, even in asymptomatic patients [10]. In Brazil, South Africa, Kenya, Malawi, the United Kingdom, Vietnam, Tanzania and India, Cryptosporidium spp. has a higher incidence in HIV-IPP and is a cause of considerable morbidity and mortality (Figure 3) [35].
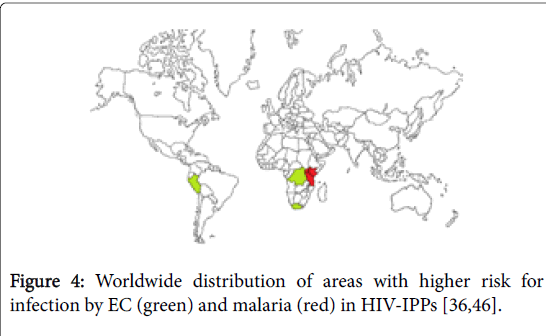
Enteroaggregative, enterotoxigenic and enteropathogenic Escherichia coli (EC) are often isolated and are associated with acute diarrhea in HIV-IPPs in Peru, South Africa and Zaire (Figure 4) [36].
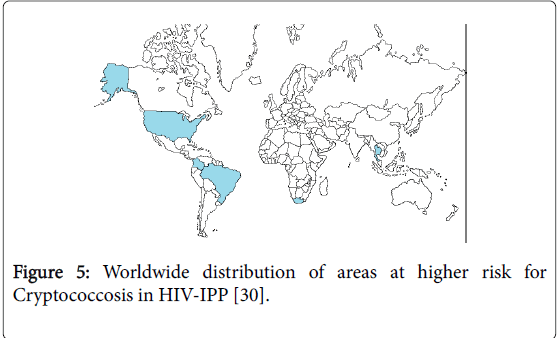
Cryptococcosis is a fungal infection, which particularly affects HIVIPP with states of severe immunosuppression [30,31]. In South Africa, Colombia, Brazil, the United States of America (USA) and Thailand, the incidence of cryptococcosis varies between 0.85 and 32% (Figure 5). [30] The most common strains are Cryptococcus neoformans (CN) and Cryptococcus gattii [30,31] and are associated with high mortality [13]. The main organs affected are the central nervous system (CNS), lung, skin and kidney [48]. Renal attainment is poorly characterized in the literature. However, cryptococcal pyelonephritis can be dramatic and fatal [48].
HIV-EBV co-infection is associated with chronic stimulation of B cells and consequent expansion of EBV-infected B cells, which adds to the risk of neoplasms associated with EBV infection (see neoplastic complications). CART counteracts this super infection, thereby reducing EBV viremia and neoplastic risk. There are two types of EBV: type I is most prevalent in the Caucasian and Southeast Asian populations, while type II is most prevalent in Africa and New Guinea. In Uganda, non-CART HIV-IPPs is more likely to have a coinfection with the 2 types of EBV than children under CART [45].
The prevalence of HIV and HBV co-infection is lower in the pediatric population than in the adult population [49] being the major risk factors adolescence, elevation of liver enzymes, stage 3 and 4 of the WHO HIV infection [50]. The synergism between HIV and CHB accelerates the progression of liver disease secondary to infection and increases the risk of chronic HBV infection [50,51].
Urogenital schistosomiasis has been associated with HIV infection in adolescents, the main agent being Schistosoma haematobium [42].
According to the WHO, there are 10 million cases of tuberculosis annually, 15% of which correspond to TB-HIV co-infection [32]. In the United States and the United Kingdom, the incidence of HIVtuberculosis co-infection in the pediatric population is 23 times lower than in South Africa (1:100 children-year vs. 23:100 children-year) [41]. The main risk factors for co-infection are severe immunodeficiency, age less than 2 years, CART less than 6 months and infected cohabitants [32,41]. The presentation of HIV-IPP is similar to that of non-HIV-IPP, with cavitation being uncommon [41].
Although the incidence of tuberculosis has been declining since the introduction of CART, the incidence of tuberculosis and non tuberculous mycobacterial infections, such as Mycobacterium avium , remains higher in HIV-IPPs. In Spain, hospitalized HIV-IPP has a frequency of non-tuberculous mycobacterial infections 16x higher than that of non-HIV-IPP [32].
Sub-acute sclerosing panencephalitis is a rare, progressive and destructive CNS process secondary to measles virus infection. Its prevalence is highest in developing countries, such as India and the Middle East, with 21 and 2.4 new cases per million, respectively. There is usually a history of measles during childhood and only later development of the pathology [39].
In Tanzania, Kenya and Uganda HIV-IPP are at higher risk for developing malaria (Figure 4). In Tanzania, HIV-IPP with malaria has a 28%-127% higher risk of developing a second malaria episode compared to malaria-infected non-HIV-IPP [46].
Human lymphotropic virus type 1 (HLVT-1) has characteristics similar to HIV-1, namely, trophism by CD4+ cells, geographic distribution and transmission pathways. HLVT-1 and HIV-coinfection have synergistic effects and are therefore associated with an increased risk of neurological disease caused by HLVT-1, a higher mortality rate and shorter survival. In the Federal University Hospital of Bahia, 47.30% of HIV-IPP had higher HIV-HLVT-1 co-infections and CD4cc, however, this count does not confer protection against opportunistic infections [40].
In Ethiopia and the Mediterranean area, the incidence of visceral HIV-leishmaniasis co-infection is higher in HIV-IPP with AIDS. The main etiological agents belong to the Leishmania donovani complex (L. infantum , L. donovani ). In HIV-IPP with severe immunosuppression the manifestations may be atypical, that is, the dermatotropic species may affect viscera and the viscerotropic can assay themselves to the skin, causing disseminated cutaneous leishmaniasis [34].
Non-Infectious Complications
Mucocutaneous complications
Cutaneous manifestations may affect more than 90% of HIV-IPPs [26], are usually multiple and have an atypical or severe presentation and may be frequent or resistant to treatment [52].
The main cutaneous complications reported in the literature are dermatitis, namely diaper-associated dermatitis, seborrheic dermatitis, atopic dermatitis and chronic eczema [6,9,10,25,52]. In the study by Moreira-Silva et al. 43.1% of HIV-IPP had dermatitis [9].
Mucocutaneous manifestations predominantly affect adolescents, in the form of recurrent rash, in association with other manifestations, such as pruritus papular eruption, angular cheilitis, contagious molluscum, diffuse plantar wart, oral thrush [3,26]. Skin lesions are intimately related to the degree of immunosuppression. As the main rash triggers we have the drugs, namely cotrimoxazole, ampicillin and nevirapine [26].
Endocrinological complications
Decreased bone density is a worldwide prevalent metabolic complication among HIV-IPPs, especially after the introduction of CART. HIV infection and CART act on the bone formation process and cause a decrease in bone density, which confers an increased risk of early osteoporosis in adolescence [3,14,57].
Hypovitaminosis D is common in HIV-IPP and its prevalence ranges from 18% to 93% [13].
HIV IIPs show a pattern of slow growth and pubertal delay [3,10,20,57,66,67] that correlate with immunosuppressive states, opportunistic infections and malnutrition [3,10,67]. Low weight-forage at the introduction of CART, together with poor growth in the first few months after introduction of CART, is an indicator of disease progression and increases the risk of IRS [71]. CART is a protective factor , which when introduced early improves growth and reduces pubertal delay [66,72].
Hyperlactacidemia due to mitochondrial dysfunction caused by HIV infection per se or by CART, especially protease inhibitors (PI) and nucleoside reverse transcriptase inhibitors (NRTIs) is described in the literature. Its clinical condition is usually non-specific, with gradual or fulminant installation with organ dysfunction. The diagnosis is made by serum lactates >5 mmol/L and increased anionic metabolic gap [14].
Metabolic changes are increasing due to HIV infection per se and CART, with the main changes being: metabolic syndrome (MS), altered body fat (BF) distribution, subclinical hypothyroidism [20].
Typical changes in puberty may mask changes in BF distribution [20]. Abnormal BF distribution increases the risk of insulin resistance, dyslipidemia and lactic acidosis. [14,57,65,69].
Lipodystrophy syndrome is classified into 3 entities, namely lipoatrophy, which is characterized by loss of subcutaneous adipose tissue of the face, buttocks and extremities, making the veins prominent; Lipohypertrophy, which is characterized by increased waist circumference, "buffalo neck", mammary hypertrophy in girls and gynecomastia in boys; And mixed. The risk factors for developing this syndrome are dose and duration of CART, PI (lopinavir, ritonavir), NRTI (stavudine, zidovudine, efavirenz), age (older children), HCV co-infection, puberty, high body mass index and rapid immune recovery [17,57,65,68,69].
MS is an independent risk factor for cardiovascular disease and is characterized by hypertension, dyslipidemia, obesity and hyperglycemia [3,20,65].
The prevalence of arterial hypertension in HIV-IPP is higher than the general population (19.6% vs. 17.7%) [73].
Dyslipidemia is also a complication frequently encountered in HIVIPP [57,58] and the main risk factors are cumulative effect of CART, especially ritonavir, stavudine and efavirenz [58,68,74]; Lipohypertrophy and HIV per se [14,20,68,74] HIV-IPP with MS or under CART, especially PI, have low levels of HDL and high levels of triglycerides, VLDL and total cholesterol [20,57,65,68,75]. In addition, male sex, lipoatrophy and altered BF distribution are associated with increased triglycerides [57,58,74].
Insulin resistance is increasing in HIV-IPPs [20,57,74] and the risk factors are CART (PI and thiamine analogs), high body mass index, advanced stage of HIV infection, HIV-HCV co-infection, family history, dyslipidemia, puberty, old age. Despite this, diabetes and hyperglycemic states are rare [14,68].
Although clinical hypothyroidism is poorly described in the literature in HIV-IPP, subclinical hypothyroidism is common, especially in patients with moderate to severe immunosuppression and is characterized by an increase in TSH with normal T4 and T3. There is an inverse correlation between CD4cc and TSH [57].
The "euthyroid patient syndrome" is more frequent in severe immunosuppression and in the lower CD4cc and consists in the reduction of the conversion of T4 in T3, with accumulation of T4 and increase of the T4 conversion in reverse T3 [57].
Dysregulation of the hypothalamic-pituitary-adrenal axis is common in HIV-IPP and may lead to adrenal insufficiency [57].
Cardiovascular complications
There is increasing evidence that there is a risk of premature cardiovascular disease (CVD) in HIV-IPP with infection acquired through mother-to-child transmission [14].
In the pre-CART period, 25% of the HIV-IPP had left ventricular hypertrophy (LVH) and/or left ventricular dysfunction (LVD). Cardiac pathology was typically fulminant, due to myocarditis, pleural effusions, pulmonary hypertension or arrhythmias [14,17].
After the introduction of CART, several studies between 2004 and 2016 refer to CVD, especially early atherosclerosis in children, arterial stiffness, thickening of the intimal layer of the arteries, coronary arteriopathy, cardiomegaly, LVD, low ejection fraction, LVH, dilated cardiomyopathy [3,11,14,17,57,58]. There is scientific evidence that increased serum biomarkers, such as C-reactive protein, vascular-1 cell adhesion molecules, intercellular adhesion molecule, interleukin-6, are an increased risk for CVD [14,17,58].
Respiratory system complications
The non-infectious complication of the respiratory system most common in HIV-IPP, but rare in the adult population is interstitial lymphocytic pneumonitis (IBD), which in the long term may progress to cor pulmonale and/or bronchiectasis [3,6,9]. This pathology responds to CART, so its frequency has decreased since its introduction [3,9]. In the retrospective cohort study conducted at the Nossa Senhora da Glória State Infant Hospital, which included HIVIPP referenced between 2001 and 2011, 19.5% of HIV-IPPs had IBD and was more frequent in children younger than 2 years old [9]. Bronchiolitis obliterans is another non-infectious respiratory complication, which, unlike IBD, does not respond to CART [3].
Neurological complications
HIV is neurotrophic and may lead to severe changes in the CNS of HIV-IPP, especially in states of immunosuppression. The main disorder reported is HIV-associated progressive encephalopathy [3,6,9,15,37,59,60]. However, with the introduction of CART, its incidence has declined dramatically. [12,37,60]
HIV-IPPs, which have low CD4+, high viral load or acquired infection by mother-to-child transmission, often have cognitive deficits, delayed neurological development (language, motor skills, verbal reasoning, spatial integrative visual ability, memory) and behavioral disorders (aggressive behaviors, attention deficit, difficulties in interpersonal relationships, sleep disorders), psychiatric disorders (posttraumatic stress disorder, depression, hyperactivity disorder and attention deficit) and motor disorders. The deficits appear to increase throughout childhood [3,10,15,37,59,60] and decrease with the early introduction of CART [3,6,12,37,59,60]. Memory deficiency mainly consists of the inability to acquire new verbal and visual information. The recognition memory is not affected [15].
Stroke is a recognized complication of HIV infection, particularly in HIV-infected patients whose transmission route was mother-to-child and its incidence in the pediatric age ranges from 1.3 to 2.6%. Ischemic accidents are the most common (73%) and are located in the cerebral cortex, basal ganglia and internal capsule. Hemorrhagic accidents are essentially intracerebral [16].
In the pre-CART period and currently in developing countries with reduced access to CART, stroke is attributed to opportunistic infections by VZV, CMV, SP, CN, MT, Haemophilus influenzae ; and neoplasms (primary CNS lymphoma or disseminated Kaposi sarcoma (KS)). To date, there have been no reported cases of stroke associated with adverse effects of CART in pediatric age [16].
HIV-associated cerebral vasculopathy is more common in patients with low CD4cc and high viral load. This pathology mainly affects medium-sized cerebral vessels. The patient may remain asymptomatic, or may develop encephalopathy, cognitive disorders, or stroke [16].
Convulsions are common in HIV-IPP due to focal cerebral cortical lesion, of infectious or neoplastic etiology. However, it is rare as an initial symptom. Ramanujam et al. reported the case of a 14 year old boy diagnosed with HIV infection as a consequence of CMV encephalitis who presented as continuous partial epilepsy [61].
Jadhav et al. described, for the first time, acute motor axonal neuropathy (Guillian Barré Syndrome variant) in an 11 year old girl infected with HIV. Peripheral neuropathies are uncommon in HIVIPP, but inflammatory demyelinating neuropathies are known to be associated with acute seroconversion, whereas distal sensory neuropathies are associated with progressive immunosuppression [62].
Nephrological complications
Regardless of the stage of HIV infection, renal disease (RD) is a common complication in the pediatric age, with an incidence of 0.26-2.6 episodes per 100 patient-years and therefore its screening HIV-IPP is recommended [18,43,44,64]. The risk of RD increases with age, low CD4cc, high HIV viral load, tenofovir, HCV and/or HBV coinfection and in the African population with mutation of MYH9 and/or APOL1 [3,18,43,64].
The major RDs reported in HIV-IPP are HIV-associated nephropathy (HIV-N) and immunocomplex-mediated RD (ICRD). [43,44,48] These pathologies progress to chronic RD in 5-40% of HIVIPP. [44,64] Prior to the introduction of CART, 50% of the chronic conditions were HIV-N, but the tenofovir proximal renal toxicity is changing this paradigm. [3,14,18,43,44,64]. Tenofovir can cause acute tubular necrosis, Fanconi's syndrome, nephrogenic diabetes insipidus, hyperphosphatemia and proteinuria. [14,43,44,64] Although there is association with proteinuria, there is usually no progression for CKD [14].
HIV-N is characterized by a nephrotic syndrome associated with acute kidney failure [43,44] and proteinuria, that presents from 8 months to 3 years before end-stage kidney disease. [44,64] The main findings in kidney biopsy is focal segmental glomerulosclerosis [43,44] while mesangioproliferative lesions and the histologic pattern of “ball in cup” appearance are characteristic of immunocomplex-mediated renal disease [43,44].
Acute tubular necrosis is a acute kidney injury associated with urinary tract infections in HIV-IPP that are undernourished, with sepsis or diarrhea and under treatment with tenefovir [14,43,44,64].
HIV-associated thrombotic microangiopathy is another complication reported in literature. [43,44,48].
The main hydroelectrolytic disorders in HIV-IPP reported in literature are gastroenteritis associated hyponatremia, hypernatremia, severe malnutrition or gastroenteritis associated hypocalcemia, hyperphosphatemia, hypophosphatemia, hypocalcemia and hypomagnesemia. Syndrome of inappropriate antidiuretic hormone secretion, mostly associated with PJ infections, lactic acidosis associated with sepsis or drug toxicity and metabolic acidosis with normal anion gap, associated with diarrhea or drug nephrotoxicity and consequent loss of bicarbonate were also described [44,48].
Gastrointestinal complications
The main gastrointestinal presentations are summarized in Table 2 [4,6,9,10,33,49].
Chronic diarrhea is reported in many studies as a common symptom in HIV-IPP [4,6,9,10] in developing countries, mostly in regions with no access to CART [36] and is the main cause of morbidity and mortality [4,6,10]. Eijk et al. found that diarrhea associated with fever and malnutrition was more common in HIV-IPP than in non-HIV-IPPs. Diarrhea was identified as the cause of death in 37.8% of HIV-IPP [4].
| Complications | Main complications Reported in the Literature | |
|---|---|---|
| Mucocutaneous | Dermatitis [6,9,10,52] | Diaper-associated dermatitis |
| Seborrheic dermatitis | ||
| Atopic dermatitis | ||
| Chronic eczema | ||
| Drugs-associated rash [26] | ||
| Pruritus papular eruption [3,26] | ||
| Angular cheilitis [3,26] | ||
| Kaposi’s Sarcoma (KS) [3,6,53] | ||
| Leiomyosarcoma [54-56] | ||
| Cardiovascular | Left ventricular hypertrophy and dysfunction [14,17] | |
| Myocarditis, pleural effusions, pulmonary hypertension, arrhythmias [14,17] | ||
| Early atherosclerosis, arterial stiffness, thickening of the intimal layer of the arteries, coronary arteriopathy, cardiomegaly, low ejection fraction, dilated cardiomyopathy [3,11,14,17,57,58] | ||
| Respiratory Tract | Interstitial lymphocytic pneumonitis [3,6,9] | |
| Cor pulmonale [3,6,9] | ||
| Bronchiectasis [3,6,9] | ||
| Bronchiolitis obliterans [3] | ||
| Leiomyosarcoma [54-56] | ||
| Nervous system | HIV-associated progressive encephalopathy [3,6,9,15,37,59,60] | |
| Delayed neurological development [3,10,15,37,59,60] | ||
| Behavioral, psychiatric and motor disorders [3,10,15,37,59,60] | ||
| HIV-associated cerebral vasculopathy [16] | ||
| Stroke [16] | ||
| Convulsions [61] | ||
| Peripheral neuropathy [62] | ||
| CNS lymphoma [53-56] | ||
| Gastrointestinal | Hepatosplenomegaly [4,6,9,10,33,49] | |
| Chronic or recurrent [4,6,9,10,33,49] | ||
| HIV-associated Hepatitis [4,6,9,10,33,49] | ||
| Wasting Syndrome [4,6,9,10,33, 49] | ||
| Body weight loss greater than 2 percentiles in 2 measurements performed with a 30-day interval [4,6,9,10,33,49] | ||
| Pancreatitis [4,6,9,10,33,49] | ||
| Hepatotoxicity [4,6,9,10,33,49] | ||
| Leiomyosarcoma [54-56] | ||
| Anal intraepithelial cancer [63] | ||
| Urogenital and Nephrological | HIV-associated nephropathy [43,44,48] | |
| Immunocomplex-mediated renal disease [43,44,48] | ||
| Tubular dysfunction with hydroelectrolytic disorders [44,48] | ||
| HIV-associated thrombotic microangiopathy [43,44,48] | ||
| Drugs toxicity [43,44,48] | Drug-induced crystal nephropathy (indinavir, nelfinavir, atazanavir, acyclovir, sulfadiazina) | |
| Fanconi Syndrome (lamivudine, abacavir, didanosine) | ||
| Tubulopatia distal: Anfotericina | ||
| Acute tubular necrosis [14,43,44,64] | ||
| Tenofovir proximal renal toxicity: acute tubular necrosis, Fanconi's syndrome, nephrogenic diabetes insipidus, hyperphosphatemia and proteinuria [14,43,44,64] | ||
| Cervical cancer [3,53] | ||
| Nephroblastoma [54] | ||
| Otorhinolaryngological | Hearing impairment [25,28] | |
| Cervical lymphadenopathy [25] | ||
| Oral hairy leukoplakia, linear gingival erythema, necrotizing ulcerative gingivitis, delayed eruption of primary teeth [7,8,25] | ||
| KS [3,6,53] | ||
| Non-Hodgkin's lymphoma [3,6,45,53] | ||
| Dental caries [7,8] | ||
| Ophthalmological | Microangiopathy associated with HIV infection [29] | |
| Retinal phlebitis, mean uveitis [29] | ||
| Endocrinological | Metabolic syndrome [3,20,65] | |
| Decreased bone density [3,14,57] | ||
| Hipovitaminose D [13] | ||
| Stunting [3,10,20,57,66,67] | ||
| Pubertal delay [3,10,20,57,66,67] | ||
| Hyperlactacidemia [14] | ||
| Lipodystrophy Syndrome [17,57,65,68,69] | ||
| Subclinical hypothyroidism [57] | ||
| Hematological | Chronic anemia [9,49,70] | |
| Neutropenia [8-10] | ||
| Thrombocytopenia [8-10] | ||
| Leukopenia [8-10] | ||
| Lymphadenopathy [8-10] | ||
| Non-Hodgkin's lymphoma (diffuse B-cell type) [3,6,45,53] | ||
| Hodgkin's lymphoma [53-56] | ||
| Acute leukemia [53-56] | ||
| Burkitt's lymphoma [3,6,45,53] | ||
Table 2: Major complications non-infectious in HIV-IPP.
Chronic diarrhea is more frequent in HIV-IPP, mostly in AIDS stage and is secondary to enterocyte change by HIV per se (HIV enteropathy), by CART, by opportunistic infections or by gastrointestinal neoplasms [4,36].
HIV infection per se, along with systemic opportunistic infections, neoplasms, severe anemia and hepatotoxic drugs are frequent causes of high levels of hepatic transaminases [33,49]. Elevation of transaminases levels is a particular problem in developing countries, where most HIV-IPP CART regimens include non-nucleoside reverse transcriptase inhibitors, which have known hepatotoxicity [49].
Otorhinolaryngological complications
Hearing loss (HL) affects between 20% to 33% HIV-IPP [25,38]. Sensorineural HL is the most common and seems to be associated with advanced stages of HIV infection [38]. Conductive HL is also described [38]. Chronic Otitis media is considered as a possible cause of HL [10,38].
Cervical lymphadenopathy, mainly in upper jugular, submandibular, submental and posterior cervical zones is common in HIV-IPP [25].
Oral lesions afect about 10% of HIV-IPP and they can be the first clinical manifestation of HIV infection. The major risk factors are severe immunosuppression, CD4cc<200 cells/mm3, viral load>10 000 copies/mL, xerostomia and poor oral hygiene. CART contributes significantly for the reduction of oral lesions in HIV-IPP [7,8]. The main oral lesions are summarized in Table 2 [7,8,25].
Dental cavities are a common finding in HIV-IPP and its prevalence, besides being inversly proportional to the patients’ immune state, varies with age, with about 9% en HIV-IPP<2 years old and 71% in HIV-IPP>5 years old. [8,25] Xerostomia and use of sucrose-based medication (antibiotics, antifungal, zidovudine) are the main causes of high prevalence of dental cavities in HIV-IPP [7,8].
Ophthalmological complications
Ophthalmological manifestations are common in HIV-IPP, mostly associated with infectious disorders. The leading non-infectious complication reported in literature is HIV microangiopathy with cotton-wool spots and hemorrhage at funduscopic examination [29].
Westland et al. described a case of peripheral retinal phlebitis and mild uveitis, in a 11 years old boy infected with HIV, born in Senegal, that presented with visual impairment, mainly for distant vision [29].
Hematological complications
Most of hematological morbidity in HIV-IPP corresponds to anaemia and is associated with advanced stages of HIV infection and low CD4cc [9,49,70]. Chronic anemia is more prevalent in HIV-IPP between 0 and 5 years old [9,70]. Some studies suggest bone marrow suppression as the main physiopathological mechanism [9]. Anaemia is an independent negative prognostic factor, associated with high mortality and progression to AIDS. The main types of anemia described in literature are microcytic-hypochromic, normocytichypochromic and normocytic-normochromic anaemia [70]. Other hematological disorders described include neutropenia, thrombocytopenia, lymphadenopathy and leukopenia [8-10].
Neoplasic complications
The risk of developing neoplasms is higher in HIV-IPP [53-56] and it increases if CD4+ cells percentage is below 15% and in severe and long term immunosuppression states. [3,53,54] Increase in survival with CART caused a higher period of exposure to HIV infection, which predisposes HIV-IPP to preneoplastic lesions which, in turn, grants higher risk of developing neoplasms in adolescence and early adulthood [3,6,53,54].
The 3 AIDS-defining neoplasms are KS, Non-Hodgkin’s lymphoma (NHL) and Cervical cancer and they are associated with Human Herpesvirus 8, EBV and HPV, respectively [53]. After the introduction of CART there was a decrease in the incidence of these neoplasms. [45,54].
Non AIDS-defining neoplasms include acute leukemia, Hodgkin’s lymphoma, CNS lymphoma, Nephroblastoma and Leiomyosarcoma [53-56].
NHL, mainly diffuse B-cell type (NHL-DB) and Burkitt’s lymphoma, along with EBV-associated leiomyosarcoma (EBV-LMS) and KS are the leading neoplasms diagnosed in HIV-IPP [3,6,45,53,56].
In HIV-IPP, NHL-DB is the most common neoplasm, with preferential location in the abdomen [6,53]. Other possible locations, but less frequent, include lungs, CNS and bone marrow [6].
EBV infection is associated with various neoplasms in both immunocompetent and immunocompromised individuals. Coinfection HIV-EBV in the pediatric population increases the risk of EBV-LMS, representing the 2nd most common neoplasm in HIV-IPP. [54-56]. Diagnosis of EBV-LMS is achieved in HIV-IPP around 8 years old and the most common locations are the gastrointestinal tract, respiratory system, biliary tree, spleen, skin and adrenal glands. Mucocutaneous involvement is rare, but there are records of it in HIVIPP with EBV-LMS. The main metastatic lesions originating from EBV-LMS are located in the lungs [55,56]. Some types of lymphoma, as CNS lymphoma, NHL-DB and Burkitt’s lymphoma, are also associated with HIV-EBV co-infection (EBV-1 and EBV-2) in HIV-IPP [45,53]. HIV-IPP under CART have lower viral loads of EBV, which indicates that CART seems like a protective factor that, by controlling EBV super infection, reduces the risk of EBV-associated lymphomas [45].
KS clinical presentation varies with CD4cc, the immunosuppression state and age of HIV-IPP. Cutaneous manifestations of KS are more frequent in adolescents than in infants [3].
HIV-HPV co-infection increases the risk of developing in situ carcinoma and invasive carcinoma of the cervix, anus, vulvo-vaginal and penile. Development of preneoplastic lesions associated with HPV infection is related to severe immunosuppression states in HIV-IPP. An association between infection with serotypes 16 and 18 of HPV and anal intraepithelial cancer in a 10 year old girl, native from Angola and with HIV infection can be found in literature [63]. HPV infection in adolescents has a strong relation with cervical dysplasia and cervical cancer [3].
Immune restitution syndrome
Introduction of CART induces changes in the immune system as, for example, the recovery of CD4+ cells. IRS is a consequence of those immunological changes and it consists in a worsening of a previous opportunistic infection (paradoxical IRS) or in the development of an opportunistic infection previously undiagnosed in the first 12 months after commencing CART. The main etiologic agents involved are mycobacteria, HSV, HZV, CMV, PJ and CN (Table 3) [41,48,76,77]. Furthermore, IRS may be associated with the development of autoimmune diseases, like Graves’ Disease and Hashimoto’s thyroiditis (Table 3) [57,76].
| Complications | Etiologic Precipitants Reported in the Literature |
|---|---|
| Infectious | HSV [41,48,76,77] |
| HZV [41,48,76,77] | |
| PJ [41,48,76,77] | |
| CN [41,48,76,77] | |
| Mycobacterias: MT [41,48,76,77], Mycobacterium avium intracellulare [76] | |
| Leishmania donovani Complex [34] | |
| Immunological reaction to BCG [76] | |
| Stevens-Johnson Syndrome | Precipitating drugs: Nevirapine, efavirenz e cotrimoxazole [78] |
| Autoimmune diseases | Graves´s Disease [57,76] |
| Hashimoto’s Thyroiditis [57,76] |
Table 3: Major complications associated to IRS.
Studies performed in adult populations suggest that IRS occurs more frequently in patients with lower CD4cc when they iniciate CART and in patients with fast increases in CD4cc [76].
IRS may complicate tuberculosis with respiratory failure, cerebral tuberculomas, pleural effusion or generalized lymphadenopathy in the first 6 months after initiating CART, whereby HIV-IPP should only start CART 2 to 8 weeks after the beginning of tuberculosis treatment. [41].
Paradoxical IRS associated with disseminated tuberculosis is described by Bosse et al. in a 14 year old boy diagnosed with mild to moderate granulomatous interstitial nephritis [77].
In the study by Gkentzi et al., in London, 5.7 cases of IRS per 100 HIV-IPP were registered in the first 12 months after initiating CART. 3 deaths were imputed to IRS, associated with disseminated infection by CMV, MT or Mycobacterium avium intracellulare, with multiorganic failure. Bacillus Calmette-Guerin vaccine (BCG)-associated IRS was registered in 4 infants with immunization at birth, that manifested symptoms as axillary lymphadenopathy and ulceration in the injection site up to 10 weeks after initiating CART. This complication is coincident with viral load reduction and increase in CD4cc and is distinguished from side effects of BCG, because these side effects occur in the first 4 months after immunization, while the complication occurs 10 months to 9 years after immunization [76].
Stevens-Johnson syndrome is associated with IRS in HIV-IPP and the main medications capable of inducing it are nevirapine, efavirenz and cotrimoxazol. Clinical manifestations appear between 5 to 31 days after commencing medication with these drugs [78].
Cryptococcus infection associated with IRS includes aseptic meningitis, disseminated atypical skin lesions, suppurative lymphadenopathy, mediastinitis and also, although rarely described, renal cryptococcosis. The kidney is a potential reservoir for CN and a source for infection reactivation in IRS [48].
There are references to visceral leishmaniasis in HIV-IPP that initiated CART, which is characterized by multiple lesions similar to post-kala-azar dermal leishmaniasis [34].
Final Considerations
HIV-IPP’s survival as increased with prenatal diagnosis of HIV infection, prophylactic attitudes during pregnancy and childbirth and with early diagnosis and treatment of in uterus exposed children to HIV infection. Meanwhile, a parallel decrease in morbidity and mortality allowed HIV-IPP to reach adulthood but with higher susceptibility to develop disorders associated with prolonged exposure to HIV infection and CART.
The main complications in HIV-IPP vary with their immunosuppression state, HIV infection transmission mechanism, age at the beginning of CART and geographic location, with this last one influencing distinct exposures to various infectious agents and different access to CART and healthcare support.
Diagnosis of HIV infection can be made during the follow-up of an asymptomatic infant that was exposed to HIV during pregnancy or following an atypical clinical presentation.
In the absence of TARC, in early childhood there is rapid progression and the main complications are serious bacterial and viral infections and AIDS-defining diseases. In later infancy, the HIV-IPP remains asymptomatic until adolescence, or present common infections in this age group, but with more severity, recurrent or refractory to treatment. In adolescence, opportunistic infections are more similar to those of HIV-infected adults than those prevalent in childhood.
Although there was a decrease in opportunistic infections since the institution of CART, they continue to be more frequent and more severe in HIV-IPP than in non-HIV-IPP. Infectious agents vary according to the biological system affected, but the most reported are SP, PJ, CN, EBV, Cryptosporidium spp., Candida spp. and Mycobacteria. HIV infected adolescents also have higher risk of vaccine-preventable infections, which is justified by lack of vaccination, incorrect handling/storing of vaccines or lack of adequate immunological response. Therefore, it is important to recognize the characteristic clinical manifestations of the different infections mentioned, in order to be able to achieve early diagnosis and treatment, so that morbidity and mortality is further reduced in HIVIPP.
HIV-N, diarrhoea and chronic anaemia are typical in HIV-IPP, as is the higher risk of neoplasms, with the most prevalent being NHL and KS.
CART is a protective factor because, besides reducing the number of opportunistic infections, it has reduced the incidence of AIDS-defining neoplasms, has improved the growth and reduced the pubertal delay in HIV-IPP, has reduced also the early development of HIV-N, as well as the delayed neurodevelopment and the behavioural, psychiatric and motor disorders in HIV-IPP. Paradoxically, CART increased the risk of IRS, CVD, MS and Lypodistrophy.
Investigation and education of health professionals on comorbidities associated with HIV infection, particularly the health professionals responsible for the follow-up of HIV-IPP, is crucial to achieve early detection and consequently being able to improve the quality of life of both patients and their families.
References
- (2016) AIDS by the numbers-Aids is not over, but it can be.
- (2016) Global AIDS update.
- Lowenthal ED (2014) Perinatally acquired HIV infection in adolescents from sub-Saharan Africa: A review of emerging challenges. Lancet Infect Dis 14: 627-639.
- Van-Eijk AM (2010) Diarrhea in children less than two years of age with known HIV status in Kisumu, Kenya. Int J Infect Dis 14: 220-225.
- Get on the fast-track (2016) The life-cycle approach to HIV.
- Wu E (2015) Human immunodeficiency virus infection in children and adolescents: More of 25 years in Chile. Rev Chilena Infectol 32: 44-56.
- Martinez-Sandoval B (2012) Idiopathic ulcers as an oral manifestation in pediatric patients with AIDS: Multidisciplinary management. J Clin Pediatr Dent 37: 65-69.
- Rovaris NS (2014) Oral health status and its impact on the quality of life of children and adolescents living with HIV-1. BMC Res Notes 7: 478.
- Moreira-Silva, SF (2013) Comorbidities in children and adolescents with AIDS acquired by HIV vertical transmission in Vitoria, Brazil. PLoS One 8: 82027.
- Wolf ER (2016) Health outcomes of international HIV-infected adoptees in the US. Pediatr Infect Dis J 35: 422-427.
- Sainz T (2015) Cardiac function in vertically HIV-infected children and adolescents in the era of highly active antiretroviral therapy. Pediatr Infect Dis J 34(5): p. e125-e131.
- Lazarus JR, Rutstein RM, Lowenthal ED (2015) Treatment initiation factors and cognitive outcome in youth with perinatally acquired HIV infection. HIV Med 16: 355-361.
- Phongsamart W (2014) Long-term outcomes of HIV-infected children in Thailand: The Thailand pediatric HIV observational database. Int J Infect Dis 22: 19-24.
- Fortuny C (2015) Metabolic and renal adverse effects of antiretroviral therapy in HIV-infected children and adolescents. Pediatr Infect Dis J 34: 36-43.
- Nichols SL (2016) Learning and memory in children and adolescents with perinatal HIV infection and perinatal HIV exposure. Pediatr Infect Dis J 35: 649-654.
- Perez-Yepes C (2012) Cerebral infarction in an adolescent with AIDS: A case report. Bol Asoc Med PR 10: 54-57.
- Sims AM, Hadigan C (2011) Cardiovascular complications in children with HIV infection. Curr HIV/AIDS Rep 8: 209-214.
- Deyà-Martínez À (2016) Cystatin C: A marker for inflammation and renal function among HIV-infected children and adolescents. Pediatr Infect Dis J 35: 196-200.
- Organization WH (2016) Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach.
- Espiau M (2016) Metabolic syndrome in children and adolescents living with HIV. Pediatr Infect Dis J 35: 171-176.
- Payne H (2015) Incidence of pneumococcal and varicella disease in HIV-infected children and adolescents in the United Kingdom and Ireland. Pediatr Infect Dis J 2015. 34: 149-154.
- Cohen C (2015) Epidemiology of viral-associated acute lower respiratory tract infection among children <5 years of age in a high HIV prevalence setting, South Africa, 2009-2012. Pediatr Infect Dis J 34: 66-72.
- Graham SM (2011) Impact of human immunodeficiency virus infection on the etiology and outcome of severe pneumonia in Malawian children. Pediatr Infect Dis J 30: 33-38.
- Muloiwa R (2016) Incidence and diagnosis of pertussis in South African Children hospitalized with lower respiratory tract infection. Pediatr Infect Dis J 21: 41-45.
- Taipale A (2011) Otorhinolaryngological findings and hearing in HIV-positive and HIV-negative children in a developing country. Eur Arch Otorhinolaryngol 268: 1527-1532.
- Umoru D (2012) Mucocutaneous manifestation of pediatric human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) in relation to degree of immunosuppression: A study of a West African population. Int J Dermatol 51: 305-312.
- Zuckerman R (2015) HSV oropharyngeal shedding among HIV-infected children in Tanzania. Int J Std AIDS 26: 456-61.
- Sudenga SL (2012) Incidence, prevalence and epidemiology of herpes simplex virus-2 in HIV-1-positive and HIV-1-negative adolescents. Sex Transm Dis 39: 300-305.
- Westland T (2015) Case report: An 11 year old girl presenting with asymptomatic retinal vasculitis leading to diagnosis of HIV-1 infection. AIDS 29: 1901-1902.
- Lizarazo J (2014) Cryptococcosis in Colombian children and literature review. Mem Inst Oswaldo Cruz 109: 797-804.
- Nyazika TK (2016) Cryptococcal meningitis presenting as a complication in HIV-infected children: A case series from sub-Saharan Africa. Pediatr Infect Dis J 25: 36-40.
- Jensen J (2012) Reduction in mycobacterial disease among HIV-infected children in the highly active antiretroviral therapy era (1997–2008). Pediatr Infect Dis J 31: 278-283.
- Velasco-Benitez CA (2008) Digestive, hepatic, and nutritional manifestations in Latin American children with HIV/AIDS. J Pediatr Gastroenterol Nutr 47: 24-26.
- Gelanew T (2011) Disseminated cutaneous leishmaniasis resembling post-kala-azar dermal leishmaniasis caused by Leishmania donovani in three patients co-infected with visceral leishmaniasis and human immunodeficiency virus/acquired immunodeficiency syndrome in Ethiopia. Am J Trop Med Hyg 84: 906-912.
- Samie A (2014) Parasitic infection among HIV/AIDS patients at Bela-Bela clinic, Limpopo province, South Africa with special reference to cryptosporidium. Southeast Asian J Trop Med Public Health 45: 783-795.
- Medina AM (2010) Diarrheagenic Escherichia coli in human immunodeficiency virus (HIV) pediatric patients in Lima, Peru. Am J Trop Med Hyg 83: 158-163.
- van-Arnhem LA (2013) Neurologic abnormalities in HIV-1 infected children in the era of combination antiretroviral therapy. PLoS ONE 8: 64398.
- Christopher N (2013) The prevalence of hearing impairment in the 6 months-5 years HIV/AIDS-positive patients attending paediatric infectious disease clinic at Mulago Hospital. Int J Pediatr Otorhinolaryngol 77: 262-265.
- Gowda VK, Sukanya V, Shivananda S (2012) Acquired immunodeficiency syndrome with sub-acute sclerosing panencephalitis. Pediatr Neurol 47: 379-381.
- Pedroso C (2011) Coinfection by HIV-1 and human lymphotropic virus type 1 in Brazilian children is strongly associated with a shorter survival time. J Acquir Immune Defic Syndr 57: 208-211.
- Hamzaoui A (2014) Childhood tuberculosis: A concern of the modern world. Eur Respir Rev 23: 278-291.
- Kleppa E (2015) Schistosoma haematobium infection and CD4+ T-cell levels: A cross-sectional study of young South African women. PLoS One 10: 119326.
- McCulloch MI, Kala UK (2015) Renal transplantation in human immunodeficiency virus (HIV)-positive children. Pediatr Nephrol 30: 541-548.
- Bhimma R, Purswani MU, Kala U (2013) Kidney disease in children and adolescents with perinatal HIV-1 infection. J Int AIDS Soc 16: 18596.
- Petrara MR (2014) Epstein-Barr virus load in children infected with human immunodeficiency virus type 1 in Uganda. J Infect Dis 210: 392-399.
- Ezeamama AE (2012) HIV infection and the incidence of malaria among HIV-exposed children from Tanzania. J Infect Dis 205: 1486-1494.
- Masipa JN (2013) Noma (cancrum oris): A report of a case in a young AIDS patient with a review of the pathogenesis. Head Neck Pathol 7: 188-192.
- Ramdial PK (2011) Pediatric renal cryptococcosis: Novel manifestations in the acquired immunodeficiency syndrome era. Int J Surg Pathol 19: 386-392.
- Aurpibul L (2015) Prevalence and incidence of liver dysfunction and assessment of biomarkers of liver disease in HIV-infected Asian children. Pediatr Infect Dis J 34: 153-158.
- Peebles K (2015) Pediatric HIV-HBV Co-infection in Lusaka, Zambia: Prevalence and short-term treatment outcomes. J Trop Pediatr 61: 464-467.
- Aurpibul L (2012) HIV and hepatitis b co-infection among perinatally HIV-infected Thai adolescents. Pediatr Infect Dis J 31: 943-947.
- Sturt AS (2013) Temporal trends in mucocutaneous findings among human immunodeficiency virus 1-infected children in a population-based cohort. Pediatr Dermatol 30: 451-456.
- Simard EP (2012) Long-term cancer risk among people diagnosed with AIDS during childhood. Cancer Epidemiol Biomarkers Prev 21: 148-154.
- Bohlius J (2016) Incidence of AIDS-defining and other cancers in HIV-positive children in South Africa: Record linkage study. Pediatr Infect Dis J 35: 164-170.
- Mahlobo TT, Grieve A, Loveland JA (2012) Pediatric multifocal myofibroblastic tumors with involvement of the gallbladder: HIV and Epstein-Barr virus-associated smooth muscle cell tumors. J Pediatr Surg 47: 1-4.
- Tetzlaff MT, Nosek C, Kovarik CL (2011) Epstein-Barr virus-associated leiomyosarcoma with cutaneous involvement in an African child with human immunodeficiency virus: A case report and review of the literature. J Cutan Pathol 38: 731-739.
- Loomba-Albrecht LA, Bregman T, Chantry CJ (2014) Endocrinopathies in children infected with human immunodeficiency virus. Endocrinol Metab Clin North Am 43: 807-828.
- Sonego M (2016) Dyslipidemia, diet, and physical exercise in children on treatment with anti-retroviral medication in El Salvador: A cross-sectional study. Pediatr Infect Dis J 2: 15-17.
- Ruisenor-Escudero H (2016) Nutritional and immunological correlates of memory and neurocognitive development among HIV-infected children living in Kayunga, Uganda. J Acquir Immune Defic Syndr 71: 522-529.
- Crowell CS (2014) Neurologic disease in HIV-infected children and the impact of combination antiretroviral therapy. Rev Med Virol 24: 316-331.
- Ramanujam B (2016) Epilepsia partialis continua as presenting manifestation of AIDS: A rarity. J Int Assoc Provid AIDS Care 15: 19-22.
- Jadhav S, Agrawal M, Rathi S (2014) Acute motor axonal neuropathy in HIV infection. Indian J Pediatr 81: 193.
- Zaramella M (2013) Grade 3 anal intraepithelial neoplasia in an HIV-infected African girl. Pediatr Infect Dis J 32: 254-256.
- Mitchell CD (2015) Predictors of resolution and persistence of renal laboratory abnormalities in pediatric HIV infection. Pediatr Nephrol 30: 153-165.
- Musiime V (2014) Anthropometric measurements and lipid profiles to detect early lipodystrophy in antiretroviral therapy experienced HIV-infected children in the CHAPAS-3 trial. Antivir Ther 19: 269-276.
- Williams PL (2013) Pubertal onset in children with perinatal HIV infection in the era of combination antiretroviral treatment. AIDS 27: 1959-1970.
- Ramokolo V (2014) HIV infection, viral load, low birth weight and nevirapine are independent influences on growth velocity in HIV-exposed South African infants. J Nutr 144: 42-48.
- Hillesheim E (2014) Dietary intake and nutritional status of HIV-1-infected children and adolescents in florianopolis, Brazil. Int J STD AIDS 25: 439-447.
- Alam N (2012) Body fat abnormality in HIV-infected children and adolescents living in Europe: prevalence and risk factors. J Acquir Immune Defic Syndr 59: 314-324.
- Ruhinda EN, Bajunirwe F, Kiwanuka J (2012) Anaemia in HIV-infected children: Severity, types and effect on response to HAART. BMC Pediatr 12: 1.
- Kariminia A (2014) Weight as predictors of clinical progression and treatment failure: Results from the TREAT Asia Pediatric HIV observational database. J Acquir Immune Defic Syndr 67: 71-76.
- Makadzange (2015) Clinical, virologic, immunologic outcomes and emerging HIV drug resistance patterns in children and adolescents in public art care in Zimbabwe. PLoS ONE 10: 144057.
- Chatterton-Kirchmeier S (2015) Increased prevalence of elevated blood pressures in HIV-infected children, adolescents and young adults. Pediatr Infect Dis J 34: 610-614.
- Innes S (2016) High prevalence of dyslipidemia and insulin resistance in HIV-infected prepubertal African children on antiretroviral therapy. Pediatr Infect Dis J 35: 1-7.
- Syed SS (2013) Assessment of biomarkers of cardiovascular risk among HIV type 1-infected adolescents: Role of soluble vascular cell adhesion molecule as an early indicator of endothelial inflammation. AIDS res hum retroviruses 29: 493-500.
- Gkentzi D (2014) Incidence, spectrum and outcome of immune reconstitution syndrome in HIV-infected children after initiation of antiretroviral therapy. Pediatr Infect Dis J 33: 953-958.
- Bosse KR (2013) Acute renal injury in a 14 year old with HIV/AIDS and tuberculosis. Pediatr Infect Dis J 32: 380.
- Dziuban EJ (2013) Stevens–Johnson syndrome and HIV in children in Swaziland. Pediatr Infect Dis J 32: p. 1354-1358.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 5596
- [From(publication date):
April-2017 - Dec 18, 2024] - Breakdown by view type
- HTML page views : 4762
- PDF downloads : 834