HIV Encephalitis Presenting as Epilepsia Partialis Continua
Received: 03-Sep-2022 / Manuscript No. ECR-22-53274 / Editor assigned: 06-Sep-2022 / PreQC No. ECR-22-53274 / Reviewed: 20-Sep-2022 / QC No. ECR-22-53274 / Revised: 24-Sep-2022 / Manuscript No. ECR-22-53274 / Published Date: 30-Sep-2022 QI No. / ECR-22-53274
Abstract
Seizures in HIV positive patients can be a consequence of opportunistic infections, neoplasms, or HIV encephalopathy. Most commonly, these are acute symptomstic seizures secondary to focal cortical lesions, however onset with Epilepsia Partialis Continua is extremly rare. We report case of a 21 year old boy, with nopre-morbid illnesses, presenting with Epilepsia Partialis Continua, MRI Brain showed bihemispherical cortical lesions, and was detected to be HIV positives. He showed good clinical improvement with IV Immunoglobulins and multiple Antiepileptic drugs.
Keywords
Heavy metal; Cadmium; Sensitivity; Nitrification
Introduction
Acute Symptomatic Seizures can occur in 2% to 20% of all Human Immunodeficiency Virus (HIV) infected individuals [1]. The most common underlying cause is focal cortical lesion, which etiologically can be opportunistic infections (Toxoplasmosis, Tuberculosis, Cryptococcosis), neoplastic lesion (CNS Lymphoma), and HIV encephalopathy [2]. Seizure at onset in HIV patients with Epilepsia Partialis Continua (EPC) in is a rare entity [3]. We discuss a case of 21 year old male who presented with Epilepsia Partialis Continua, and was detected to be HIV positive with significantly high HIV RNA load [4].
Case study
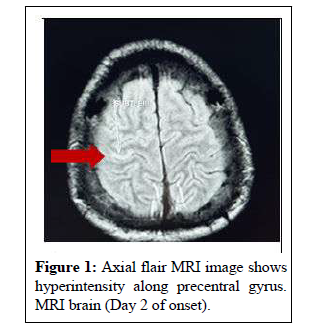
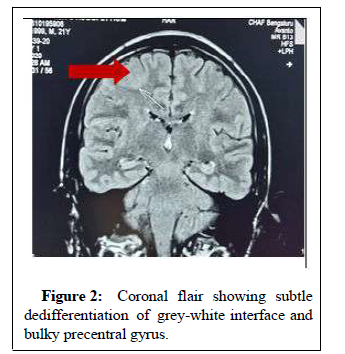
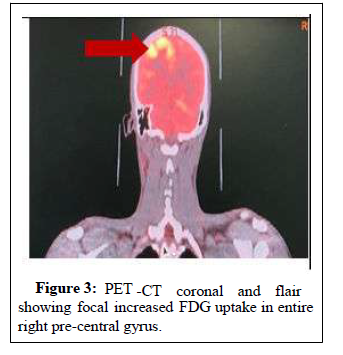
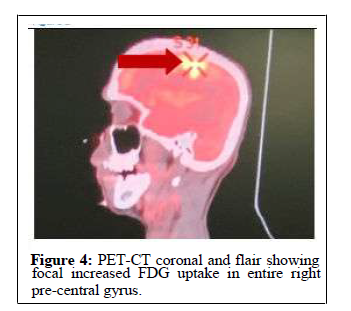
21 years male, resident of Tamil Nadu, India, right handed individual, educated upto Class 10th, unmarried and no past comorbidities [5]. He presented with history of witnessed seizure three months back [6]. Semiology of event was characterized by no preceding aura, Ictus with jerking movement of left angle of mouth and left upper limb associated with uprolling of eyeballs and tongue bite (duration of episode nearly 2 minutes), followed by post ictal phase drowsiness, post-ictal amnesia for the episode [7]. He was initially managed in peripheral hospital, wherein he continued to have repetitive, involuntary clonic-myoclonic movements of left upper limb associated with deviation of angle of mouth towards right, without impairment of sensorium [8]. He was managed at peripheral hospital with sequential Anti-epileptic drugs (Phenytoin, Levitracetam and Oxcarbazepine), with no significant reduction in frequency and severity of seizures [9]. He was thereafter transferred to Command Hospital, Bangalore for further management [10]. Initial evaluation revealed normal higher mental functions, speech characterized by hypotonic, scanning dysarthria, bilateral lower motor neuron 7th Nerve palsy left>right) and focal myoclonic jerks involving left angle of mouth and distal left upper limb with phenomenology suggestive of Epilepsia Partialis Continua (EPC) [11]. In view of the characteristic clinical profile, possibilities of Rasmussen’s Encephalitis, Autoimmune Encephalitis and Focal cortical lesions involving Right Motor Cortex were considered (Dysplasia, Space occupying lesions) [12]. He was managed with IV Immunoglobulin at 2 g/kg over five days, along with Anti-epileptic drugs (Tab Oxcarbazepine 750 mg BD, Tab Levitracetam 1.5 g BD, Tab Perampanel 6 mg OD) [13]. Initial evaluation revealed normal hemogram and biochemical parameters. MRI brain showed focal area of cortical T2/FLAIR hyperintensity in right pre-central gyrus (hand knob area) with dedifferentiation of greywhite interface and focal diffusion hyperintensity, PET-CT showed focal increased FDG uptake in same region-right Pre-central gyrus. CSF Study including Cytology, biochemistry, ADA levels, CSF for Auto-immune Encephalitis panel (Anti-NMDA, VGKC, AMPA antibodies) and CSF Biopanel (PCR for HSV, CMV, EBV, pneumococus) was Negative. He was detected to have HIV ELISA Positive, with HIV RNA load of 163771 IU/ml, CD4 T cell count of 95 cells/cmm. EEG showed Right Fronto-central spike and wave discharges, occurring periodically at frequency of one Hz with phase reversal at C4 (Figures 1-4).
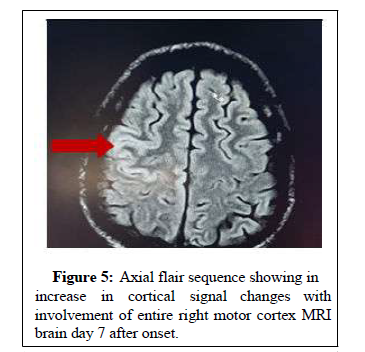
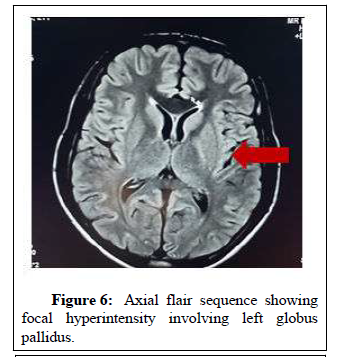
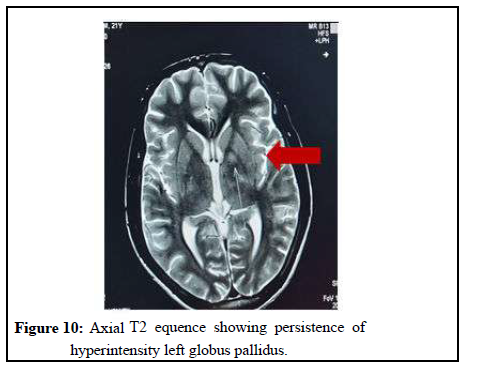
At Day 7 days, he had worsening in severity of seizures, with progression to status epilepticus (bilateral upper and lower limb myoclonic jerks and deterioration of sensorium). This necessitated endotracheal intubation, mechanical ventilation, intravenous midazolam infusion along with anti-epileptic drugs. Repeat MRI brain (Day 8) showed increase in cortical signal changes, with in the involvement of entire right motor cortex and subtle FLAIR hyperintensity in left Globus pallidus. In consideration of clinical and radiological findings, he was managed with additional IV Immunoglobulin at 1 g/kg over 02 days. During the course of hospitalizarion, he developed Aspiration Pneumonitis while on Mechanical ventilator. He was managed with culture sensitive antibiotics, AEDs and supportive management (Figures 5-8).
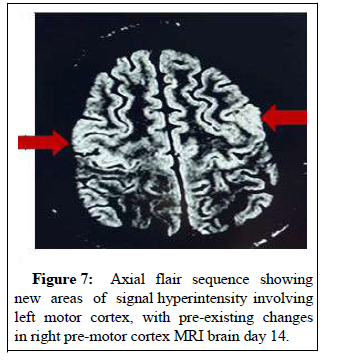
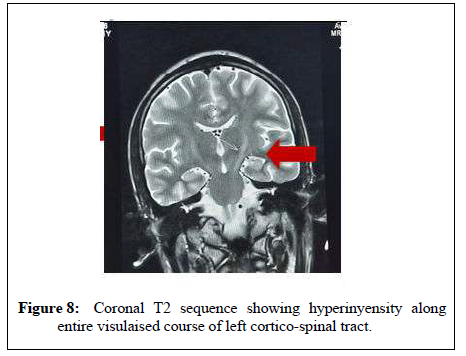
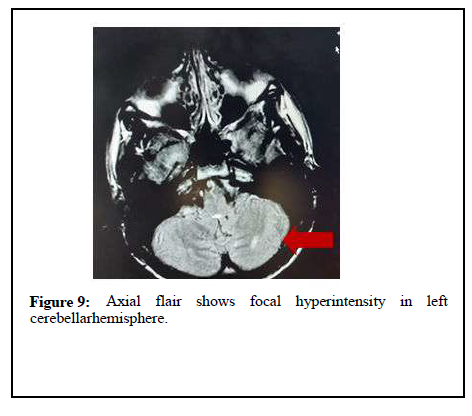
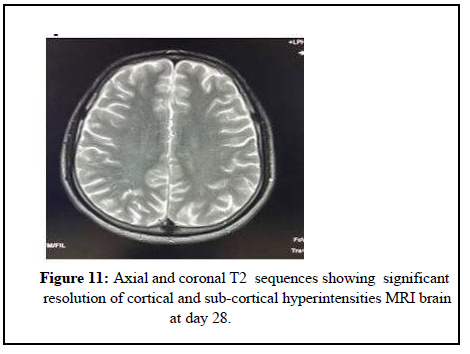
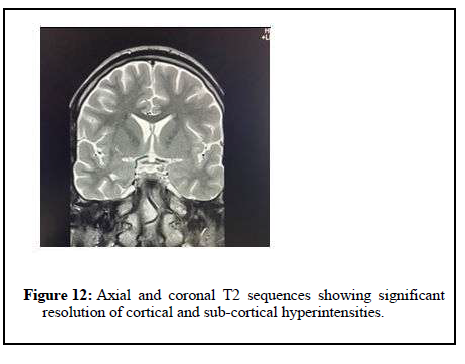
MRI brain (Day 15) showed new areas of signal abnormalities involving left motor cortex, along with T2 prolongation (with areas of diffusion restriction) along the entire course of left cortico-spinal tract. There were new discrete focal signal changes in left cerebellar hemisphere and right occipital lobe, with previously noted lesions in right motor cortex and left globus pallidus. He showed gradual clinical improvement over next one week with remission of seizures and improvement in sensorium. He was finally discharged on day 30, with advice to continue Anti-epileptic drugs (Tab Perampanel 6 mg once daily, Tab Lacosamide 200 mg twice daily, tab leviteracetam 1 gm twice daily, Tab Oxcarbazepine 750 mg twice daily), along with Anti-Retroviral treatment (Tab Tenofovir 300 mg once daily, tab lamivudine 300 mg once daily, tab efavirenz 600 mg OD), along with cap fluconazole 150 mg once daily and tab septran DS once daily. Follow-up MRI brain done at 6 weeks showed complete resolution of previously noted cortical and sub-cortical lesions in the (Figures 9-13).
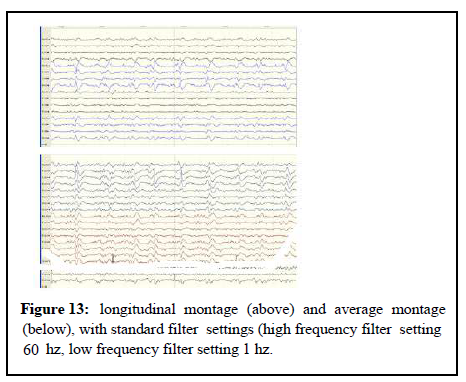
classification: Dyes iii right fronto-central region. Interpretation:Awake record showing background activity of 8-10 hz (better seen over left hemisphere). Longitudinal montage shows right frontocentral spike and wave discharges, occurring periodically at frequency of one hz with phase reversal at c4. Average montage shows epileptiform discharges with maximum amplitude at c4.
Discussion
Acute symptomatic seizures in HIV Infection has been described in 4% of HIV patients as initial presentation, and in 20.1% of HIV patients with previous neurological involvement in 8.2% among HIV patients with seizure as presentation. In the study 93.9% of patients had opportunistic infections responsible for seizures including tuberculosis, cryptococcosis and toxoplasmosis affecting the central nervous system. Epilepsia partialis continue is defined as a variant of simple focal motor status epilepticus, characterized by stereotyped, arrhythmic repetitive muscle jerks, affecting single muscles, muscle groups, an entire limb or larger parts of one hemibody continuing over prolonged periods of time. EPC has been included in subclass of focal motor status, in the ILAE task force report on status epilepticus. There are very few case studies reporting epilepsia partialis continua as the presenting symptom of HIV infection. The present case has several peculiarities, firstly this case presented epilepsia partialis continua with secondary generalization. There was worsening of sensorium with refractory status epilepticus, necessitating endotracheal intubation, IV Benzodiazepine Infusion, IV Immunoglobulins and four anti-epileptic drugs. He made uneventful clinical recovery over 3 weeks period. It have reported a case with Isolated focal mycoclonic jerks involving left upper limb with rare secondary generalization. The case was managed with prednisolone, carabamazepine and ART, and showed gradual protracted recovery over six month period, with radiological resolution 4. The other two reported case series reported no significant change in outcomes with treatment. Treatment with IV Immunoglobulins in this setting has not been previously described. Initiation of immunomodulation along with aggressive ART plays an important role in clinical profile suggestive of epilepsia partialis continua and HIV infection (Table 1).
| Author | Ferrari et al.[4] | Bartolome i et al.[5] | Ramanuja n et al.[6] | Present case | |
| Year | 1998 | 1999 | 2016 | 2021 | |
| Number | Two | One | One | One | |
| Age, years | 39 | 36 | 54 | 14 | 21 |
| Gender | Male | Male | Male | Male | Male |
| Semiology of seizure | EPC-Right UL | EPC-Left UL | EPC-distal right upper limb | Generalize d tonic clonic seizure followed by EPC involving Left half of body |
Complex partial seizure followed by EPC involving distal left upper limb |
| MRI brain | Bilateral frontal cortical and subcortical | Right frontal cortical | Left pre- central sulcus | Right parieto- occipital cortex and thalamus | Right precentral sulcus, followed by bilateral pre-central sulcus |
| EEG | Spike wave discharges- left frontal | Normal | Irregular theta rhythm over left fronto- central region | PLEDS- right fronto- central region. |
PLEDs- right Fronto- central region |
| CSF Study Cytology (per cmm, pred. cells) Protein Glucose PCR | No cells | Normal | No cells | 400, Neutrophils |
Normal |
| Normal | 68 | Normal | 120 | Normal | |
| Normal | Normal | Normal | 60 | Normal | |
| JCV + | JCV + | Negative | CMV Positive |
Negative | |
| CD4 Tcell count | 60 | 270 | - | 51 | 95 |
| HIV RNA | - | - | - | - | 163771 |
| Managem ent ART | Didanosine | Details N/A | Dideoxycyti -dine,Indin avir, |
Acyclovir, Meropenem | Tenofovir, Lamivudine , Effavirenz Perampanel, |
| AED | Clonazepam | Lamivudine Carbamaz epine | Oxcarbaze pine,Levitra cetam,Lacos amid e | ||
| Outcome | Death | Death | Improved, resolution of MRI changes | Death | Improved, resolution of MRI changes |
Secondly, sequential MRI Imaging of Brain showed progressive increase in distribution of lesions, initial imaging showing right Precentral gyral thickening, which were non-enhancing followed by signal changes in left cortico -spinal tract as well as changes in subcortical region (globus pallidus) and Cerebellar hemisphere. CSF PCR negative for HSV, CMV, JCV, pneumococus and Cryptococcus.
These lesions were Non-contrast enhancing, hyperintense on T2 / FLAIR, no significant change on T1 sequence (unlike lesions in progressive multifocal leucoencephalopathy). These signal changes have not been previously reported in HIV-related Encephalitis. HIV related cortical lesions can be due to CMV, toxoplasma, lymphoma, and PML. Previously reported case from AIIMS, EPCs were secondary to CMV-related Encephalitis in HIV (MRI brain showing signal changes in the parieto-occipital cortex and thalamus). It have reported two cases with EPC secondary to PML (proved on CSF positive for JCV PCR, and other case brain biopsy positive for JCV PCR), with MRI brain showing features of PML involving frontal cortical and sub-cortical region.
MRI imaging in CMV encephalitis is characterized by ventricular prominence, enhancement in the periventricular subependymal lining along the lateral ventricles, septum pellucidum, corpus callosum and fornices due to ventriculitis, or diffuse or patchy increased signal intensities in white matter owing to demyelination. Toxoplasma encephalitis is radiologically characterized by usually multiple ring enhancing lesions with surrounding edema, and predilection for basal ganglia. Primary CNS Lymphomas usually have solitary and multiple mass lesions with approximately equal frequency, and majority of lesions display irregular or patchy contrast enhancement. Besides, lesions larger than 4 cm in size, and with involvement of corpus callosum or peri-ventricular/periependymal areas are more likely to be lymphoma. PML usually occurs as non-contrast enhancing periventricular and subcortical, bilateral asymmetrical lesions with no surrounding edema. However, PML lesions in setting of Immune Reconstitution Inflammatory Syndrome (IRIS) associated with increase in CD4 T cell counts and drop of HIV plasma viral load on ART. In this context, PML/IRIS can present with contrast enhancement on MRI, as wellas focal edema and mass effect.
Periodic Lateralized Epileptiform Discharges on EEG in HIV patients have been described by (PLEDS over the right fronto-polar region, MRI revealing meningeal thickening along with nonspecific findings), (Aphasic status epilepticus and PLEDS on EEG, as the first presentation of AIDS-toxoplasma complex), (EPCs secondary to AIDS-associated CMV encephalitis) and (periodic lateralized epileptiform discharges in neurosyphilis and HIV Infection).
Conclusion
Cases presenting with acute onset EPC should undergo extensive evaluation, including HIV seropositivity. The present case has shown that early initiation of immunomodulation along with anti-epileptic drugs was helpful in bringing excellent clinical outcomes.
References
- Sinha S, Satishchandra P, Nalini A, Ravi V, Subbakrishna DK, et al (2005) New-onset seizures among HIV infected drug naıve patients from South India. Neurol Asia 10: 29-33.
- Sempere AP, Villaverde FJ, Martinez-Menendez B, Cabeza C, Pena P, et al (1992) First seizures in adults: A prospective study from the emergency department. Acta Neurol Scand 86: 134-138.
- Trinka E, Cock H, Hesdorffer D, Rossetti AO, Scheffer IE, et al (2015) A definition and classification of status epilepticus report of the ILAE task force on classification of status epilepticus. Epilepsi 56: 1515-1523.
- Ferrari S, Monaco S, Morbin, Zanusso G, Bertolasi L, et al (1998) HIV associated PML presenting as epilepsia partialis contonua. J Neurol Sci 161: 180-184.
- Bartolomei F, Gavaret M, Dhiver C, Gastaut JA, Gamarelli D, et al (1999) Isolated chronic epilepsia continua in an HIV infected patient. Arch Neurol 56: 111-114.
- Bhargavi R, Deepa D, Surekha D, Manjari T, Padma MVS, et al (2016) Partialis continua as presenting manifestation of AIDS: A rarity. J Int Assoc Prov AIDS Care 15: 19-22.
- Thurnher MM, Thurnher SA, Schindler E (1997) CNS involvement in AIDS: Spectrum of CT and MR findings. Eur Radiol 7: 1092-1097.
- Montaya JG, Remington JS. Toxoplasma gondii (2000) In: Principles and practice of infectious diseases, 5th edition, MandellGL, Bennett JE, Dolin R, Churchill Livingstone, Philadelphia 2000: 2858.
- Ciacci JD, Tellez C, VonRoenn (1999) Lymphoma of the central nervous system in AIDS. Semin Neurol 19: 2013.
- Tan K, Roda R, Ostrow L (2009) PML-IRIS in patients with HIV infection: Clinical manifestations and treatment with steroids. Neurol 72: 1458.
- Cury RF (2004) Focal nonconvulsive status epilepticus associated to PLEDs and intense focal hyperemia in an AIDS patient. Seizure 13: 358-361.
- Ozkaya G, Kurne A, Unal S, Oguz KK, Karabudak R, et al. (2006) Aphasic status epilepticus with periodic lateralized epileptiform discharges in a bilingual patient as a presenting sign of ‘‘AIDStoxoplasmosis complex.’’ Epilepsy Behav 9: 193-196.
- Takagaki K, Morales MK, Vitantonio D, Berkowitz F, Bell WL, et al. (2014) Periodic lateralized epileptiform discharges (pleds) in patients with neurosyphilis and hiv infection. Clin EEG Neurosci.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Arivalagan B, Goel J, Gupta S, Singh B (2022) HIV Encephalitis Presenting as Epilepsia Partialis Continua. Epidemiol Sci 12: 458.
Copyright: © 2022 Arivalagan B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2964
- [From(publication date): 0-2022 - Feb 20, 2026]
- Breakdown by view type
- HTML page views: 2500
- PDF downloads: 464