Histopathological Characteristics of Different Parts of Surgical Specimens of Ureteropelvic Junction Stenosis
Received: 28-Nov-2022 / Manuscript No. DPO-22-81452 / Editor assigned: 30-Nov-2022 / PreQC No. DPO-22-81452 (PQ) / Reviewed: 14-Dec-2022 / QC No. DPO-22-81452 / Revised: 21-Dec-2022 / Manuscript No. DPO-22-81452 (R) / Accepted Date: 21-Dec-2022 / Published Date: 28-Dec-2022 DOI: 10.4172/ 2476-2024.8.1.213
Abstract
Background: Ureteropelvic Junction Stenosis (UPJS) is one of the main causes of hydronephrosis caused by Ureteropelvic Junction Obstruction (UPJO) , which can damage renal function in severe cases.We want to explore more possible etiologies of UPJO by means of compare the pathological features of different anatomical sites in the specimens obtained from children with UPJO caused by UPJS, in particular, differences in the number and distribution of Interstitial Cells of Cajal (ICCs),muscle and collagen.
Methods: A total of 34 surgical specimens were obtained, centered on the stenotic lesion segment as UPJ segment. A 1.5 cm range of renal pelvis tissue was taken along its upper edge and used as a normal control. A 1.5 cm area of tissue was taken from the ureteral along the lower edge of the UPJ segment for the ureteral stricture segment. Hematoxylin-eosin staining, Masson staining, and immunohistochemistry were used to observe the tissue arrangement of different parts, the number and distribution of ICCs, the muscle to collagen ratio (MC ratio). Two different physicians checked the number of cells in 9 fields of view under the microscope and calculated the mean value and the distribution of muscle and collagen was analysed using the online software ImageJ. The final results were analysed using SPSSPRO by multiple samples Friedman test and paired test.
Results: The highest number of ICCs was found in the renal pelvic segment, which was significantly different from both the UPJ segment and the ureteral stenosis segment. There was no statistically significant difference between the UPJ segment and the ureteral stenosis segment. Collagen fiber hyperplasia was most pronounced in the UPJ segment, and the muscle-to-collagen fiber ratio and collagen fiber volume differed in all three different sites.
Conclusion: In UPJO due to UPJ stenosis, the number of ICCs in the UPJ segment is reduced or even absent compared to normal tissue, but there is no significant difference with the ureteral stenosis segment. 2. When ureteral buds develop from the middle to the ends, the lesion is triggered by one of the upper ureteral segments and terminates at the ureteropelvic junction, not starting at the ureteropelvic junction.
Keywords: Hydronephrosis; Ureteropelvic junction stricture; Histopathology; ICCs; Collagen fibrosiS
Abbreviations
UPJO: Ureteropelvic Junction Obstruction; ICCs: Interstitial Cells of Cajal; RP: Segment of the Renal Pelvis; UPJ: The Ureteropelvic Junction; US: Ureteral Stricture; SD: Standard Deviation; CVF: Collagen Volume Fraction; MC: Muscle Collagen Ratio
Introduction
A large number of studies have been conducted on the etiology of UPJO at home and abroad [3]. But the reason why functional UPJO appears and will disappear without intervention in most cases is still not clear. This study aims to compare the pathological changes and differences among different parts of the tissue by observing the pathological changes in the surgical specimens of children with UPJ stenosis who underwent surgical treatment to search for possible causes of disease.
Materials and Methods
Research subject
A total of 92 children with hydronephrosis were admitted to our hospital from January 1, 2021 to November 1, 2021, aged from 15 days to 14 years, excluding children older than 7 years and younger than 3 years, with an average age of 5.3 years. Inclusion criteria were: It meets the diagnostic criteria of UPJO and has the support of auxiliary examination results such as B-ultrasound, nuclear magnetic resonance hydrography, intravenous pyelography, urological contrast-enhanced ultrasound, and so on. Only cases caused by stenosis were considered. It conforms to the surgical indications of pyeloplasty. All operations were performed by the same surgeon and assisted by the same team. The exclusion criteria were: Severe disorders of the heart, brain, lung, and other organs caused by various reasons; Complicated with systemic infection, immune system deficiency, or unstable vital signs; Patients with UPJO other than pyeloureteral junction stenoses, such as concomitant renal or ureteral calculi, ectopic vascular compression, iatrogenic stenosis, duplex kidney or ureter, ureteral polyps, and other causes, were all removed. Children with a BMI of 24 or more. According to the inclusion criteria, 34 children (28 males and 6 females) were selected as research objects.
Collection method
Dismembered pyeloplasty is the first choice for treatment. The effect of this method on relieving obstruction was immediate, and timely intervention could reduce the degree of renal impairment or further prevent its aggravation [4]. In this study all the children underwent dismembered pyeloplasty, open or laparoscopic surgery performed based on the age of the children. All children were reexamined and diagnosis and evaluation were performed, excluded the surgical contraindications.
After the anesthesia takes effect in children with open surgery, adjust the position and disinfection and sheet spreading are often prescribed. An oblique incision of approximately 3-4 cm in length was made in the 11th intercostal space on the affected side. Each layer was incised sequentially to the retroperitoneal space, the middle and lower part of the kidney, the renal pelvis, and the upper ureter were exposed free, distinct narrow genocidal junction were seen. Incised 1.5 cm along the wedge of renel pelvis, carefully judged until the normal ureteral tissue appeared. The lesion segments were not only tough but also had internal white scar feeling, dry and narrow thin cords. Therefore in this study, the lesion segment was taken as the center, the upper edge of the renal pelvis was taken as the control group, and the lower edge of the ureteral stenosis segment was also taken to study whether there was a difference of pathological changes between them. The lower pole of the kidney and the lowest point of the ureterotomy were fixed with intermittent para-position suture then reconstructed the renal pelvis [5,6]. The double J ureteral tube was inserted, and the renal pelvis was reset after the suturing was completed. One negative pressure drainage tube was disposed of in the renal fossa, and the incision was closed by suturing layer by layer. If laparoscopic pyeloplasty is selected, except for the steps and some details such as positioning, placing the stamp card, establishing pneumoperitoneum, and closing the instrument entrance after an operation, the other steps are the same as above.
Experimental method
Pathological examination methods: The surgical intervention will remove the stenotic lesion segment, therefore, from the diseased segment of the UPJ as the center, the 1.5 cm segment of the renal pelvis was taken along the upper edge and upward (as the control group), and the 1.5 cm ureteral stricture tissue was taken along the lower edge and downward. To explore the etiological mechanism by comparing the microscopic pathological characteristics of the diseased segment and the normal segment, all the specimens obtained were fixed with a tissue fixator. Used for HE/Masson trichrome staining, and immunohistochemistry to observe and evaluate the distribution of collagen fibers and ICCs [7].
HE/Masson trichrome staining follow the reagent instructions. The IHC is dewaxing and drying first. An appropriate amount of antigen repair solution EDTA was prepared and repairs the antigen.10 mg of lyophilized HRP powder was dissolved in PBS and added to the section to block. After used the diluted primary antibody then translated to the refrigerator overnight. The next day added an appropriate amount of secondary antibody. The cells were counterstained using the prepared hematoxylin rinsed in PBS, and returned to blue in distilled water and sealed by neutral gum.
The observable indicators are MC ratio (analysed by two independent observers through image color analysis). The online color extraction tool ImageJ Fiji2 was used to calculate the area of color difference in the slices and quantify the MC ratio. The red and blue area corresponds to muscles and collagen. The ratio was calculated separately and converted into a single number, and the ratio of the two was taken as the MC ratio, e.g.60%/40%, Z1.5. And the number of positive cells in IHC was counted (2 observers, double-blind evaluation, counted the target cells in 9 fields). Because CD117 is expressed in both mast cells and ICC cells, nonspecific staining should be excluded when counting.
The statistical treatment we use is statistical software SPSSPRO to analyse the data, the measurement data of MC ratio (muscle to collagen ratio) and the number of ICCs in different tissue parts. Multiple sample Friedman test and paired T test were used for data analysis.
Results
Pathological changes of the lesions and IHC
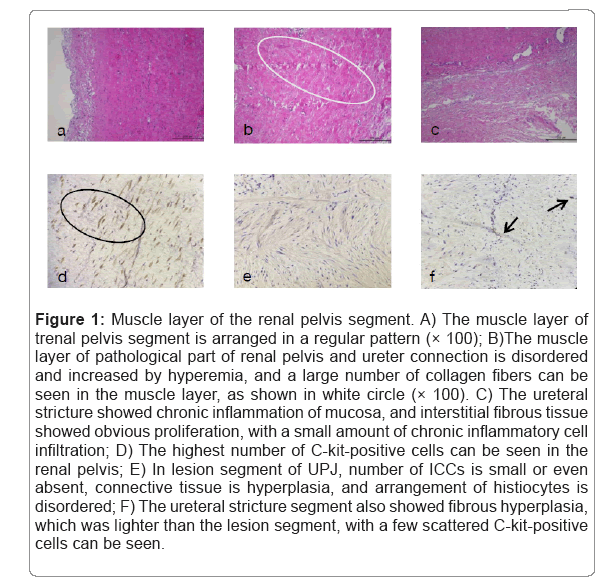
Pathological changes of the segments with HE stain and IHC in renal pelvis, the renal pelvis and ureter (UPJ), ureter stricture segments (Figures 1a-1f).
Figure 1: Muscle layer of the renal pelvis segment. A) The muscle layer of trenal pelvis segment is arranged in a regular pattern (× 100); B)The muscle layer of pathological part of renal pelvis and ureter connection is disordered and increased by hyperemia, and a large number of collagen fibers can be seen in the muscle layer, as shown in white circle (× 100). C) The ureteral stricture showed chronic inflammation of mucosa, and interstitial fibrous tissue showed obvious proliferation, with a small amount of chronic inflammatory cell infiltration; D) The highest number of C-kit-positive cells can be seen in the renal pelvis; E) In lesion segment of UPJ, number of ICCs is small or even absent, connective tissue is hyperplasia, and arrangement of histiocytes is disordered; F) The ureteral stricture segment also showed fibrous hyperplasia, which was lighter than the lesion segment, with a few scattered C-kit-positive cells can be seen.
Comparison of ICCs, muscle and collagen fibers at three sites
The proportion of muscle and collagen in specimens of different parts was obtained by image analysis software ImageJ. It was obtained by Friedman test of multiple paired samples. Significant differences were found between the RP segment vs. the UPJ segment and between the RP segment vs. the US segment, and no significant differences were found between the UPJ segment and the US segment (Table 1).
| The specimen category | Median ± SD | P value |
|---|---|---|
| Renal Pelvis | 0.5 ± 0.351 | 0.01 |
| Ureteropelvic Junction | 0.06 ± 0.024 | |
| Ureteral Stricture | 0.09 ± 0.045 |
Table 1: Muscle to collagen ratio in renal pelvic segment, UPJ segment and stenosis segment.
Masson trichrome stain
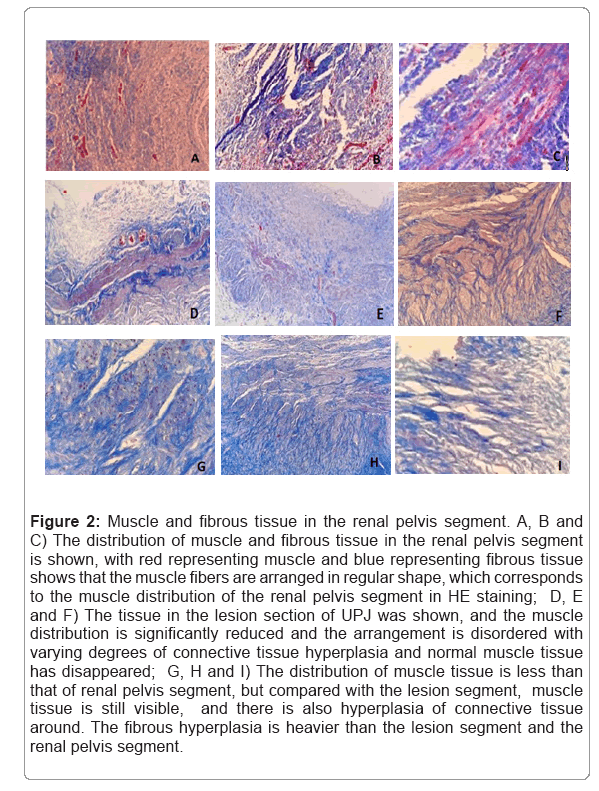
Masson trichrome stain and it’s manifestations of the renal pelvis, the renal pelvis and ureter(UPJ), ureter stricture segments (Figures 2a- 2i).
Figure 2: Muscle and fibrous tissue in the renal pelvis segment. A, B and C) The distribution of muscle and fibrous tissue in the renal pelvis segment is shown, with red representing muscle and blue representing fibrous tissue shows that the muscle fibers are arranged in regular shape, which corresponds to the muscle distribution of the renal pelvis segment in HE staining; D, E and F) The tissue in the lesion section of UPJ was shown, and the muscle distribution is significantly reduced and the arrangement is disordered with varying degrees of connective tissue hyperplasia and normal muscle tissue has disappeared; G, H and I) The distribution of muscle tissue is less than that of renal pelvis segment, but compared with the lesion segment, muscle tissue is still visible, and there is also hyperplasia of connective tissue around. The fibrous hyperplasia is heavier than the lesion segment and the renal pelvis segment.
The number of ICCs and CVF in different parts were compared
Median and standard deviation of ICCs in nine different high power fields in visible renal pelvis segment, UPJ lesion segment, and ureteral stricture segment. The results were significantly different after SPSSPPRO using Freidman test and Nemenyi test. The number of ICC cells in the renal pelvis was the most, while the distribution of UPJ lesion was the least or even absent. Collagen volume fraction CVF derived from collagen distribution in Masson trichrome stained specimens obtained by ImageJ analysis software. Using t-test analysis, the collagen volume fraction in the renal pelvis segment, UPJ lesion segment and ureteral stenosis segment were respectively different. The distribution of collagen fibers in the diseased and stenosis segments of UPJ was less different than that in the other two segments. The collagen volume fraction was the highest in the lesion segment of UPJ, and the collagen fibers were significantly proliferated (Table 2).
| Comparison between specimens | Median ± SD | P value | ||
|---|---|---|---|---|
| ICCs | RP vs. UPJ | 23 ± 4.729 | 19 ± 2.234 | 0.01 |
| RP vs. US | 23 ± 4.729 | 13 ± 2.665 | 0.01 | |
| UPJ vs. US | 4 ± 2.496 | 6 ± 0.431 | 0.07 | |
| CVF | RP vs. UPJ | 0.41 ± 0.131 | 0.365 ± 0.021 | 0.01 |
| RP vs. US | 0.41 ± 0.131 | 0.27 ± 0.079 | 0.01 | |
| UPJ vs. US | 0.775 ± 0.11 | 0.095 ± 0.058 | 0.03 | |
Table 2: Number of ICCs and collagen volume fraction between three different sites.
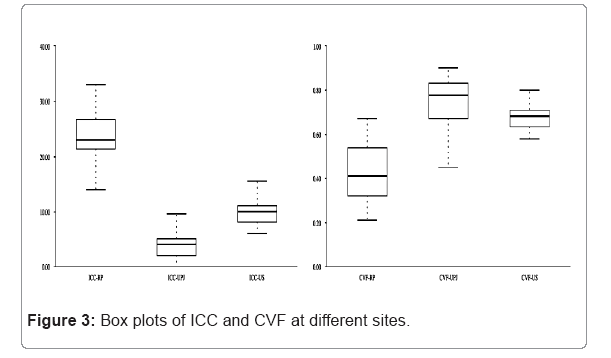
Box plots of ICC and CVF at different sites
The number of ICCs was highest in the pelvic segment and less and statistically insignificant in the UPJ and ureteral stenosis segments. The collagen volume fraction differed in all segments of the tissue (Figure 3).
Discussion
UPJO is the most common reason leading to congenital hydronephrosis in children and its etiology is complex and unclear. Among which UPJ stenosis is the most common cause. Among them, the stenosis of UPJ is the most common cause of disease. From the perspective of histopathology, some studies have found that the diseased segment of the UPJ usually has hypertrophy and disarrangement of smooth muscle, and there is a large number of collagen fiber hyperplasia between the muscles. The ICCs with pacing function distributed in the urinary tract were widely reduced in number, sparsely distributed, or even absent in the diseased segment. There were significant differences compared with adjacent normal tissues such as the renal pelvis and proximal ureter tissue, on the one hand, it was verified that the lack of ICCs in the lesion segment resulted in ineffective down-flow of urinary tract peristalsis, obstruction, and hydronephrosis [5]. As the child grows, the kidneys continue to produce urine, without timely intervention at the right time, the hydronephrosis will further expand and cause long-term compression of the nephron due to the limited space in the trunk, and there is a great risk of renal function damage, which seriously endangers the health of children.
Among the known major causes of UPJ stenosis, changes in ICCs are considered to be of great importance [8]. The number of ICCs at the UPJ is closely related to the occurrence of UPJO in children with congenital hydronephrosis. However, it remains to be elucidated why the number of ICCs at the UPJ decreases. Chronic inflammatory reactions as well as inflammatory cells infiltration were seen in most specimens. Also because the inflammatory response can promote scar proliferation, suggesting that it may promote further stenosis of the lesioned segment, early obstructive symptoms in UPJO may also be related to the presence or recurrence of urinary tract infection and the degree of inflammation.
Previous studies have focused on pathological changes in ureteral junction, but in this study, three different anatomical sites in the surgical specimens of the children were selected for comparison with each other to enrich the study, validate and explore.
34 surgical specimens were selected and divided into three parts,they were renal pelvis segment, UPJ lesion segment and ureteral stenosis segment. HE staining, Masson trichrome staining, and immunohistochemical staining were performed to explore the number and distribution of ICCs in three different parts and the distribution ratio of muscle tissue to collagen fibers. Since both ICCs and mast cells express C-kit positivity, they need to be distinguished by their morphology and have different distribution sites. ICCs are generally located at the inner edge of the circular muscle layer, parallel to the muscle fibers, shuttle-shaped, with few large nuclear cells. Mast cells are mostly found in the mucosal and submucosal layers. According to the experimental results, it can be concluded that in UPJO due to UPJ stenosis, the number of ICCs in the UPJ segment is reduced or even absent compared to normal tissue, but there is no significant difference with the ureteral stenosis segment [9]. When ureteral buds develop from the middle to the ends, the lesion is triggered by one of the upper ureteral segments and terminates at the ureteropelvic junction, not starting at the ureteropelvic junction.
The results showed that the highest number of ICCs was found in the renal pelvic segment, which was significantly different from both the UPJ segment and the ureteral stenosis segment. There was no statistically significant difference between the UPJ segment and the ureteral stenosis segment. Collagen fiber hyperplasia was most pronounced in the UPJ segment, and the muscle-to-collagen fiber ratio and collagen fiber volume differed in all three different sites. The sample size of this study is relatively small, and although the selected samples meet the inclusion and exclusion criteria, there are still biases caused by the different duration of disease and inconsistent degrees of obstruction. The wide range of deficits in the children receiving the intervention studied here; however, reliable studies have shown that age-related changes in the expression of ICCs do not alter the distribution of ICCs in UPJO [10].
Ureteral buds differentiate from the center to both ends, and previous studies focused on pathological changes at the ureteral migration of the renal pelvis, ignoring the ureteral stenotic segment that was removed together by surgery. The results of this study showed no statistical difference in the distribution of the number of ICCs between the UPJ segment and the ureteral stenosis segment, and the difference in the distribution of collagen fibers and muscle was not significant. According to the developmental orientation, the etiology of hydronephrosis due to UPJ stenosis in UPJO may be triggered by the developmental process somewhere in the upper ureter, rather than due to the pathogenesis of the first lesion in the ureteropelvic junction.
The limitations of our study are the sample size is small and the large age fraction may cause biased. There may be subjective influences when checking the number of cells, but we have try to reduce the error by making the site of the specimens is unknown to the testers. A later comparison with tissue specimens from other causes of UPJO can be made to further verify the possible etiology of this disease.
In summary, it is suggested that the etiology of UPJO due to UPJ stenosis, in addition to the need for further in-depth studies from the causative factors of decreased proliferation of ICCs, may not originate in the pyeloureteral junction but occur in the upper ureter.
Conclusion
In children with hydronephrosis caused by UPJ stenosis, the number of ICCs and the ratio of MC was the highest in the renal pelvis and was different from that in the UPJ and stenosis segments, there was no significant difference in ICCs and MC ratio between the UPJ segment and the stenotic segment. It's suggested that although clinicians are concerned about the length of the ureter and to prevent excessive tension at the suture, they should also resect the entire ureteral stricture at the lower edge of the UPJ as much as possible to ensure the removal of abnormal tissue in the ureter as much as possible and relieve the mechanical obstruction.
In UPJO due to UPJ stenosis, the number of ICCs in the UPJ segment is reduced or even a bsent compared to normal tissue, but there is no significant difference with the ureteral stenosis segment. When ureteral buds develop from the middle to the ends, the lesion is triggered by one of the upper ureteral segments and terminates at the ureteropelvic junction, not starting at the ureteropelvic junction. Chronic inflammation of the mucosa was observed in the surgical specimens. Future studies should focus on whether urinary tract infection is related to the progression of this disease.
Declarations
Ethics approval and consent to participate
Design of this study and management of patients and controls were in accordance with the Helsinki Declaration and approved by the Human Ethics Committee of the Xinjiang Medical University Affiliated First Hospital.
Competing interests
All patients or their legal custodies in their native language
Funding
This study was supported by Xinjiang Uygur Autonomous Region Natural Science Foundation Project and Xinjiang Uygur Autonomous Region Science (Grant No.2022E02047) and Technology Support Project (Grant No.2022D01A141) approved by the Department of Science and Technology of Xinjiang Uygur Autonomous Region.
Authors' contributions
All authors are involved in this study conception and design. Drafting of the manuscript by Jia Li with Nafeisha Tuerdi. Data acquisition was handled by Jia Li and Junbo Bai.Jia Li and Nafeisha Tuerdi prepared figuers and tables. Jia Li and Kaifang Liu analysis and interpretation the datas. All authors reviewed the manuscript.
References
- Yhoshu E, Menon P, Rao KLN, Bhattacharya A (2022) Outcome analysis of reduction and nonreduction dismembered pyeloplasty in ureteropelvic junction obstruction: A randomized, prospective, comparative study. J Indian Assoc Pediatr Surg 27:25-31.
[Crossref] [Google Scholar] [Pubmed]
- Babu R, Vittalraj P, Sundaram S, Shalini S (2019) Pathological changes in ureterovesical and ureteropelvic junction obstruction explained by fetal ureter histology. J Pediatr Urol 15:240.e1-240.e7.
[Crossref] [Google Scholar] [Pubmed]
- Mohammadjafari H, Rafiei A, Kosaryan M, Yeganeh Y, Hosseinimehr SJ (2014) Determination of the severity of ureteropelvic junction obstruction using urinary epidermal growth factor and kidney injury molecule 1 levels. Biomark Med 8:1199-1206.
[Crossref] [Google Scholar] [Pubmed]
- Abbas T, Elifranji M, Al-Salihi M, Ahmad J, Vallasciani S, et al. (2022) Functional recoverability post-pyeloplasty in children with ureteropelvic junction obstruction and poorly functioning kidneys: Systematic review. J Pediatr Urol 21:S1477-5131.
[Crossref] [Google Scholar] [Pubmed]
- Vemulakonda VM (2021) Ureteropelvic junction obstruction: diagnosis and management. Curr Opin Pediatr 33:227-234.
[Crossref] [Google Scholar] [Pubmed]
- Wishahi M, Mehena AA, Elganzoury H, Badawy MH, Hafiz E, et al. (2021) Telocyte and cajal cell distribution in renal pelvis, Ureteropelvic Junction (UPJ), and proximal ureter in normal upper urinary tract and UPJ obstruction: reappraisal of the aetiology of UPJ obstruction. Folia Morphol (Warsz). 80:850-856.
[Crossref] [Google Scholar] [Pubmed]
- Liu G, Liu X, Yang Y (2022) Comparative transcriptome analysis of miRNA in hydronephrosis male children caused by ureteropelvic junction obstruction with or without renal functional injury. Peer J 10:e12962.
[Crossref] [Google Scholar] [Pubmed]
- Huang ZP, Qiu H, Yang Y, Zhang L, Yang B, et al. (2016) The role of interstitial cells of cajal in acute cholecystitis in guinea pig gallbladder. Cell Physiol Biochem38:1775-1784.
[Crossref] [Google Scholar] [Pubmed]
- Mut T, Acar Ö, Oktar T, Kılıçaslan I, Esen T, et al. (2016) Intraoperative inspection of the ureteropelvic junction during pyeloplasty is not sufficient to distinguish between extrinsic and intrinsic causes of obstruction: Correlation with histological analysis. J Pediatr Urol 12:223.e1-223.e2236.
[Crossref] [Google Scholar] [Pubmed]
- Issi O, Deliktas H, Gedik A, Ozekinci S, Bircan MK, et al. (2015) Does the histopathologic pattern of the ureteropelvic junction affect the outcome of pyeloplasty. Urol J 12:2028-2031.
[Crossref] [Google Scholar] [Pubmed]
Citation: Li J, TuErdi N, Liu K, Bai J (2023) Histopathological Characteristics of Different Parts of Surgical Specimens of Ureteropelvic Junction Stenosis. Diagnos Pathol Open 8:213. DOI: 10.4172/ 2476-2024.8.1.213
Copyright: © 2023 Li J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3176
- [From(publication date): 0-2023 - Nov 26, 2025]
- Breakdown by view type
- HTML page views: 2722
- PDF downloads: 454