Research Article Open Access
Histopathologic Changes in Dental Follicles of Bone-impacted vs. Partially Bone-impacted 3rd Molars
Esshagh Lassemi1, Mohammad Hosein Kalantar Motamedi2*, Aghdas Frouzandeh3, Farzin Sarkarat4, Mohadese Ghasemi5 and Reza Lasemi6
1 Department of Oral and maxillofacial surgery, College of Dentistry, Azad University of Medical Sciences Tehran, Tehran, Iran
2 Department of Oral and Maxillofacial Surgery, Trauma Research Center, Baqiyatallah University of Medical Sciences and Azad University of Medical Sciences, Tehran, Iran
3 Department of Pathology, college of dentistry, Azad University of Medical Sciences Tehran, Tehran, Iran
4 Department of Oral and Maxillofacial Surgery, College of Dentistry, Azad University of Medical Sciences Tehran, Tehran, Iran
5 Private Practice Dentistry, Tehran, Iran
6 Private Practice Medicine, Tehran, Iran
- *Corresponding Author:
- Mohammad Hosein Kalantar Motamedi
Department of Oral and Maxillofacial Surgery
Trauma Research Center
Baqiyatallah University of Medical Sciences and
Azad University of Medical Sciences, Tehran, Iran
Tel: 982122616946
E-mail: motamedical@yahoo.com
Received Date: December 17, 2013; Accepted Date: January 28, 2014; Published Date: February 02, 2014
Citation: Lassemi E, Motamedi MHK, Frouzandeh A, Sarkarat F, Ghasemi M, et al. (2014) Histopathologic Changes in Dental Follicles of Bone-impacted vs. Partially Bone-impacted 3rd Molars. J Oral Hyg Health 2:120. doi:10.4172/2332-0702.1000120
Copyright: © 2014 Lassemi E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
Aim: Pathologic changes within pericoronal tissues of impacted third molars have been reported. Retained impacted teeth within the bone may lead to pathologic changes in pericoronal tissues. This may endanger the patient’s health; fortunately, this is rare and most of these pathologic changes are benign. However, as these changes are asymptomatic in nature and differentiation between a normal and an abnormal follicle is clinically difficult if not impossible, microscopic evaluation of histopathology changes of impacted third molar follicles was undertaken.
Materials and Method: Follicles of 100 asymptomatic impacted third molars removed from patients in a private dental clinic were submitted for histopathology examination. Patients with systemic diseases and those with distinct pathologic lesions as well as those with pericoronal infections were excluded. Follicles of both maxillary and mandibular impacted third molars were assessed. The width of pericoronal radiolucencies did not exceed 5 millimeters on periapical radiography. Data including the patients’ age, sex, radiolucency, type of impaction, location and presence of second molar root resorption were recorded. Oral pathologists microscopically evaluated the samples, the prevalence of pathologic changes was determined and the demographic factors were statistically evaluated by the chi square and Fisher Exact tests.
Results: In this study of 100 impacted third molar follicles from 78 patients (49 males and 51 females), 54 samples showed pathologic changes (p<0.3). Third molar follicles of patients younger than 25 years showed 66.7% pathologic changes (p<0.6).
Conclusion: We had a high prevalence of pathologic changes in impacted third molar follicles (more than half); these changes were twice as high in patients younger than 25 years and twice as high in the mandible as the maxilla and almost seven times as high (87.1%) in follicles of partial bony impactions than in fully bone impacted 3rd molars. Although the literature shows these follicular changes rarely transform into serious pathologic entities, however, early diagnosis and removal of impacted third molar follicles in adolescence still appear warranted.
Keywords
Impacted third molar; Pathologic changes; Follicle
Introduction
Pathologic changes within pericoronal tissues of impacted third molars have been reported. Retained impacted teeth within the bone may lead to pathologic changes in pericoronal tissues. When an impacted third molar is removed, its pericoronal tissue must be assessed for pathologic changes microscopically [1-4]. Although most of these pathologic changes are benign, however, as these changes are asymptomatic in nature differential diagnosis of a normal follicle from an abnormal one both radiographically and microscopically is important. Because this is clinically difficult if not impossible. Pericoronal tissues of impacted teeth may show pathologic changes such as cyst or neoplasm [5,6]. The origin of several cysts and tumors particularly dentigerous cyst and ameloblastoma can arise from the dental follicle and its ectodermal layer [1-4]. Rakprastikul in a study (2001) reported that 65.58% of 104 samples from the dental follicle showed histopathologic changes [4]. Dachi and Howell l in an x-ray study reported that 10% of 3874 samples from the dental follicle were dentigerous cysts. Thus, differential diagnosis of a normal follicle from abnormal one is of concern [5]. We assessed the prevalence and type of pathologic changes of impacted third molar follicles [6-9].
Patients and Methods
Seventy-eight patients who had referred for removal of their impacted third molar were studied. Patients with systemic diseases, those with specific pathologic lesions in the area and those with dental infection were excluded. All patients had a pericoronal radiolucency width of less than 5 mm on standardized periapical x-rays. The follicle obtained following impacted teeth removal was submitted in 10% formalin to the maxillofacial pathology department. After processing and staining with Hematoxilin and Eosin, the samples were microscopically evaluated via light microscopy and 400 (40×10) magnification. Neoplasm and cystic change in the follicular lumen was assessed. The prevalence of pathologic changes in the samples was determined. The data was evaluated by Chi-Square and Exact Fisher tests.
Results
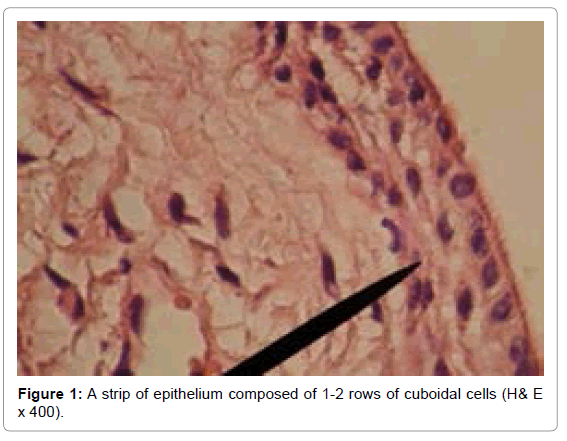
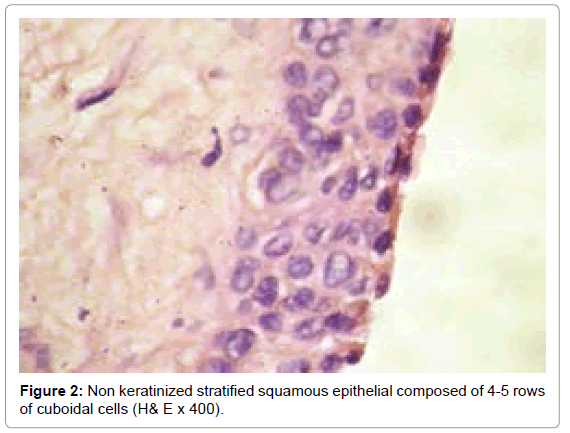
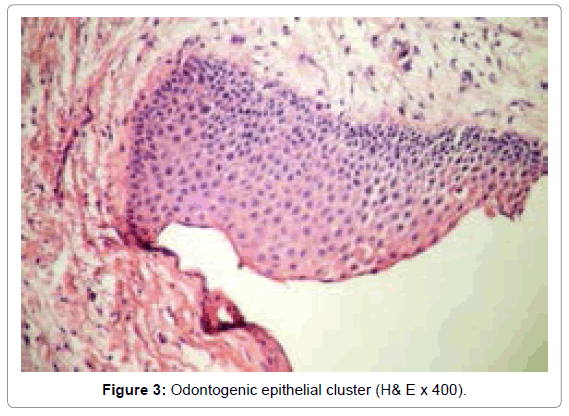
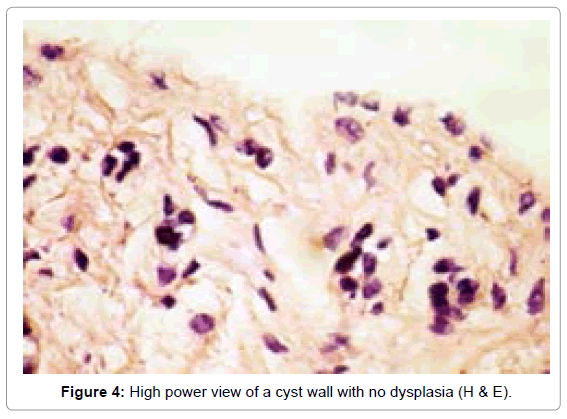
The age of the patients was between 14-40 years and the mean of age was 27. The cause for removal of impacted third molar was prevention of occurrence of pathologic lesions and caries and orthodontic purposes; 100 samples (49 in males and 51 in females) from impacted third molar follicles taken from 78 patients were evaluated; 54 samples (15 in upper jaw and 39 in lower jaw) showed abnormal follicles (p<0.3), (Figure 1). These abnormalities had squamous metaplasia similar to dentigerous cysts or proliferation and nests of odontogenic epithelial remnants (Figures 2 and 3). This form of epithelial change left untreated may transform to mural ameloblastoma; in some samples, the epithelial lining of a cyst wall was discernable but there was no dysplasia (Figure 4).
In 54 samples (27 in males and 37 in females) aged below 25 years 36/54 samples (66.7%) showed pathologic changes (p<0.6); 39/54 samples (72.2%) were in the mandible.
In 54 samples 47/54 samples (87.1%) were from semi-impacted teeth; 80/100 follicles were from semi-impacted teeth 20/100 were from fully bone impactions (Table 1).
| Number | P value | Odds ratio | |
|---|---|---|---|
| Patient Age <25 | 36 (66.7%) | <0.7 | |
| Patient Age >25 | 18 (33.3%) | ||
| Maxilla | 15 (27.7%) | ||
| Mandible | 39 (72.2%) | <0.3 | |
| Bone Impacted | 7 (12.9%) | ||
| Semi-Bone Impacted | 47 (87.1%) | <0.06 | 2.6 |
Table 1: Distribution of 54 samples of follicles with pathologic changes in impacted third molars.
Discussion
Baykul in a study on 94 patients (30 males and 64 females ) despite width of follicular space less than 2.5 mm in impacted wisdom teeth surgery reported 50% pathologic change that represented dentigerous cyst similar to our study [8]. Al-Khateeb and Bataineh at the University of Jordan in a study on 2432 impacted lower third molar reported 46.4% pathologic change [9]. Rakprastikul in a study on 92 patients (mean age 26 years) in 104 impacted third molar reported 58.65% pathologic change with 50.94% representing dentigerous cysts. In our study besides the squamous metaplasia in the follicular lumen, the existence of more than two row of cell layer was reported as a first cystic change [4]. In Adelsperger’s study 13 samples of 18 patients over 21 years showed pathologic changes [10]. In our study 18 samples of 36 patients over 25 years old showed pathologic change. At present the existence of more than two layers of epithelial cells are considered pathologic [11]. In our study, there were a large number of odontogenic epithelial remnants that have potential to become mural ameloblastomas.
Conclusion
We had a high prevalence of pathologic changes in impacted third molar follicles (more than half); these changes were twice as high in patients younger than 25 years and twice as high in the mandible as the maxilla; and almost twice as high in follicles (58.7%) of partial bony impactions than in fully bone impacted 3rd molars. Although the literature shows these follicular changes rarely transform into serious pathologic entities, however, early diagnosis and removal of impacted third molar follicles appear warranted.
References
- Akadiri OA, Okoje VN, Fasola AO, Olusanya AA, Aladelusi TO (2007) Indications for the removal of impacted mandible third molars at Ibadan--any compliance with established guidelines? Afr J Med Med Sci 36: 359-363.
- Stathopoulos P, Mezitis M, Kappatos C, Titsinides S, Stylogianni E (2011) Cysts and tumors associated with impacted third molars: is prophylactic removal justified? J Oral Maxillofac Surg 69: 405-408.
- Stephens RG, Kogon SL, Reid JA (1989) The unerupted or impacted third molar--a critical appraisal of its pathologic potential. J Can Dent Assoc 55: 201-207.
- Rakprasitkul S (2001) Pathologic changes in the pericoronal tissues of unerupted third molars. Quintessence Int 32: 633-638.
- Dachi SF, Howell FV (1961) A survey of 3,874 routine full-mouth radiographs. I. A study of retained roots and teeth. Oral Surg Oral Med Oral Pathol 14: 916-924.
- Glosser JW, Campbell JH (1999) Pathologic change in soft tissues associated with radiographically 'normal' third molar impactions. Br J Oral Maxillofac Surg 37: 259-260.
- Saravana GH, Subhashraj K (2008) Cystic changes in dental follicle associated with radiographically normal impacted mandibular third molar. Br J Oral Maxillofac Surg 46: 552-553.
- Baykul T, Saglam AA, Aydin U, BaÅŸak K (2005) Incidence of cystic changes in radiographically normal impacted lower third molar follicles. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99: 542-545.
- Al-Khateeb TH, Bataineh AB (2006) Pathology associated with impacted mandibular third molars in a group of Jordanians. J Oral Maxillofac Surg 64: 1598-1602.
- Adelsperger J, Campbell JH, Coates DB, Summerlin DJ, Tomich CE (2000) Early soft tissue pathosis associated with impacted third molars without pericoronal radiolucency. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 89: 402-406.
- Kotrashetti VS, Kale AD, Bhalaerao SS, Hallikeremath SR (2010) Histopathologic changes in soft tissue associated with radiographically normal impacted third molars. Indian J Dent Res 21: 385-390.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 15201
- [From(publication date):
March-2014 - Apr 19, 2025] - Breakdown by view type
- HTML page views : 10511
- PDF downloads : 4690