High-Grade Non-Invasive Transitional Cell Carcinoma with Osseous Metaplasia of the 3-Year-Old Boy Urinary Bladder
Received: 20-May-2015 / Accepted Date: 07-Jul-2015 / Published Date: 09-Jul-2015 DOI: 10.4172/2161-0681.1000236
Abstract
Transitional cell carcinomas of the urinary bladder are very rare in paediatrics. In children clearly outweights low grade transitional cell carcinomas, however individual cases of high grade tumors were also described.
Introduction
Transitional cell carcinomas of the urinary bladder are very rare in paediatrics. In children clearly outweights low grade transitional cell carcinomas, however individual cases of high grade tumors were also described.
Case report
We present the case of a 3-year-old boy who was referred to paediatric urology with attack of macroscopic hematuria with subsequent recurrent microscopic hematuria, without dysuria. Ultrasound (US) examination of kidneys showed no pathology (right kidney length 72 mm, width 9 mm, left kidney length 75 mm, width 11 mm, parenchyma with reasonable echogenity). US of the bladder revealed a 13 × 6 mm hyperechogenic, slightly irregular, oval mass on the dorsal bladder wall with apparent vascularization in color flow mode (CFM).
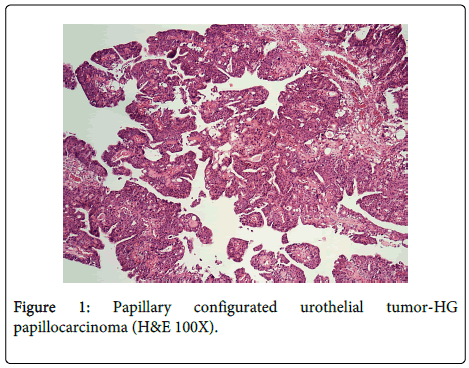
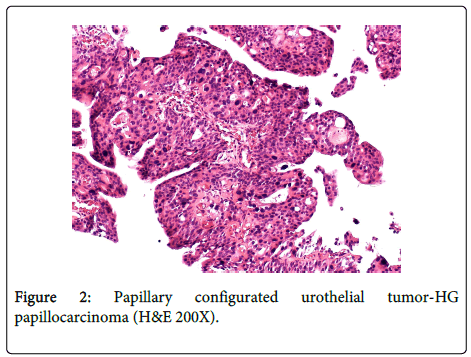
During cystoscopy a polypous tumor with thin stalk on the posterior bladder wall was identified and resected. Basis of the tumor was resected separately and wound bed was treated by laser and coagulation. We reviewed the pathologic specimen and the sample was then sent to the consultation examination for a second reading to an affiliated medical center. Histologically were encountered fragments of papillary configurated urothelial tumor (Figures 1 and 2).
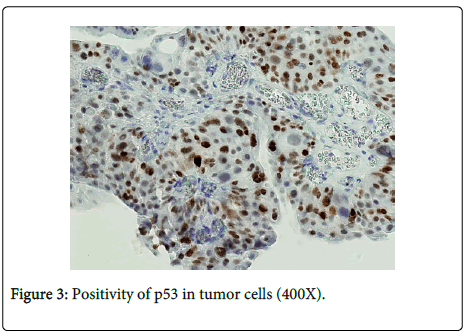
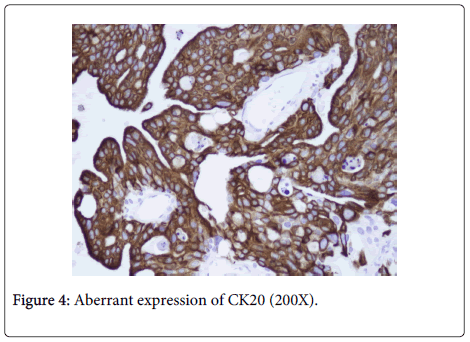
The papillae are covered by urothel of various widths with architectonics disorder and greater focal nuclear atypia. Mitotic activity is evident, also in higher layers of urothelium. Glandular and squamous cell metaplasia is present. Positivity of p53 and aberrant expression of CK20 were evident in tumor cells in immunohistochemical examination (Figures 3 and 4).
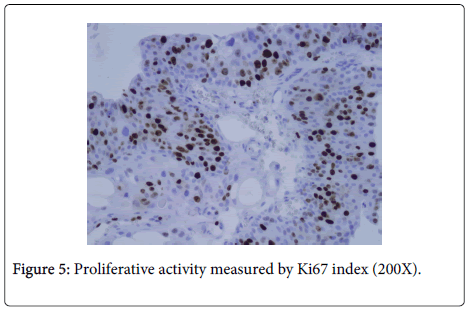
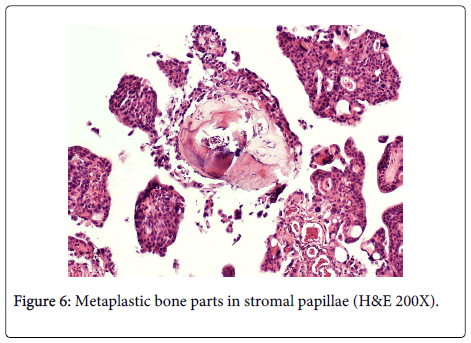
Proliferative activity measured by Ki67 index is up to 20% (Figure 5). Metaplastic bone parts of benign appearance are focally present in stromal papillae (Figure 6) The consensus diagnosis was high-grade transitional cell carcinoma (HG TCC) based on the 2004 WHO classification of bladder tumors. Three months from diagnosis there was no evidence of tumor recurrence on ultrasound and urine cytology had remained negative.
Discussion
Bladder tumors, and in particular bladder transitional cell carcinomas, are rare in children. Nearly all reported tumors in paediatric patients are low grade and invasive disease is present in only 3% of cases [1]. Fewer than 30 cases of transitional cell carcinoma (TCC) have been reported in children less than 10 years of age [2-4]. The male-to-female ratio is 3:1. There is also an ethnic difference: white patients are 39 times more common than black patients [5]. The onset symptom is usually macroscopic haematuria, isolated or recurrent, usually with no associated dysuria. Diagnosis is occasionally delayed in paediatric patients because there is a tendency to underestimate haematuria in children [1]. Definitive diagnosis is performed by cystoscopy, which also allows evaluation of tumor extension, excision or biopsy for pathological study [6]. The histological pattern can be papillary, solid or mixed. The lesion is often seen as a thickening of the epithelium with an increased number of cell layers evenly distributed but densely packed.
The nuclei often retain a semblance of normal orientation but are rounded and pleomorphic. Mitosis may be numerous. TCC is non-invasive or minimally invasive at diagnosis in 75% of cases. There is a 50-60% recurrence rate after initial excision with 10-15% of progression to muscular involvement [7-8]. Transitional cell carcinoma with osseous metaplasia of the stroma is a rare variant of urothelial carcinoma. There are only a few case reports describing this condition, which must be distinguished especially from sarcomatoid carcinoma. There is no evidence for a sarcomatous component (absence of mesenchymal cell proliferation, absence of mitosis in stromal cells) in TCC with osseous metaplasia [9].
The differential diagnosis of bladder tumors, in children include especially 2 conditions: nephrogenic adenoma and hamartoma.
Nephrogenic adenoma is a benign proliferation of glands of the urinary tract which is almost exclusively seen in urinary bladder in children and can mimic a malignant tumor. Due to the papillary appearance seen on cystoscopy and predominant papillae on microscopy, it may be mistaken for TCC. Other histological differences include absence of mitosis, necrosis and significant cytological atypia, varied histological patterns, edematous lamina propria and the presence of inflammation. Immunohistochemical profile of nephrogenic adenoma includes positive staining with CK7, AMACR, PAX2 and PAX8 (TCC is negative for both AMACR and PAX8) [10].
Hamartomas of the urinary bladder are extremely rare (to date only 10 cases, 5 of them in children under 20 years old). On microscopic examination the tumor is composed of tubuloglandular, nested epithelial and fibromyxoid mesenchymal tissues. Glands can be cystically distended and are lined by a single to a few layers of flattened urothelium. These cystic dilated glands occasionally contain amorphous eosinophilic secretory concretion or granular proteinaceous material. A part of the mesenchymal tissue can show osteoid-like metaplasia and intestinal metaplasia with goblet cells can be observed in the cystic glands. Hypervascularity, consisting of engorged thin-walled cavernous vascular tissues can also be a distinctive finding of the tumor. There are neither cellular atypia nor mitotic activity of the epithelial or mesenchymal component of the tumor suggestive of true neoplastic growth. Hematopyuria associated with infection or inflammatory reaction in the bladder is a characteristic clinical sign in most reported cases [11].
Basic differences between papilloma, low grade (LG) and high grade (HG) papillocarcinoma and nephrogenic adenoma are listed in Table 1.
| Papilloma | Low grade papillocarcinoma | High grade papillocarcinoma | Nephrogenic adenoma | |
|---|---|---|---|---|
| Age | Mean age:46 years; range 22-89 years, may occur in children |
Mean age:70 years; rare in children |
Usually ages 50+; extremely rare in children |
Almost exclusively in children |
| Gross description | Soft, pink, small isolated growth with delicate papillary structures, usually pedunculated, mean 3 mm. | More solid cores with firmer consistency than papillomas, usually solitary. Wide variation in size. |
Sessile or cauliflower-like with necrosis and ulceration. Exophytic papillary growth. |
Polypoid, sessile or papillary, 20% are multiple. |
| Histology | Discrete papillary growth with a central fibrovascular core lined by urothelium of normal thickness and cytology. | Papillary urothelial neoplasm with some degree of cytoarchitectural disorder and distinct but low grade cytologic abnormality. No high-grade cytologicfeatures (no pleomorphism, no mitoses toward surface, no nucleoli throughout). |
A neoplasm with urothelium lining papillary fronds, a predominant disorderly pattern and moderate to marked architectural and cytologicatypia. | Metaplastic change with papillary or cystic structures composed of small hollow tubules similar to mesonephric tubules, usually lined by a single layer of bland cuboidal or hobnail cells, surrounding eosinophilic or basophilic secretions. Absence of mitosis, necrosis and significant cytological atypia. |
| Positive stains | CK20 limited to superficial/umbrella cells as in normal urothelium CK7 |
CK20 is stronger and diffusely extending into the deep layers Ki67 mostly about 20% p53 index mostly less than 5% CK7 Blood group antigens |
CK20 is stronger and diffusely extending into the deep layers Ki67 higher (mostly more than 40%) p53 index mostly more than 10% CK7 Survivin Overexpression of p16 Beta hCG in 1/3 ER in 14% |
CK7 AMACR PAX2 PAX8 EMA |
| Negative stains | p53 low Ki67 |
Usually survivin AMACR PAX8 |
Blood group antigens No/weak expression of E-cadherin |
CK20 CK903 p63 CD10 (may be positive) |
Table 1: Differences between papilloma, LG and HG papillocarcinoma and nephrogenic adenoma [10,12,17].
Conclusion
In paediatric cases of haematuria, transitional cell carcinoma must be ruled out. Among carcinomas of the bladder in children, the most common is a low grade TCC, which must be distinguished especially from nephrogenic adenoma and hamartoma, in cases with osseous metaplasia also from sarcomatoid carcinoma. In the setting of HG disease, resection and adjuvant therapies should be pursued in the attempt to limit recurrences and disease progression.
References
- Hoenig DM, McRae S, Chen SC, Diamond DA, Rabinowitz R, et al. (1996) Transitional cell carcinoma of the bladder in the pediatric patient. J Urol 156: 203-205.
- Lerena J, Krauel L, GarcÃa-Aparicio L, Vallasciani S, Suñol M, et al. (2010) Transitional cell carcinoma of the bladder in children and adolescents: six-case series and review of the literature. J PediatrUrol 6: 481-485.
- Gülpinar O, Soygür T, Baltaci S, Akand M, Kankaya D (2006) Transitional cell carcinoma of bladder with lamina propria invasion in a 10-year-old boy. Urology 68: 204.
- Patel R, Tery T, Ninan GK (2008) Transitional cell carcinoma of the bladder in first decade of life. PediatrSurgInt 24: 1265-1268.
- Madgar I, Goldwasser B, Nativ O, Hanani Y, Jonas P (1988) Long-term followup of patients less than 30 years old with transitional cell carcinoma of bladder. J Urol 139: 933-934.
- Wilson-Storey D, Allen AE, Variend S (1992) Transitional cell papillary bladder neoplasm in a girl: an unusual presentation. J PediatrSurg 27: 113-114.
- Khasidy LR, Khashu B, Mallett EC, Kaplan GW, Brock WA (1990) Transitional cell carcinoma of bladder in children. Urology 35: 142-144.
- Rodriguez A, Burday D, Sexton W, Ahmad N, Pow-Sang JM (2005) Urothelial carcinoma in a child. Arch EspUrol 58: 473-475.
- Mege-Lechevallier F, Cherasse A, Ronze S, Colombel M, Scoazec JY (2007) [Transitional carcinoma of the ureter with osseous metaplasia of the stroma: a case report]. Ann Pathol 27: 43-46.
- Sathe PA, Ghodke RK, Kandalkar BM (2012) Multifocal nephrogenicadenoma - a mimicker of malignancy. Indian J Pediatr 79: 1661-1663.
- Ota T, Kawai K, Hattori K, Uchida K, Akaza H, et al. (1996)Â Hamartoma of the urinary bladder. Int J Urology 6:211-214.
- Safaei A, Farzaneh MR, Amin Sharifi AR (2012) Immunohistochemistery Study in a Case of Nephrogenic Adenoma of Bladder. Iran J Med Sci 37: 137-140.
- Paner GP, Zehnder P, Amin AM, Husain AN, Desai MM (2011) Urothelial neoplasms of the urinary bladder occurring in young adult and pediatric patients: a comprehensive review of literature with implications for patient management. AdvAnatPathol 18: 79-89.
- Fine SW, Humphrey PA, Dehner LP, Amin MB, Epstein JI (2005) Urothelial neoplasms in patients 20 years or younger: a clinicopathological analysis using the world health organization 2004 bladder consensus classification. J Urol 174: 1976-1980.
- Berrettini A, Castagnetti M, Salerno A, Nappo SG, Manzoni G, et al. (2015) Bladder urothelial neoplasms in pediatric age: experience at three tertiary centers. J PediatrUrol 11: 26.
- Telli O, Sarici H, Ozgur BC, Doluoglu OG, Sunay MM, et al. (2014) Urothelial cancer of bladder in young versus older adults: clinical and pathological characteristics and outcomes. Kaohsiung J Med Sci 30: 466-470.
Citation: Skarda J, Michalek J, Tichy T, Smakal O, Kral M et al. (2015) High-Grade Non-Invasive Transitional Cell Carcinoma with Osseous Metaplasia of the 3-Year-Old Boy Urinary Bladder. J Clin Exp Pathol 5:236. DOI: 10.4172/2161-0681.1000236
Copyright: © 2015 Skarda J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 15791
- [From(publication date): 8-2015 - Jul 05, 2025]
- Breakdown by view type
- HTML page views: 11153
- PDF downloads: 4638