Heterogeneity in the Prevalence of Health Risk Factors among Justice- Involved Adolescents: The Intersectionality of Gender and Race/Ethnicity
Received: 26-Jul-2018 / Accepted Date: 09-Oct-2018 / Published Date: 11-Oct-2018 DOI: 10.4172/2161-0711.1000629
Keywords: Gender; Race; Ethnicity; Intersectionality; Health risk; STD; Marijuana use; Juvenile delinquents; Arrested youth
Introduction
Research on health risk behaviors among justice-involved youth of different gender and race/ethnicity groups has increased in recent years. Studies of subgroups of these youth have focused on offense severity, mental health, substance abuse, sexual risk, or Sexually Transmitted Disease (STD) status, and often combinations of these problems. A major focus has been on youth placed on detention [1-3] or in residential programs [4,5]. However, studies involving youth in juvenile court [6], probation [7-9], or centralized intake facilities [10,11] have increased. This research continues to confirm that justiceinvolved youth have higher prevalence rates of these problems, than adolescent in the general community [12-14], and that the prevalence rates for mental health problems [1,2,15], substance use [16], sexual risk behavior, and STD status [3] differ among gender and race/ethnic subgroups [11].
At the same time, as Wells et al. [17] noted, these etiological studies have, with few exceptions, not provided information on the intersectionality of gender and race/ethnicity and the prevalence of health risk factors across these diverse subgroups within the same study. Most often, studies are completed on male and female youth from specific race or ethnicity groups, or involve same-gender youth from different race/ethnicity groups. Often, we generalize from results in different studies, focusing on specific, but different psychosocial problems among various subgroups of youth.
These generalizations assume the predictors, and sometimes causes, of these problems are similar across these youth subgroups in different locations. This is an important issue, as prevention and intervention approaches that are sensitive to gender and race/ethnic group health risk variations are more likely to be successful because they are informed by an understanding of the intersectionality of gender and culture [17]. As the National Institute on Drug Abuse (NIDA) [18] has indicated, “Tailoring services to fit the needs of the individual is an important part of effective drug abuse treatment for criminal justice populations”.
There is a need for more research to determine if offense severity, mental health, substance abuse, sexual risk issues, and STD status are similar or different across multiple gender and race/ethnicity subgroups entering the juvenile justice system, when examined simultaneously. Such studies can provide a more nuanced understanding of the factors and processes involved in the etiology of these serious public health problems.
Health risk problem areas that are gender and race/ethnic specific may require targeted prevention and intervention strategies, whereas health risk factors which are similarly reflected across different gender and race/ethnic subgroups of youth could lead to the development of more generic intervention programs. Yet, surprisingly, research is lacking on intersectional studies that examine the prevalence of a broad range of risk factors among justice-involve youth.
More research is needed on youth entering intake facilities following arrest. Since research has indicated that 80% of arrested youth are returned to the community following arrest [19], centralized intake facilities present an excellent opportunity to identify diverse at-risk youth health risks and link them with community-based services [20].
Focus of this study
The present study sought to address the above identified gaps in the research literature by examining simultaneously offense severity and the health risk factors noted above, in a sample of newly arrested male and female youth from diverse race/ethnicity backgrounds entering a centralized intake facility in a southeastern U.S. city. As described in more detail in the strategy of analyses section, we conducted a multigroup, latent class analysis involving post-intake arrest release status (a proxy for charge level), mental health, drug use, and sexual risk factors, including STD test results. The study is unusual in that biological data on both drug use and STDs were collected. The data provided a unique opportunity to assess the relative influence of these factors on a diverse group of youths, many of whom were released back to the community following arrest. Specifically, the present study addressed three research questions:
• Based on latent class analysis, are there subgroups reflecting different combinations of arrestee’s post-intake release, mental health, drug use, and sexual risk factors, including STD test results, across gender and race/ethnicity groups?
• If so, what proportion of youths in these subgroups comprise the various categories for post-intake release, mental health, drug use, sexual risk, and STD infection across gender-race/ethnicity groups?
• How does age relate to the latent class analysis findings?
Method
Data and procedures
The data were collected from a Health Coach Service for youth entering a Juvenile Assessment Center (JAC), a centralized intake facility, in a southeastern U.S. city. Every juvenile arrested or charged in the county is taken to the JAC for intake processing. During intake, youths were informed of the Health Coach Service and solicited for participation. The Health Coach Service involves collaboration with the Department of Health (DOH) to gather data from the youths and link them to appropriate services. Specifically, the Health Coach service has four major goals [21]: (1) offer HIV evidence-based risk reduction information and education to youth using a gender and developmentally appropriate online curriculum; (2) perform urinalysis (via the EMIT procedure) for recent drug use, rapid initial testing for HIV (swab test), and testing for other STDs (chlamydia and gonorrhea); (3) provide follow-up with youth and link youths who are drug-involved, test positive for HIV or other STDs, or screen high on a depression inventory with appropriate treatment; and (4) refer youth who report they do not have a “medical home” to a collaborating family health center, and monitor and track adolescents’ engagement and retention in care.
Participation in the service is voluntary, and the Health Coaches obtain informed consent from participants. State law does not require youth 12 years and over to obtain parental consent for STD or HIV testing or treatment. Due to the sensitive nature of the health data, DOH and the Health Coach Service collect the data and de-identify the data prior to providing it to the researchers for analysis. Thus, the data used in this study were deemed exempt by the Institutional Review Board (IRB). The present study examines data collected from n=1,620 youths with first or initial JAC entry who received Health Coach services (October 19, 2015 [project implementation date] through December 31, 2016 for females, and February 4, 2016 through December 31, 2016 for males). High male (82%) and female (85%) youth participation rates in the Health Coach Service were obtained during the period covered by this study.
Sociodemographic information (gender, age, race/ethnicity) and post-JAC placement were available for all youth declining the Health Coach Service. Comparisons of youth agreeing or declining to participate in the Health Coach Service indicated only one significant difference between the two groups: participating youth were slightly older (15.8 vs. 15.6 years old, respectively, p<0.05). (Due to space concerns, detailed results are not presented. A copy of the results can be obtained from the senior author upon request.)
Measures and group membership
Socio-demographic information was collected on the youths’ selfreported gender (refers to biological sex rather than gender identity), race/ethnicity, and age. Age was measured in number of years at time of JAC entry and was a covariate in subsequent analyses. Self-reported gender (male vs. female) and race/ethnicity (African American or Black, Hispanic, and white) were used to categorize youth into subgroups for the latent class analyses.
In accordance with State law, JAC personnel must complete a Detention Risk Assessment Instrument (DRAI) for each youth processed at the JAC [22]. The DRAI takes into consideration the youth’s most serious current offense, other current offenses and pending charges, prior offense history, current legal status, and aggravating or mitigating circumstances. Based on this information, each youth is assigned a risk score. Youths assigned 0-6 points are released to the community without supervision, awaiting placement in a diversion program. Youths assigned 7-11 points are placed on nonsecure home detention (i.e., home arrest). Youths assigned 12 or more points are placed in secure detention. The categorical post-JAC release variable used in subsequent analyses reflects the seriousness of offense categories: 1=outright release, 2=home detention and 3=secure detention.
Participating youths provided urine samples. At the DOH testing lab, the urine samples were split, with half of the specimen tested for drugs and the other half tested for STD infection. For drug use, the Urinalysis (UA) tested for the following using the EMIT procedure: (1) methamphetamines, (2) cocaine, (3) opiates, (4) marijuana, (5) spice (UR144 metabolite), (6) alcohol, and (7) benzodiazepines. Two compounds were used to test for the presence of alcohol in the urine specimens: (1) Ethanol (ETOH), 8 to 12 h use and (2) ethyl glucuronide (EtG), 4 to 5 days of use. The cut off levels are 20 ng/mL of urine and 500 ng/mL of urine, respectively. The cutoff level for a positive for marijuana test is 50 ng/mL of urine. Few youths tested positive for any drug other than marijuana (range 0% to below 5% for each drug category excluding marijuana); hence, these drugs were excluded from further analysis. The UA results for marijuana were dichotomized (0=negative, 1=positive) for subsequent analysis.
The other half of the urine specimens were tested for STD infection. A non-invasive, U.S. Food and Drug Administration (FDA)-approved, urine-based nucleic acid test, GenProbe Aptima® Combo 2 Assay, was used to test for chlamydia and gonorrhea. The sensitivity of GenProbe's test has been shown to be superior to culture and direct specimen tests. For chlamydia, the sensitivity and specificity of the GenProbe urinebased test are 95.9% and 98.2%, respectively, and for gonorrhea, they are 97.8% and 98.9%, respectively [23]. For analyses purposes, each youth's STD results were recoded into a dichotomous variable representing positive (coded as 1) for any STD (i.e., chlamydia, gonorrhea, or both) or negative (coded as 0) for all STD tests.
In addition to STD infection, an indicator of sexual risk behavior was included in the present study. Research has consistently used the number of sexual partners as an indicator of sexual risk behavior [24]. Participants were asked to self-report their lifetime number of sexual partners using a question taken from the high school version of the Centers for Disease Control’s Youth Risk Behavior Survey [25]. The question asked: “During your life, with how many people have you had sexual intercourse?” Response choices were “I have never had sexual intercourse,” “1 person,” “2 people,” “3 people,” “4 people,” “5 people,” and “6 or more people.” The lifetime number of sexual partners variable was coded as 0 for “never had sexual intercourse” to 6 for “6 or more people.”
Finally, a measure of elevated depressive symptoms was included in the study. Depression was measured using the 8-item version of the Center for Epidemiological Studies Depression Scale (CES-D) [26]. The eight depressive symptom items are: “I felt I could not shake off the blues even with the help from my family and friends,” “I felt sad,” “I felt depressed,” “I thought my life had been a failure,” “I felt fearful,” “My sleep was restless,” “I felt lonely,” and “I had crying spells.” Youths were asked to report how many days in the past week they felt this way, with responses scored as 0=less than one day, 1=1-2 days, 2=3-4 days, or 3=5-7 days. An additive index was used to measure the level of depression. A previous study of the Health Coach Service data confirmed the 8-item depression measure demonstrated a good fit of the data to Confirmatory Factor Analysis (CFA) results among African American/Black and white youth [27]. An additional CFA of the 8 depression items also yielded a one factor, invariant model which fit the data for Hispanic males and females (χ2=26.70, df=20, p=0.14; Comparative Fit Index [CFI]=0.999, Tucker-Lewis coefficient [TLI]=0.999; Root Mean Square Error of Approximation [RMSEA]=0.04). Previous research has found that a depression measure score of 7 or higher is a threshold score indicative of potentially needing clinical intervention [28,29]. Therefore, a dichotomous measure of elevated depression was created for subsequent analyses with total depression scale scores of 0-6 coded as 0 and scores of 7 or higher coded as 1.
Analysis strategy
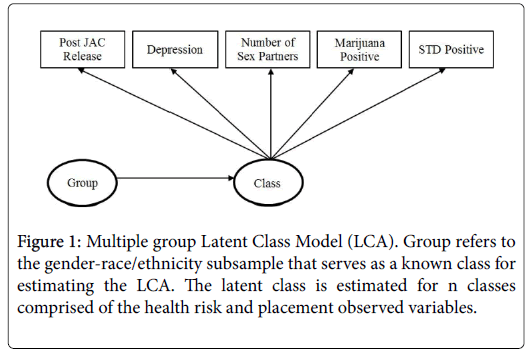
The analyses proceeded in several stages. First, descriptive comparisons were made among the six gender-race/ethnicity comparison groups on the variables analyzed in this study. Second, a Latent Class Analysis (LCA) was completed on the following health risk variables: post-JAC release status (a measure of offense severity), UA marijuana test results, STD status, number of lifetime sexual partners, and elevated depression. The LCAs were performed using Mplus Version 8.0 [30]. LCA seeks to identify an underlying classification of entities (e.g., individuals) which are related to manifest indicators in probabilistic terms [31]. In particular, the LCA model is useful when studying a heterogeneous population. Latent class analysis assumes heterogeneity exists within a population and that two or more latent variables (i.e., classes) can cluster the population into more homogenous subtypes based on distribution of the characteristics of the observed variables (e.g., offense severity, UA test results, STD status, number of sexual partners, and depression) [31]. The resulting classes are latent variables reflecting the underlying phenomenon under study but are not directly observable. The observed variables are considered indicators of these latent variables. The use of LCA in this study was exploratory in nature, i.e., without specification of hypotheses relating to the values of the conditional or latent class probabilities. The objective of the LCA analyses was to examine the heterogeneity, or variation, in numbers of health risk behaviors and their magnitude, and identify health risk behavior among subgroups of youths across gender and race/ethnicity groups, assuming heterogeneity exists. Multi-group LCA (using the known class function in Mplus) was employed for this purpose. LCAs were performed across the six gender-race/ethnicity groups (described below) on the health risk behavior measures. MLR (Maximum Likelihood Parameter estimates with standard errors and a chi-square statistic that are robust to non-normality and non-independence of observations) was used as an estimator [30]. The Mplus feature for ML estimation of missing values was used to treat any missing data [30]. Figure 1 illustrates the model that was estimated. Finally, following the LCA estimations, an additional analysis was performed. For each gender-race/ethnicity group, the relationship between youth age and the variables in the latent class model were studied.
Regarding missing data, other than the UA marijuana test results and STD test results (n=244 and n=329 cases, respectively), no cases were missing information on the variables included in the analyses. Analyses were conducted to examine whether cases with valid or missing data on UA marijuana test results or STD test results differed regarding the other measures [32]. Near zero relationships were found, suggesting the cases with missing data on these two variables did not introduce systematic bias. There was a significant correlation between valid and missing data relating to the marijuana test results and STD test results (r=0.474, p<001). However, since the youths’ urine specimens were split for drug and STD testing, this relationship was an artifact of the testing procedure, not a reflection of systematic bias. Hence, the Mplus data imputation procedure [33] was used, in which each missing value was replaced by a set of plausible values drawn from their predictive distribution [34] to estimate the values of the missing data.
Assessing LCA model fit
Several indictors were used to assess LCA model fit: (1) the classification table, with high diagonal values and low off-diagonal values indicating good classification quality [30]; (2) entropy, with values ranging from 0 to 1, with scores close to 1 indicating clear classifications [30]; (3) Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), and the sample size adjusted BIC (saBIC), with lower AIC, BIC, and saBIC, scores (i.e., closest to zero) indicating a better fit of the model; (4) the fit of the model to the univariate and bivariate frequency tables, with smaller standardized residuals between the observed and estimated (expected) probabilities indicating better model fit. (The mixture model with known classes precluded use of the Lo-Mendell-Rubin likelihood ratio test of model fit [35]; and having more than one categorical latent variable prevented use of a parametric bootstrapped likelihood test of model fit [36,37].) Substantive meaningfulness of the LCA solution was also a criterion in assessing fit. In addition, the LCA analyses reported here utilized sufficient ratios of cases to analysis variables to provide reliable parameter estimates for the models.
Results
In constructing the comparison groups for analysis, the gender and race/ethnicity variables were cross-tabulated. Results indicated the following subsample sizes across the six gender-race/ethnicity groups: African American or Black males (n=621; 38.3%), African American or Black females (n=311; 19.2%), Hispanic males (n=128; 7.9%), Hispanic females (n=108; 6.7%), white males (n=221; 13.6%), and white females (n=175; 10.8%). Ethnicity information was not available for n=56 youth (3.5%); hence, these youths were excluded from subsequent analyses.
Age, health risk factor, and post-jac release comparisons
As can be seen in Table 1, the average age in the six gender-race/ ethnicity groups ranged from 15.47 to 15.99. On average, females were slightly younger than the males in the study. Males in each race/ethnic group had higher marijuana test positive rates, reported more lifetime sexual partners, and had higher rates of placement in secure detention, than females. Most females were released outright from the JAC, without a form of detention. On average, females had higher rates of elevated depression and higher STD positive rates, than males.
| Variables | Black Males | Black Females | Hispanic Males | Hispanic Females | White Males | White Females | Statistical Significance |
|---|---|---|---|---|---|---|---|
| Age, mean (SD) | 15.99 (1.26) | 15.47 (1.46) | 15.99 (1.27) | 15.64 (1.46) | 15.94 (1.23) | 15.64 (1.54) | F(5, 1558) = 8.10*** |
| N | 621 | 311 | 128 | 108 | 221 | 175 | |
| Post JAC release | |||||||
| Outright | 30.90% | 56.30% | 49.20% | 66.70% | 47.50% | 70.30% | χ2(10) = 137.45*** |
| Home detention | 25.40% | 19.60% | 25.00% | 13.90% | 19.00% | 8.60% | |
| Secure detention | 43.60% | 24.10% | 25.80% | 19.40% | 33.50% | 21.10% | |
| N | 621 | 311 | 128 | 108 | 221 | 175 | |
| Marijuana positive | 48.70% | 30.30% | 48.10% | 38.90% | 53.10% | 31.20% | χ2(5) = 42.80*** |
| N | 515 | 261 | 108 | 90 | 192 | 154 | |
| Elevated depression | 6.10% | 21.90% | 10.90% | 26.90% | 13.10% | 31.40% | χ2(5) = 101.07*** |
| N | 621 | 311 | 128 | 108 | 221 | 175 | |
| Sex partners, mean (SD) | 3.46 (2.36) | 1.63 (1.84) | 3.14 (2.36) | 1.88 (1.85) | 2.71 (2.27) | 2.13 (2.13) | F(5, 1558) = 36.11*** |
| N | 621 | 311 | 128 | 108 | 221 | 175 | |
| STD positive | 9.00% | 14.10% | 6.90% | 13.60% | 6.30% | 8.40% | χ2(5) = 10.61*** |
| N | 499 | 241 | 102 | 88 | 174 | 131 | |
| Note. JAC = Juvenile Assessment Center. Two-tailed p-values: *p < 0.05; **p < 0.01; ***p < 0.001 | |||||||
Table 1: Age, post jac release, and health risk factors comparisons across gender by race/ethnicity groups.
Relationships among the variables in the latent class analysis
Polychoric correlations among the categorical variables included in the LCAs found varying degrees of relationships among them in the six gender-race/ethnicity groups. In particular, the number of reported lifetime sexual partners was most consistently and positively related to the other variables in the latent class model.
There was no indication of multicollinearity in any of these relationships. (A table reporting these results has been omitted due to space concerns. A copy of the table is available from the senior author upon request.)
LCA fit statistics
The LCA fit statistics are shown in Table 2. Given the limited number and distribution of cases across the various categorical variables, up to a three class LCA solution could be reliably estimated. A two-class solution seemed to fit the data best: (1) the classification table indicated high diagonal values and few off diagonal values greater than 0.10; (2) a very high entropy value of 0.883 was obtained; (3) the two-class solution had lower AIC, BIC, and saBIC values, than the three-class solution; (4) very few significant univariate and bivariate frequency standardized residuals were found; and (5) the two-class solution provided a more substantively meaningful fit, than the threeclass solution. As a final check on the results, the analyses were re- estimated with double the random starts, to confirm the best log likelihood was obtained and replicated. The findings indicated this was the case.
| Number of Classes | Akaike (AIC) | Bayesian (BIC) | Sample Size Adjusted BIC | Entropy |
|---|---|---|---|---|
| 1 Class | 17554.67 | 17934.88 | 17709.32 | --- |
| 2 Classes | 17475.49 | 18241.26 | 17786.98 | 0.88 |
| 3 Classes | 17517.09 | 18668.42 | 17985.41 | 0.89 |
| 4 Classes | could not be reliably estimated | |||
| Note. AIC = Akaike Information Criterion; BIC = Bayesian Information Criterion. | ||||
Table 2: Latent class analysis fit statistics (n=1564).
Two-class LCA results
The two-class LCA results, in probability scale, are shown in Table 3. Based on the average probability for each category comprising the health factors and release type variables, the two classes can best be described as High Risk, where the probabilities are generally higher for post-JAC secure detention, positive marijuana use, STD positive, higher number of sexual partners, and elevated depression in this class, vs . Low Risk, where the probabilities for these problems are generally lower in this class. While this is a common distinction in each of the six groups, there are a few exceptions to this pattern (e.g., among Hispanic males, the estimated STD positive rate among High Risk youth is 0.04, compared to 0.08 among Low Risk youth).
| Variable | Black Males High Risk (n=380; 24%) |
Black Males Low Risk (n=241; 15%) |
Black Females High Risk (n=102; 6%) |
Black Females Low Risk (n=209; 13%) |
||||
|---|---|---|---|---|---|---|---|---|
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Post JAC release | ||||||||
| Outright | 0.20*** | 0.06 | 0.52** | 0.15 | 0.51*** | 0.06 | 0.60*** | 0.05 |
| Home detention | 0.28*** | 0.03 | 0.21*** | 0.05 | 0.14** | 0.04 | 0.23*** | 0.04 |
| Secure detention | 0.53*** | 0.05 | 0.27* | 0.13 | 0.35*** | 0.06 | 0.17*** | 0.04 |
| Marijuana test | ||||||||
| Negative | 0.45*** | 0.04 | 0.63*** | 0.1 | 0.47*** | 0.07 | 0.83*** | 0.04 |
| Positive | 0.55*** | 0.04 | 0.37*** | 0.1 | 0.53*** | 0.07 | 0.17*** | 0.04 |
| STD test | ||||||||
| Negative | 0.88*** | 0.03 | 0.98*** | 0.04 | 0.62*** | 0.08 | 1 | 0 |
| Positive | 0.13*** | 0.03 | 0.02 | 0.04 | 0.38*** | 0.08 | 0 | 0 |
| Sex partners | ||||||||
| None | 0.07 | 0.09 | 0.37** | 0.11 | 0.06 | 0.04 | 0.56*** | 0.06 |
| 1 | 0.09* | 0.04 | 0.19** | 0.06 | 0.26*** | 0.06 | 0.22*** | 0.04 |
| 2 | 0.04 | 0.04 | 0.18** | 0.06 | 0.20*** | 0.05 | 0.09** | 0.03 |
| 3 | 0.09*** | 0.03 | 0.10* | 0.04 | 0.25*** | 0.06 | 0 | 0 |
| 4 | 0.05 | 0.03 | 0.15* | 0.06 | 0.08* | 0.04 | 0.06* | 0.02 |
| 5 | 0.12* | 0.05 | 0 | 0 | 0.03 | 0.02 | 0.02 | 0.01 |
| 6 or more | 0.54*** | 0.12 | 0.02 | 0.19 | 0.13* | 0.05 | 0.05 | 0.03 |
| Elevated depression | ||||||||
| No | 0.94*** | 0.02 | 0.93*** | 0.03 | 0.68*** | 0.06 | 0.85*** | 0.04 |
| Yes | 0.06*** | 0.02 | 0.07** | 0.03 | 0.32*** | 0.06 | 0.16*** | 0.04 |
| Hispanic Males High Risk (n = 33; 2%) |
Hispanic Males Low Risk (n = 95; 6%) |
Hispanic Females High Risk (n = 73; 5%) |
Hispanic Females Low Risk (n = 35; 2%) |
|||||
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Post JAC release | ||||||||
| Outright | 0.15 | 0.12 | 0.61*** | 0.09 | 0.56*** | 0.06 | 0.88*** | 0.07 |
| Home detention | 0.30* | 0.13 | 0.23*** | 0.05 | 0.17*** | 0.05 | 0.09 | 0.05 |
| Secure detention | 0.54*** | 0.12 | 0.16 | 0.09 | 0.28*** | 0.06 | 0.04 | 0.04 |
| Marijuana test | ||||||||
| Negative | 0.55*** | 0.13 | 0.51*** | 0.07 | 0.54*** | 0.07 | 0.73*** | 0.09 |
| Positive | 0.45** | 0.13 | 0.50*** | 0.07 | 0.46*** | 0.07 | 0.27** | 0.09 |
| STD test: | ||||||||
| Negative | 0.96*** | 0.05 | 0.92*** | 0.04 | 0.81*** | 0.05 | 0.96*** | 0.04 |
| Positive | 0.04 | 0.05 | 0.08* | 0.04 | 0.19*** | 0.05 | 0.04 | 0.04 |
| Sex partners | ||||||||
| None | 0 | 0 | 0.27*** | 0.07 | 0.03 | 0.03 | 0.69*** | 0.13 |
| 1 | 0.19 | 0.1 | 0.14** | 0.04 | 0.36*** | 0.07 | 0.1 | 0.12 |
| 2 | 0.04 | 0.04 | 0.11** | 0.04 | 0.31*** | 0.06 | 0 | 0 |
| 3 | 0 | 0 | 0.13** | 0.04 | 0.06 | 0.04 | 0.19* | 0.08 |
| 4 | 0.20* | 0.09 | 0.05 | 0.04 | 0.04 | 0.03 | 0 | 0 |
| 5 | 0.19 | 0.11 | 0.04 | 0.03 | 0.07* | 0.03 | 0 | 0 |
| 6 or more | 0.37* | 0.18 | 0.27** | 0.09 | 0.13* | 0.05 | 0.02 | 0.07 |
| Elevated depression | ||||||||
| No | 0.59* | 0.25 | 1 | 0 | 0.59*** | 0.07 | 1 | 0 |
| Yes | 0.41 | 0.25 | 0 | 0 | 0.41*** | 0.07 | 0 | 0 |
| White Males: High Risk (n = 59; 4%) |
White Males: Low Risk (n = 162; 10%) |
White Females: High Risk (n = 38; 2%) |
White Females: Low Risk (n = 137; 8%) |
|||||
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Post JAC release | ||||||||
| Outright | 0.33*** | 0.07 | 0.54*** | 0.06 | 0.49*** | 0.13 | 0.77*** | 0.05 |
| Home detention | 0.15 | 0.08 | 0.21*** | 0.04 | 0.15 | 0.08 | 0.07* | 0.03 |
| Secure detention | 0.53*** | 0.09 | 0.26*** | 0.05 | 0.36* | 0.14 | 0.17*** | 0.04 |
| Marijuana test | ||||||||
| Negative | 0.42*** | 0.1 | 0.49*** | 0.05 | 0.34* | 0.14 | 0.79*** | 0.07 |
| Positive | 0.58*** | 0.1 | 0.51*** | 0.05 | 0.66*** | 0.14 | 0.21** | 0.07 |
| STD test | ||||||||
| Negative | 0.79*** | 0.11 | 1 | 0 | 0.65** | 0.25 | 1 | 0 |
| Positive | 0.21 | 0.11 | 0 | 0 | 0.35 | 0.25 | 0 | 0 |
| Sex partners | ||||||||
| None | 0 | 0 | 0.35*** | 0.07 | 0 | 0 | 0.42*** | 0.09 |
| 1 | 0.06 | 0.06 | 0.17*** | 0.04 | 0.08 | 0.07 | 0.22*** | 0.05 |
| 2 | 0.1 | 0.08 | 0.15*** | 0.04 | 0 | 0.23 | 0.16** | 0.06 |
| 3 | 0 | 0 | 0.17*** | 0.04 | 0.06 | 0.07 | 0.09** | 0.03 |
| 4 | 0.20* | 0.1 | 0.04 | 0.05 | 0.21* | 0.1 | 0.04 | 0.04 |
| 5 | 0.18* | 0.09 | 0 | 0 | 0.29* | 0.13 | 0.02 | 0.03 |
| 6 or more | 0.45** | 0.14 | 0.13 | 0.1 | 0.36* | 0.15 | 0.05 | 0.04 |
| Elevated depression | ||||||||
| No | 0.83*** | 0.08 | 0.88*** | 0.03 | 0.58*** | 0.1 | 0.72*** | 0.05 |
| Yes | 0.17* | 0.08 | 0.12*** | 0.03 | 0.42*** | 0.1 | 0.28*** | 0.05 |
| Note. JAC = Juvenile Assessment Center. Mean values across categories for variables may not add up to 1.00 (100%) due to rounding errors. Two-tailed p-values: *p < 0.05; **p < 0.01; ***p < 0.001 | ||||||||
Table 3: Health risk and release characteristics for LCA results by gender-race/ethnicity group (results in probability scale).
The six gender-race/ethnicity groups differ in overall risk levels. High Risk African American males account for nearly a quarter (24%; n=380) of all youth in the study, whereas Low Risk African American males account for 15% (n=241). Six percent (n=102) of the youth were High Risk in the African American female group, while 13% (n=209) were in the Low Risk African American female group. Only 2% (n=33) of youths were in the High Risk Hispanic male group, and three times as many Hispanic males were in the Low Risk group (n=95, 6%). Five percent (n=73) of youths were in the High Risk Hispanic female group and 2% (n=35) were in the Low Risk Hispanic female group. Four percent (n=59) of youths were in the High Risk white male group, while 10% (n=162) were in the Low Risk white male group. Only 2% (n=38) of youths were in the High Risk white female group, compared to 8% (n=137) in the Low Risk white female group. Relatedly, the prevalence of High Risk youth within each gender-race/ethnicity group differs. The highest proportion of High Risk youth within gender-race/ ethnicity group was for Hispanic females (67.6%), followed by African American males (61.2%), African American females (32.8%), white males (26.7%), Hispanic males (25.8%), and white females (21.7%), respectively.
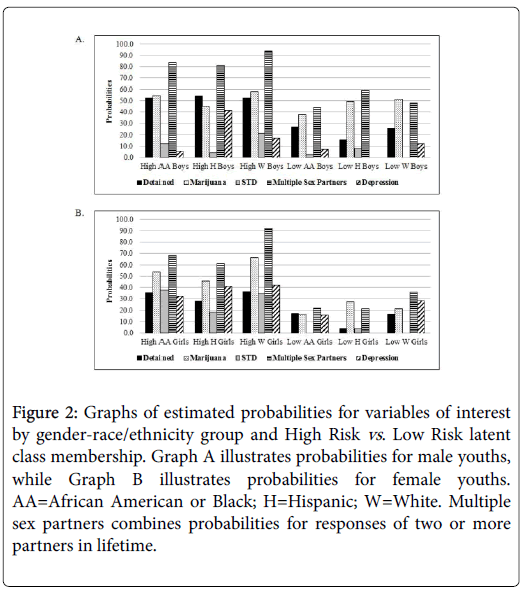
Further, the prevalence (based on probability scale estimates) of the health risk variables varies across High Risk and Low Risk youth in the six subgroups. For example, elevated depression is more salient among African American High Risk females, Hispanic High Risk males, Hispanic High Risk females, and white High Risk females, than among the other youth risk groups. Figure 2 illustrates the mean probability estimates for post-JAC secure detention, marijuana positive, STD positive, two or more sexual partners, and elevated depression for the two-class LCA results across the six gender-race/ethnicity subgroups. For post-JAC secure detention, High Risk youths have higher likelihood of being detained than Low Risk youth. Boys illustrate slightly higher probabilities of secure detention than girls, regardless of latent class membership.
Figure 2: Graphs of estimated probabilities for variables of interest by gender-race/ethnicity group and High Risk vs . Low Risk latent class membership. Graph A illustrates probabilities for male youths, while Graph B illustrates probabilities for female youths. AA=African American or Black; H=Hispanic; W=White. Multiple sex partners combines probabilities for responses of two or more partners in lifetime.
For positive marijuana UA results, the probabilities are similar across gender for the High Risk class, but about twice as likely for boys in the Low Risk class compared to girls in the Low Risk class. For STD positive test results, the probabilities are higher in the High Risk class compared to the Low Risk class and these probabilities appear to be gendered, with girls having higher rates of STD infection than boys in the sample. For multiple (two or more) sexual partners, boys and girls in the High Risk class have similar rates, but girls in the Low Risk group have lower rates than their male counterparts. For depression, African American and white girls have higher rates of depression than their male counterparts, and the rates are higher for High Risk girls than Low Risk girls. The elevated depression rates are similar for Hispanic boys and girls, and among the highest rates across the gender-race/ethnicity groups.
Relationship of age to the health risk variables for each gender-race/ethnicity group
This study sought to assess the relationship of age to the latent classes within each gender-race/ethnicity group. Unfortunately, empty cells in the joint distribution of the categorical latent variables and age for one or more of the groups prevented reliable analyses of these data.
As an alternative, for each gender-race/ethnicity group, the bivariate relationship between age and each health risk variable was examined. Table 4 reports these results. As can be seen, except for the significant, positive relationship between age and number of lifetime sexual partners in each gender-race/ethnicity group, age is not consistently related to the other risk factors.
| Variable | Black Males | Black Females | Hispanic Males | Hispanic Females | White Males | White Females |
|---|---|---|---|---|---|---|
| Post JAC release | 0.04 | 0.01 | -0.07 | 0.04 | 0.14 | -0.02 |
| Marijuana test | 0.06 | 0.23** | 0.09 | 0.01 | 0.13 | 0.47*** |
| STD test | 0.11 | 0.16 | 0.42* | -0.01 | 0.37* | 0.16 |
| Sex partners | 0.37*** | 0.43*** | 0.40*** | 0.49*** | 0.43*** | 0.48*** |
| Elevated depression | 0.01 | -0.01 | 0.04 | 0.13 | 0 | 0.08 |
| Note: JAC=Juvenile Assessment Center; Two-tailed p-values: *p<0.05; **p<0.01; ***p<0.001 | ||||||
Table 4: Correlations between age and post jac release and health risk factors by gender-race/ethnicity group.
Discussion
The purpose of this study was to examine heterogeneity in certain health risk factors among justice-involved youth across gender-race/ ethnicity subgroups. Latent class analysis was used to examine heterogeneity in the health risk factors of post-intake release status, marijuana use, STD infection, number of lifetime sexual partners, and elevated depression symptoms across six gender-race/ethnicity groups (Black male, Black female, Hispanic male, Hispanic female, white male, and white female).
The LCA results indicated the health risk characteristics across the gender-race/ethnicity groups were best described as falling into two classes: High Risk (reflected in elevated levels of the health risk variables) vs. Low Risk (reflected in comparably lower levels of health risk variables). There were a few exceptions to this pattern of findings, which were discussed in the results section. Generally, the proportions of youths with health problems varied, depending on the latent class membership (i.e., High Risk vs. Low Risk) and gender-race/ethnicity group.
Prior to conducting analyses to address these three research questions, we completed univariate analyses, comparing the six gender-race/ethnicity groups on age, UA positive test results for marijuana, elevated depression, number of reported lifetime sexual partners, post-JAC release status, and STD test results. The six comparison groups were similar in age. As noted earlier, male youth in each race/ethnic group had higher marijuana test positive rates, reported more lifetime sexual partners, and had higher rates of placement in secure detention, than female youth. Female youth had higher rates of elevated depression and higher STD positive rates, than the males-reflecting a more serious health burden regardless of race/ ethnic background.
The six gender-race/ethnicity groups differed in overall risk levels. The group with the highest prevalence of health risks was African American males, who accounted for nearly a quarter of all youth in the study. Further, the prevalence of High Risk youth within each genderrace/ ethnicity group varied, with higher prevalence indicated for African American males (61%) and Hispanic females (68%). These youth appear to be most in need of intervention services.
The LCA results found the magnitude of relationship of the health risk variables differed across High Risk and Low Risk youth in the six gender-race/ethnicity groups. These group differences in magnitude, or prevalence, of health risk factors highlight behavioral domains on which intervention efforts should focus. For example, addressing depression issues among African American High Risk females, Hispanic High Risk males, Hispanic High Risk females, and white High Risk females would seem more imperative, than for the other gender-race/ethnicity groups in our study.
Our findings underscore the importance of conducting ongoing assessments of youth entering the justice system to-among other things-identify groups at elevated risk and service need, and to inform the specific services provided to them. Such an effort will enable service providers to be more efficient in directing appropriate services to new subgroups, as well as informing shifts in service delivery efforts as the sociodemographic composition of the surrounding communities served by intake facilities change.
Relatedly, our results highlight the need for more holistic intervention, rather than one-problem-at-a-time approaches. As demonstrated in the research and our sample, high risk, justiceinvolved youth often experience elevated levels of risk on multiple health indicators. Therefore, interventions need to target multiple risk factors simultaneously.
Lastly, except for the significant, positive relationship between age and number of lifetime sexual partners, youth age showed no patterned relationship with any of the other health risk factors examined across the six gender-race/ethnicity groups. A significant, positive relationship between age and number of lifetime sexual partners, reflecting greater length of opportunity with more years of life might be expected as sexual maturity occurs across adolescence. Generally, however, age was not an important covariate for post-arrest placement, marijuana use, STD infection, or depressive symptoms across gender-race/ethnicity groups.
Conclusion
There are several strengths to our study. First, there were large numbers of male and female youth from diverse race/ethnicity groups involved in it, permitting analyses with considerable statistical power and precision of estimates. Second, the study is unusual in that biological data on both drug use and STDs were collected. These data were not subject to the social desirability bias youth in custody reflect in their answers to sensitive questions, such as their self-reporting of recent drug taking. This situation provided a unique opportunity to assess the relative importance of these factors on the health risk of male and female youth we studied.
At the same time, there are several limitations to our research. First, the analyses were conducted on cross-sectional data. Hence, no causal interpretations of our findings are possible. Second, the results of the study may not generalize to male and female youth arrested in other jurisdictions, reflecting different sociodemographic circumstances. Our results underscore the importance of replication in different populations across a variety of juvenile justice intake facilities. Third, the data on number of sexual partners and depression, although reflecting relationships that converge with the findings of other studies noted earlier, were based on self-reports.
We hope other jurisdictions will replicate our study. JACs, or similar centralized intake facilities, are ideal locations to conduct informed screening and service linkage for a diverse group of youth at the high risk end of the community continuum. JACs can serve as critical community public health and behavioral health resources, identifying and responding to the service needs of arrested youth, whose families often lack the resources to access these services on their own.
Acknowledgement
We are grateful for the support of the Florida Department of Children and Families, and the Central Florida Behavioral Care Network.
References
- Abram KM, Teplin LA, McClelland GM, Dulcan MK (2003) Comorbid psychiatric disorders in youth in juvenile detention. Arch Gen Psychiatry 60: 1097-1108.
- McClelland GM, Elkington KS, Teplin LA, Abram KM (2004) Multiple substance use disorders in juvenile detainees. J Am Acad Child Adolesc Psychiatry 43: 1215-1224.
- Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, et al. (2005) Major mental disorders, substance use disorders, comorbidity, and HIV/AIDS risk behaviors in juvenile detainees. Psychiatr Serv 56: 823-828.
- Canterbury RJ, McGarvey EL, Sheldon-Keller AE, Waite D, Reams P, et al. (1995) Prevalence of HIV-related risk behaviors and STDs among incarcerated adolescents. J Adolesc Health 17: 173-177.
- Karnik NS, Jones PA, Campanaro AE, Haapanen R, Steiner H (2006) Ethnic variation of self-reported psychopathology among incarcerated youth. Community Ment  Health J 42: 477-486.
- Bright AL, Kohl PI, Jonson-Reid M (2014) Females in the juvenile justice system: Who are they and how do they fare? Crime Delinq 60: 106-125.
- Belenko S, Knight D, Wasserman GA, Dennis ML, Wiley T, et al. (2017) The Juvenile Justice Behavioral Health Services Cascade: A new framework for measuring unmet substance use treatment services needs among adolescent offenders. J Subst Abuse Treat 74: 80-91.
- Schmiege SJ, Bryan AD (2016) Heterogeneity in the relationship of substance use to risky sexual behavior among justice-involved youth: A regression mixture modeling approach. AIDS Behav 20: 821-832.
- Wasserman GA, McReynolds LS, Ko SJ, Katz LM, Carpenter JR (2005) Gender differences in psychiatric disorders at juvenile probation intake. Am J Public Health 95: 131-137.
- Dembo R, Briones-Robinson R, Wareham J, Winters KC, Ungaro R, et al. (2016) A longitudinal study of truant youths' involvement in sexual risk behavior. J Child Adolesc Subst Abuse 25: 89-104.
- Dembo R, Faber J, Cristiano J, DiClemente RJ, Krupa JM, et al. (2017) Health risk behavior among male and female justice involved youth: Exploratory, multi-group latent class analysis. Subst Use Misuse 52: 1751-1764.
- DiClemente RJ, Santelli JS, Crosby RA (2009) Adolescent health: Understanding and preventing risk behaviors. John Wiley & Sons, New York, USA.
- Freudenberg N (2009) In Adolescent Health: Understanding and preventing risk behaviors, Jossey-Bass: San Francisco, California, USA.
- Hong JS, Voisin DR, Crosby S (2015) A review of STI/HIV interventions for delinquent and detained juveniles: An application of the social-ecological framework. J Child Fam Studies 24: 2769-2778.
- Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA (2002) Psychiatric disorders in youth in detention. Arch Gen Psychiatry 59: 1133-1143.
- Dembo R, Schmeidler J, Pacheco K, Cooper S, Williams LW (1998) The relationships between youths' identified substance use, mental health or other problems at a juvenile assessment center and their referrals to needed services. J Child Adolesc Subs Abuse 6: 23-54.
- Wells EA, Morrison DM, Gillmore MR, Catalano RF, Iritani B, et al. (1992) Race differences in antisocial behaviors and attitudes and early initiation of substance use. J Drug Educ 22: 115-130.
- National Institute on Drug Abuse (2014) Principles of drug abuse treatment for criminal justice populations a research-based guide, U.S. Department of Health and Human Services, Washington DC, USA,
- Snyder HN, Sickmund M (2006) Juvenile offenders and victims: 2006 national report. Office of Juvenile Justice and Delinquency Prevention, Washington DC, USA.
- Dembo R, Walters W (2012) In understanding and treating adolescent substance use disorders, civic research institute: Kingston, New Jersey, USA.
- Dembo R, DiClemente RJ, Brown R, Faber J, Cristiano J, et al. (2016) Health coaches: An innovative and effective approach for identifying and addressing the health needs of juvenile involved youth. J Commu Med Health Educ 6: 1-7.
- Dembo R, Brown R (1994) The hillsborough county juvenile assessment center. J Child Adolesc Subs Abuse 3: 25-44.
- Chacko M, Barnes C, Wiemann C, DiClemente R (2004) Implementation of urine testing for chlamydia (CT) and gonorrhea (NGC) in a community clinic. J Adolesc Health 34: 146-146.
- Komro KA, Tobler AL, Maldonado-Molina MM, Perry CL (2010) Effects of alcohol use initiation patterns on high-risk behaviors among urban, low income, young adolescents. Prev Sci 11: 14-23.
- Centers for Disease Control and Prevention MMWR (2015) Youth risk behavior surveillance-United Stated, 2015. Department of Health and Human Services, Atlanta, USA.
- Radloff LS (1977) The CES-D scale: A self-report depression scale for research in the general population. APM 1: 385-401.
- Dembo R, Faber J, Cristiano J, DiClemente RJ, Krupa JM, et al. (2018) Psychometric evaluation of a brief depression measure for justice-involved youths: A multigroup comparison. J Child Adolesc Subs Abuse 27: 146-155.
- Brown JL, Sales JM, Swartzendruber AL, Eriksen MD, DiClemente RJ, et al. (2014) Added benefits: Reduced depressive symptom levels among African-American female adolescents participating in an HIV prevention intervention. J Behav Med 37: 912–920.
- Santor DA, Coyne JC (1997) Shortening the CESD to improve its ability to detect cases of depression. Psycholog Assessm 9: 233–243.
- Muthén LK, Muthén BO (1998-2017) Mplus user’s guide. (8th edn.). Muthén and Muthén, Los Angeles, California, USA.
- Dayton CM (1998) Latent class scaling analysis. Sage Publications, Thousand Oaks, California, USA.
- Enders CK (2010) Applied missing data analysis. Guilford Press, New York, New York, USA.
- Rubin DB (1987) Multiple imputation for nonresponse in surveys. John Wiley and Sons, New York, New York, USA.
- Schafer JL, Olsen MK (1998) Multiple imputation for multivariate missing-data problems: A data analyst’s perspective. Multivariate Behav Res 33: 545-571.
- Lo Y, Mendell N, Rubin D (2001) Testing the number of components in a normal mixture. Biometrika 88: 767-778.
- McLachlan G, Peel D (2000) Finite mixture models. Wiley, New York, New York, USA.
- Nylund KL, Asparouhov T, Muthén BO (2007) Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Modeling 14: 535-569.
Citation: Dembo R, Faber J, Wareham J, Krupa JM, Schmeidler J, et al. (2018) Heterogeneity in the Prevalence of Health Risk Factors among Justice-Involved Adolescents: The Intersectionality of Gender and Race/Ethnicity. J Community Med Health Educ 8: 629. DOI: 10.4172/2161-0711.1000629
Copyright: © 2018 Dembo R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3556
- [From(publication date): 0-2018 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 2718
- PDF downloads: 838