Herpetic Encephalitis Lead to Acute Retinal Necrosis
Received: 16-Oct-2017 / Accepted Date: 24-Oct-2017 / Published Date: 26-Oct-2017 DOI: 10.4172/2314-7326.1000266
Abstract
Objective: The purpose of this study is to enhance the known onset time of acute retinal necrosis syndrome and explain the reason of different prognosis of acute retinal necrosis. Method: Three patients were examined by neurology and ophthalmology. Possible pathogenesis was analyzed. Results: The 3 patients were 37-year-old male, 49-year-old female and 47-year-old male respectively. After being presented at diagnosis, they had herpetic encephalitis associated with acute retinal necrosis syndrome and all the examinations are consistent with herpetic infection. Conclusion: The key to influence the vision is the vision correction at preliminary diagnosis and central retinal artery occlusion and pathogenesis in the acute phase may relate to chemotaxis ability of T cell. Keywords: Acute retinal necrosis; Herpes simplex virus; Herpetic encephalitis
Introduction
Acute retinal necrosis (ARN) is a devastating ocular disease with a very disappointing visual outcome which is characterized by retinal vasculitis and hemorrhages, focal retinal necrosis, vitreous and aqueous inflammation, and optic neuritis. It is primarily the result of human viral infections by varicella zoster virus (VZV), herpes simplex virus (HSV) types 1 and 2 and these viruses also represent an important cause of encephalitis.
We present three patients who developed the clinical picture of ARN 9 and 10 and 12 days concurrent herpetic encephalitis.
Case Report
The 3 patients were 37-year-old man, 49-year-old woman and 47- year-old man who admitted to affiliated Hospital of Qing Dao University on February 10, February 25 and July 19, 2015 respectively, with a history of fever, headache and dizzy. The results of lumbar puncture, magnetic resonance imaging (MRI), and electroencephalography (EEG) examination (Table 1) were consistent with herpetic infection. All patients presented at diagnosis had herpetic encephalitis and were treated with intravenous acyclovir 15-30mg (kg/d) three times a day.
| Cases | MRI | EEG | Cerebrospinal fluid examination | ||
|---|---|---|---|---|---|
| CSF-pressure (mmH2O) |
WBC count (× 109/L) |
CSF-protein (g/L) |
|||
| 1 | no obvious anomaly | Diffuse slow waves** | 200 | 0.05 | 0.959 |
| 2 | no obvious anomaly | Diffuse slow waves*** | 210 | 0.009 | 0.65 |
| 3 | Meet HE* | Diffuse slow waves**** | 200 | 0.01 | 0.623 |
Notation
*Diffusion Weighted Imaging (DWI) revealed hyperintensity in the left basal ganglia and bilateral corona radiata. **Moderate abnormality and 5-7 hz moderate to low amplitude θ activity. ***Moderate abnormality and diffuse 2.5-4 hz moderate to high amplitudeactivity. ****Frontal and temporal region have more moderate to high of 2-4hz irregular diffuse slow wave, and more moderate to high 2.5-4hz amplitude of sharp wave complexes distribution or continuous emergence
Table 1: The results of cerebrospinal fluid (CSF), MRI, EEG examination in 3 patients.
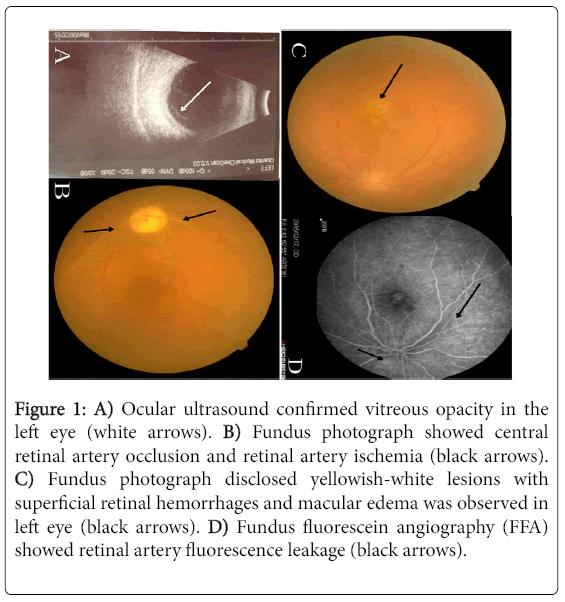
However, those patients had a sudden loss of vision in two eyes on the ninth and tenth and twelfth day of admission respectively. Ophthalmologic examination disclosed bilateral pupil were divergent and nonreactive to light in patient two and three. Ocular ultrasound of patient two confirmed bilateral vitreous opacity (Figure 1A) and fundus photograph showed central retinal artery occlusion (CRAO) and retinal artery ischemia (Figure 1B). In patient one, visual acuities on presentation were 0.04 oculus dexter (OD) and 0.2 oculus sinister (OS). Examination of the right eye revealed vitreous opacity, and fundus photograph disclosed yellowish-white lesions with superficial retinal hemorrhages and macular edema was observed in left eye (Figure 1C). Fundus fluorescein angiography (FFA) showed retinal artery fluorescence leakage (Figure 1D). A clinical diagnosis of acute retinal necrosis syndrome (ARN) was made. All the patients were treated with intravenous glucocorticoid progressively diminished and then took it orally.
Figure 1: A) Ocular ultrasound confirmed vitreous opacity in the left eye (white arrows). B) Fundus photograph showed central retinal artery occlusion and retinal artery ischemia (black arrows). C) Fundus photograph disclosed yellowish-white lesions with superficial retinal hemorrhages and macular edema was observed in left eye (black arrows). D) Fundus fluorescein angiography (FFA) showed retinal artery fluorescence leakage (black arrows).
A 17 months follow-up, visual acuities of the first patient is 0.45 right eye and 1.0 left eye, and the second patient has bilateral retinal detachment. In the following 6 months, the third patient has optic nerve necrosis in both eyes and visual acuity is not restored.
Discussion
Acute retinal necrosis (ARN) caused by herpes simplex virus (HSV) most occurs in association with or many years after HSV encephalitis which have been recorded. Intervals of herpetic encephalitis combined with ARN was 20 days to 5 months, and the longest was 20 years [1]. The explanation for such prolonged intervals includes the possibility of persistent latent virus in the CNS with spreading to the eye via the optic nerve and the presence of latent virus in the ocular tissue since the time of primary infection [2]. Different from other cases, our cases enhance the known onset time of ARN which was occurred after HE. Those patients who were immune-competent in our study occurred ARN in the acute phase of herpetic encephalitis and the earliest onset time is the ninth day of HIM. Maybe the herpes simplex virus strain type of patients infected has weak chemotaxis ability to T cell, so T cell cannot response rapidly and prevent virus from damaging the eye. Especially in case three, an intensive HE, a large number of viral was replicated and the virus may have been migrated by axonal transport, through the optic nerves, to produce optic nerve necrosis at inchoate development of ARN. In addition, Smith et al. found that herpes viruses is spread via bidirectional fast-axonal transport to sensory neurons [3]. Consequently, this virus can cause recurrent episodes of ARN [4,5] and the key to prevent recurrent episodes of ARN is to restrain the reactivation of latent virus.
Acyclovir is a potent antiviral action against varicella zoster and herpes simplex and it is effective against actively replicating virus [6]. In our cases, though all patients were given this treatment at the time of their HE and added the systemic corticosteroids when the ARN was confirmed, two patients who were no light perception in each eye after vision acuity correction had the worst outcome while the one that was 0.04 OD and 0.2 OS in spite of yellowish-white lesions under macula lutea had a better vision. A recent research disclosed that the key of influence the vision is the vision correction at preliminary diagnosis and central retinal artery occlusion (CRAO) [7]. This finding explains the cause of different prognosis of ARN in our cases and there is reason to believe that it is irrelevant for prognosis of ARN whether or not association with HE and the different onset time. Furthermore, treatment of HE does not prevent ARN [8]. This is concordant with our cases which were admitted to the hospital after the introduction and so were all given this treatment at the time of their HE whereas it didn’t prevent the ARN occur.
Conclusion
In conclusion, ARN, as one of the complications of serious HE, has a high morbidity rate and influence the quality of patients’ life. Both neurologists and ophthalmologists should pay a great deal of attention to this vision-threatening complication of HE, especially for those patients who have the anamnesis of HE and develop the discomfort of eyes. In consideration of HE may indicate a high incidence rate of ARN, the continuous application of antiviral drug may have an important significance of prophylaxis.
References
- Kamel OR, Galloway GD, Trew DR (2000) Delayed onset acute retinal necrosis 20 years following herpetic encephalitis. Eye 14: 788-788.
- Pavesio CE, Conrad DK, Mccluskey PJ, Mitchell SM, Towler HMA, et al. (1997) Delayed acute retinal necrosis after herpetic encephalitis. Br J Ophthalmol 81: 415-416.
- Smith GA, Gross SP, Enquist LW (2001) Herpesviruses use bidirectional fast-axonal transport to spread in sensory neurons. ProcNatlAcadSci U S A 98: 3466-3470.
- Perry JD, Girkin CA, Miller NR, Kerr DA (1998) Herpes simplex encephalitis and bilateral acute retinal necrosis syndrome after craniotomy. American journal of ophthalmology 126: 456-460.
- Klein A, Lefebvre P (2007) Three consecutive episodes of acute retinal necrosis due to herpes simplex-1 over twelve years following herpetic encephalitis. OculImmunolInflamm 15: 411-413.
- Laskin OL (1984) Acyclovir: Pharmacology and clinical experience. Archives of Internal Medicine 144: 1241-1246.
- Wen X, Zhang MF, Dong FT, Zhao C (2013) Factors associated with visual prognosis of acute retinal necrosis syndrome. Chinese Journal of Ophthalmology 49: 207-211.
- Vandercam T, Hintzen RQ, De Boer JH, Der Lelij AV (2008) Herpetic encephalitis is a risk factor for acute retinal necrosis. Neurology 71: 1268-1274.
Citation: Hu Q, Teng W, Hao F, Wang N (2017) Herpetic Encephalitis Lead to Acute Retinal Necrosis. J Neuroinfect Dis 8: 266. DOI: 10.4172/2314-7326.1000266
Copyright: © 2017 Hu Q, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4032
- [From(publication date): 0-2017 - Dec 27, 2024]
- Breakdown by view type
- HTML page views: 3340
- PDF downloads: 692