Research Article Open Access
Hepatocellular Carcinoma Response to Local Regional Therapy; Correlations between Pre-Liver Transplants Imaging and Explant Pathology
Alghanem M, Driman D, Bashir O, Al Judaibi B, Kakani N, Marotta P and Qumosani K*
Multiorgans Transplant Unit, London Health Science Centre, Western University, London, Ontario, Canada
- Corresponding Author:
- Karim Qumosani
Assistance Professor
Western University, 339
Windermere Road, London, Ontario, N6A 5A5, Canada
Tel: 1-519-636-7616
Fax: 1-519-663-2907
E-mail: mailto:Karim.qumosani@lhsc.on.ca
Received date: June 15, 2016; Accepted date: June 26, 2016; Published date: June 29, 2016
Citation: Alghanem M, Driman D, Bashir O, Al Judaibi B, Kakani N, et al. (2016) Hepatocellular Carcinoma Response to Local Regional Therapy; Correlations between Pre-Liver Transplants Imaging and Explant Pathology. J Gastrointest Dig Syst 6:444. doi:10.4172/2161-069X.1000444
Copyright: © 2016 Alghanem M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
HCC; Mrecist; Liver transplant; Explant; Pathology
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background/Aim: Modified Response Evaluation Criteria in Solid Tumors (mRECIST) were developed to assess the response to treatment in patients with HCC, based on measuring the amount of viable tumor using dynamic imaging (CT/MRI). Our aim to compare the estimated viable HCC after locoregional therapy (LRT) by CT imaging and prior to liver transplant to the histopathological assessment of viable HCC in the hepatic explant. Methods: We prospectively evaluated 44 patients with HCC who underwent both LRT and liver transplantation at London health science center. Using mRECIST criteria, the response to LRT was assessed by two blinded radiologists and the percentage of necrosis was reported separately for the reference CT (rCT) done after the last LRT and prior to liver transplantation. The report obtained from each radiologist was combined then was compared to the findings of an expert pathologist reporting on viable tumour present and tumour necrosis in the hepatic explants. Both parties were blinded to prevent bias in the results. Results: A total of forty-one transplant recipients fulfilled the inclusion criteria for the study. At time of listing 100% were within total volume criteria, 86% within UCSF, and 68% within Milan. The average time from the last reference CT scan to liver transplant was 57.7 days; the average time from last LRT to reference CT was 72.5 days. Thirty-four recipients (83%) had accurate assessment for necrosis (mRECIST) within 20% comparing rCT to explant (i.e. concordant). Ninteen, 19 (46%) of the 41 predicted 100% concordance. Only 7/41 (17%) had a poor concordance (>50%) between histology and reference CT images. positive correlation was detected with the correlation coefficient is calculated as 0.5723. Our study demonstrated CT-pathologic correlation in predicting number and size of tumors with Correlation coefficient 0.64 and 0.31, respectively. However, there was poor correlation in predicting total volume with correlation coefficient is calculated as 0.014. Conclusion: Dynamic CT is an accurate tool to evaluate the tumour response prior to liver transplantation and the likelihood of underestimating the tumour burden is low. With expert radiologists and pathologists, the correlation is acceptable and supports the ongoing use of frequent dynamic imaging to evaluate responses to LRT and determining transplant eligibility.
Keywords
HCC; Mrecist; Liver transplant; Explant; Pathology
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common cancer in the world and ranks third in cancer related mortality [1]. Different modalities can be used for treatment according to Barcelona algorithm [2]. Locoregional therapy (LRT) which includes radiofrequency ablation (RFA) and Trans-arterial chemotherapy embolization (TACE) are used to treat patients through different stages of the disease according to BCLC algorithm [3]. At early stages of the tumor, RFA can be used with curative intent while TACE is considered a palliative treatment if patient deemed not a transplant candidate. In pretransplant setting, these therapies frequently used as a bridge to transplant or for down staging the tumor to be within acceptable criteria for transplant. The ultimate goal of LRT to induce necrosis of the tumor. This can be achieved either by thermocoagulation (RFA) or by arterial occlusion and local administration of chemotherapy (TACE). The degree of tumor necrosis is a predictor of treatment success. Partial necrosis within the tumor leads to higher rate of tumor recurrence after liver transplantation [4]. Achieving complete necrosis is associated with lower rate of recurrence and improved survival post liver transplantation [5,6].
The radiological assessment of tumor response to Locoregional therapy has evolved to include the viability of tumor in comparison to the previously used criteria (RECIST and WHO criteria), which are based on the sum of the greatest dimensional measurement of target lesions [7]. Modified Response Evaluation Criteria in Solid Tumors (mRECIST) criteria has been introduced to overcome the limitation of measuring the tumour size only by taking into account the residual viable tumor [8,9]. The treatment response categorized into four groups according to the extent of necrosis: complete response, partial response, stable disease, or progressive disease [10].
The accuracy of measuring the tumor necrosis after LRT on dynamic imaging is under investigation. The main objective of this study, to compare the estimated viable HCC after LRT by CT imaging and before liver transplant, to the histopathological assessment of viable HCC in the hepatic explant.
Materials and Methods
This is a single Centre, correlation analysis of a prospective study approved by the local Institutional Review Board (IRB). Between January 2010 to December 2015, we evaluated all patients at London Health Sciences Centre with known HCC who underwent LRT as bridging therapy prior to liver transplantation.
Patient selection
Inclusion criteria included any patients with proven diagnosis of HCC either, by histopathology or dynamic imaging (CT/MRI). All participants were eligible for liver transplant based on HCC tumor burden within Ontario criteria which corresponds to total volume of 115 mm or less and alpha fetoprotein less than 400 [11]. The patients were listed for liver transplant with MELD exceptional points of 22 and received LRT as bridging therapy to transplant.
Treatment
The decision to proceed with bridging therapy prior to liver transplant was based on the consensus of a multidisciplinary team. In case of RFA, the procedure performed through percutaneous approach by using ultrasound guidance to insert 18-gauge, cooled-tip electrode with a 2 or 3 cm exposed tip which is attached to a radiofrequency generator. Radiofrequency energy delivered in pulses of 6-12 minutes and position changed in larger lesion to achieve complete ablation TACE involves identifying the blood vessels supplying the tumor during an angiogram and selectively delivering chemotherapeutic agent (doxorubicin 30 mg) mixed with Lipiodol followed by Embolization of the vessel for complete occlusion of blood supply.
Imaging and follow-up
Baseline CT was done before each LRT as part of assessment. A reference CT (rCT) was done within 3 months after therapy to assess response to LRT. The radiological response was evaluated using the mRECISTcriteria which are outlined in Table 1.
| Stable disease (SD) | Any cases that do not qualify for either partial response or progressive disease |
| Progressive disease (PD) | An increase of at least 20% in the sum of the diameters of viable (enhancing) target lesions, taking as reference the smallest sum of the diameters of viable (enhancing) target lesions recorded since treatment started |
| Complete response (CR) | Disappearance of any intra tumoral arterial enhancement in all target lesions |
| Partial response (PD) | At least a 30% decrease in the sum of diameters of viable (enhancement in the arterial phase) target lesions, taking as reference the baseline sum of the diameters of target lesions. |
Table 1: mRECIST, modified Response Evaluation Criteria in Solid Tumours.
Two blinded radiologists appraised the response to LRT and the percentage of necrosis was reported separately for each R CT done after each LRT and prior to liver transplantation. The results from the radiologists were compared to the findings of an expert pathologist reporting on viable tumour present and tumour necrosis in the hepatic explants. The pathologist determined the tumor viability by examining the largest diameter of the treated HCC. Both parties were blinded so prevent bias in the results.
Outcome and statistical analysis
To quantify the correlation between pre-liver transplantation radiological imaging to histopathological findings post-liver transplantation, we applied statistical analysis to four main factors under both radiology and pathology methods, which are percentage of Necrosis, number of tumors, tumor size and total tumor volume. In addition, two statistical methodologies are carried out to get consistent and reliable results. Even though of patients under observation have multiple tumors, detailed information is only accessible for the 1st tumor. Thus most of our statistical analysis is based upon the 1st tumor’s information.
First, a direct calculation of Pearson product-moment correlation coefficient is conducted for each of the four main factors. This statistic measures the linear dependence between two variables and lies between -1 and +1, with -1 indicating extremely negative correlation or moving in the opposite direction, and +1 indicating extremely positive correlation or moving in the same direction. Also, a corresponding plot of each main factor is provided to compare the movement of both results under both radiology and pathology visually.
Second, we assume there is a linear relationship between radiology and pathology results for each main factor and then analyzes how good this linear model is, or how strong the two variables of radiology and pathology results are linearly related. Through this regression analysis, we focus on the “Multiple R” in the output, which indicates the quality of the linear relationship. This Multiple R varies from 0 to 1 with larger number indicating stronger linear relationship. Also, a corresponding scatter plot with fitted linear trend line is provided for visual perception. Each dot on the plot represents a patient’s information with horizontal axis of radiology result and vertical axis of pathology results.
Results
A total of 44 transplant recipients fulfilled the inclusion criteria for the study. Three patients were excluded due to absence of a rCT after LRT and prior to liver transplant. The median age at diagnosis was 59.4 years.
There was male predominance in our patients (85%). The major indication for liver transplant in our group was liver cirrhosis secondary to hepatitis C (73%) (Table 2). Summarize the baseline characteristics of our cohort.
| Mean Age at transplant | 59.4 years |
| Gender | |
| Male | 35/41 (85%) |
| Female | 6/41 (15%) |
| Diagnosis | |
| HCV | 30/41 (73%) |
| NASH | 4/41 (9.75%) |
| ASH | 3/41 (7.3%) |
| Other | 4/41 (9.75%) |
| AFP (Mean) | 71 ng/mL |
| Transplant Criteria(Radiology) | |
| rOntario | 41/41(100%) |
| rMilan | 30/41 (68%) |
| rUCSF | 37/41 (86%) |
| Transplant Criteria(Pathology) | |
| pOntario | 41/41 (100%) |
| pMilan | 21/41 (50%) |
| pUCSF | 33/41 (80%) |
| Local regional Therapy (LRT) | |
| TACE | 31/41 (75.5%) |
| RFA | 10/41 (24.5%) |
| No. of tumors | |
| Radiology | 2.1(1-6) |
| Pathology | 1.9(1-4) |
Table 2: Summarize the baseline characteristics of our cohort.
At time of listing, all of our patients were within Ontario criteria. Majority of patients were within UCSF (86%) and Milan (68%).The HCC was single lesion was in 50% and only one lobe was affected in 70%. Most of our patients were treated with TACE (75%).
13 patients (31%) had more than one LRT (12 had >1 TACE and two had >1 RFA). No patients progressed beyond transplant criteria. The average time frame from the last reference CT scan to liver transplant was 57.7 days; the average time from last LRT to reference CT was 72.2 days.
Using mRECIST criteria for radiological evaluation of Tumor necrosis, 29 (70%) and 8 (19.5%) patients achieved complete response (CR) and partial response (PR), respectively. The histopathological assessment of liver explants revealed 24 (58.5%) and 14 (34%) patients with complete and partial response, respectively. Evaluation of tumor response summarized in Table 3.
| Complete response | Partial response | Stable disease | |
|---|---|---|---|
| Radiological response | 29 (70%) | 8 (19.5%) | 3 (7%) |
| Pathological Response | 24 (58.5%) | 14 (4%) | 3 (7%) |
Table 3: Evaluation of tumor response according to mRECIST criteria.
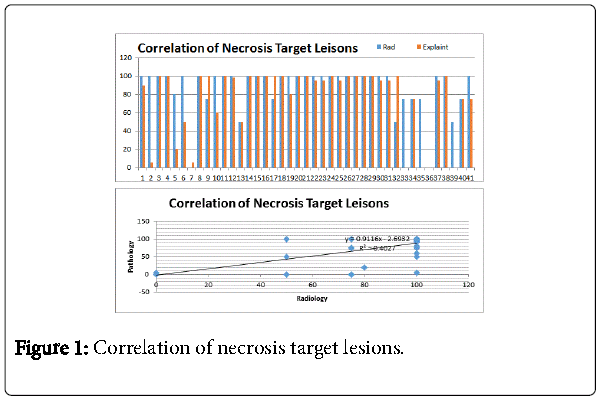
Thirty-four recipients (83%) had accurate assessment for necrosis (mRECIST) within 20% comparing rCT to explant (i.e. concordant). Twenty (58%) of the 34 predicted 100% concordance. Only 7 patients (17%) had a poor concordance (>50%) between histology and reference CT images. Comparing necrosis using mRECIST on imaging to pathological assessment of necrosis showed good correlation (Correlation Coefficient is calculated as 0.6648) (Figure 1).
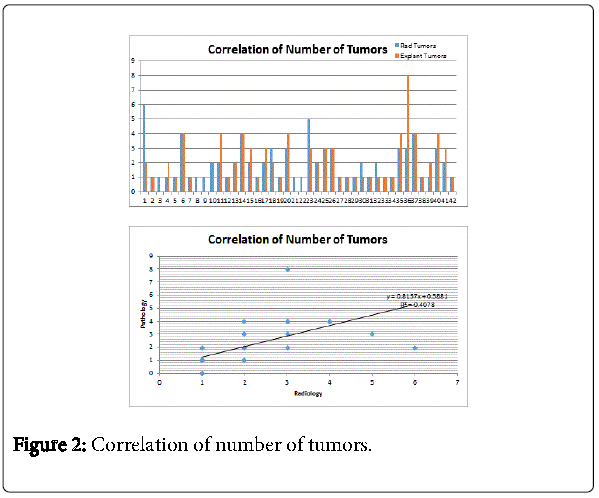
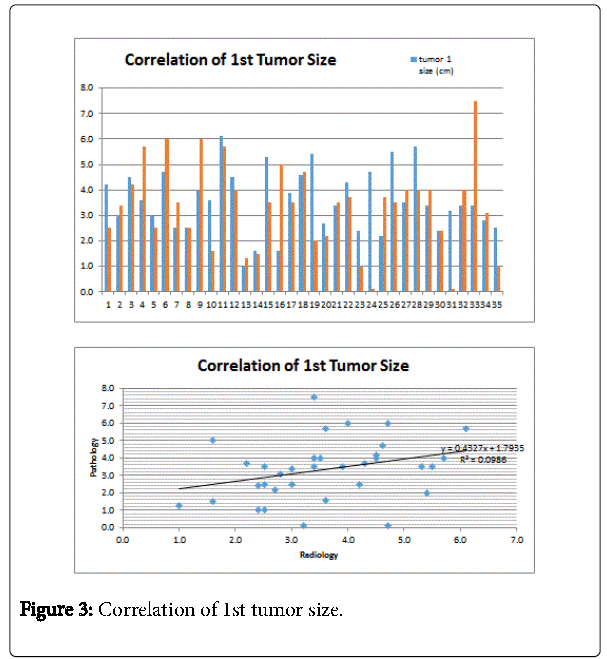
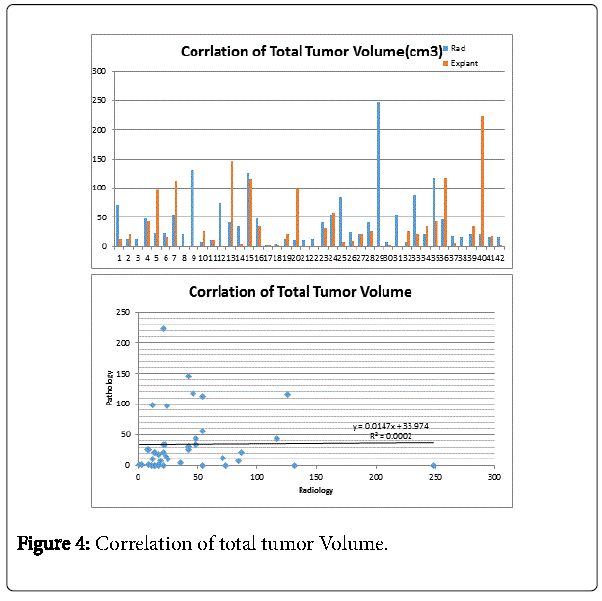
Dynamic CT was accurate in assessing the number of target lesions compared to Pathology (Correlation Coefficient 0.6648) (Figure 2). The size of 1st tumor was only obtained in 35 patients. From these patients, the size measurement on dynamic CT corresponds well with the histopathological findings (Correlation Coefficient 0.5616) (Figure 3). The predicted total tumor volume from dynamic CT showed weak association with the predicted value from histopathology (Correlation Coefficient 0.2379) (Figure 4).
Discussion
EASL-AASLD guidelines adopted the modified RECIST (mRECIST) criteria which takes into account the viability of tumor on dynamic imaging (CT/MRI) to accurately predict response to locoregional treatment. mRECIST criteria provided significantly better prognostic value compared to other methods of assessment. A study by Gillmore et al. comparing assessment of response to TACE by conventional RECIST criteria to mRECIST criteria showed significant difference in response between the two criteria. There was a survival benefit when deemed a responder by the mRECIST criteria [12]. These results confirmed by another study by Shim et al. Conventional RECIST criteria underestimates the response to LRT [13]. Forner et al. demonstrated the use of conventional RECIST criteria missed all the Complete responder and underestimated the partial responders [14].
The use of Modified RECIST criteria in assessing response to molecular therapy for HCC lead to more accurate evaluation of response. In open label study for Brivanib for HCC, Response to treatment according to mRECSIT criteria confers higher disease control and subsequently, increased overall survival [15]. In retrospective analysis for Sorafinib therapy, the prognosis of patient categorized as responder was better in the mRECIST group [16].
From our results, we can conclude that through the percentage of necrosis, number of tumors and tumor size, we derived a relative high correlation coefficient and hence a correlated relationship between the radiology and pathology results is implied. We also notice that the correlation coefficient of the total volume is not high enough. The reason for this is mainly due to the lack of the correlation for the 2nd or 3rd tumors sizes, while the total volume variable is considering all the tumors.
The limitation of this study include the extent of necrosis can be affected by interval between CT and liver transplant. In addition, the estimation of pathological necrosis was conducted by experienced pathologist but still represent a subjective measure.
Our results support the notion of dynamic CT as useful tool to estimate viable tumor after locoregional therapy and subsequently response. Similar study of 178 patients, sensitivity and specificity of CT in detecting complete necrosis were 87.5 and 68.9%, respectively [17]. Riaz et al., explored radiologic–pathologic correlation of HCC treated with internal radiation using yttrium-90 microspheres. The finding of the study showed Imaging including dynamic CT demonstrated a high predictive value for necrosis with complete response had a 100% PPV and specificity [18].
In conclusion, among expert radiologists and pathologists, the correlation is acceptable and supports the ongoing use of frequent dynamic imaging to evaluate responses to LRT and determining transplant eligibility.
References
- El-Serag HB (2011) Hepatocellular carcinoma. N Engl J Med 365: 1118-1127.
- Bruix J, Sherman M; American Association for the Study of Liver Diseases (2011) Management of hepatocellular carcinoma: an update. Hepatology 53: 1020-1022.
- Bruix J, Sherman M, Llovet JM (2001) Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL Conference. European Association for the Study of the Liver. J Hepatol 35: 421-430.
- Ravaioli M, Grazi GL, Ercolani G, Fiorentino M, Cescon M, et al. (2004) Partial Necrosis on Hepatocellular Carcinoma Nodules Facilitates Tumor Recurrence after Liver Transplantation. Transplantation 78: 12.
- Majno PE, Adam R, Bismuth H, Castaing D, Ariche A, et al. (1997) Influence of preoperative transarteriallipiodol chemoembolization on resection and transplantation for hepatocellular carcinoma in patients with cirrhosis. Annals of Surgery 226: 688-703.
- Sotiropoulos GC, Malago M, Molmenti EP, Radtke A, Brokalaki EI, et al. (2005) Disease course after liver transplantation for hepatocellular carcinoma in patients with complete tumor necrosis in liver explants after performance of bridging treatments. Eur J Med Res 10: 539-542.
- Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, et al. (2009). New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). European Journal of Cancer 45: 222-247.
- Lencioni R, Llovet JM (2010) Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis 30: 52-60.
- Lencioni R (2013) New data supporting modified RECIST (mRECIST) for Hepatocellular Carcinoma. Clin Cancer Res 19: 1312-1314.
- European Association for the study of the liver1; European Organisation For Research And Treatment Of Cancer (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56: 908-943.
- Toso C, Asthana S, Bigam DL, Shapiro AMJ, Kneteman NM (2009) Reassessing selection criteria prior to liver transplantation for hepatocellular carcinoma utilizing the Scientific Registry of Transplant Recipients database. Hepatology (Baltimore, Md.) 49: 832-838.
- Gillmore R, Stuart S, Kirkwood A, Hameeduddin A, Woodward N, et al. (2011) EASL and mRECIST responses are independent prognostic factors for survival in hepatocellular cancer patients treated with transarterial embolization. Journal of Hepatology, 55: 1309-1316.
- Shim JH, Lee HC, Kim SO (2012) Which response criteria best help predict survival of patients with hepatocellular carcinoma following chemoembolization? A validation study of old and new models. Radiology 262: 708-718.
- Forner A, Ayuso C, Varela M, Rimola J, Hessheimer AJ, et al. (2009) Evaluation of tumor response after locoregional therapies in hepatocellular carcinoma: are response evaluation criteria in solid tumors reliable? Cancer 115: 616-623.
- Park JW, Finn RS, Kim JS, Karwal M, Li RK, et al. (2011) Phase II, open-label study of brivanib as first-line therapy in patients with advanced hepatocellular carcinoma. Clin Cancer Res 17: 1973-1983.
- Edeline J, Boucher E, Rolland Y, Vaulon E, Pracht M, et al. (2012) Comparison of tumor response by Response Evaluation Criteria in Solid Tumors (RECIST) and modified RECIST in patients treated with sorafenib for hepatocellular carcinoma.Cancer 118: 147-156.
- Bargellini I, Bozzi E, Campani D, Carrai P, De Simone P, et al. (2013). Modified RECIST to assess tumor response after transarterial chemoembolization of hepatocellular carcinoma: CT-pathologic correlation in 178 liver explants. European Journal of Radiology 82: e212-218.
- Riaz A, Kulik L, Lewandowski RJ, Ryu RK, Giakoumis Spear G, et al. (2009), Radiological pathologic correlation of hepatocellular carcinoma treated with internal radiation using yttrium-90 microspheres. Hepatology 49: 1185-1193.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 12180
- [From(publication date):
June-2016 - Jul 09, 2025] - Breakdown by view type
- HTML page views : 11216
- PDF downloads : 964