Case Report Open Access
Hemosuccus Pancreaticus with Superior Mesenteric Artery Branch Pseudoaneurysm
Kevin C. Choong and John B. Ammori*Department of Surgery, University Hospitals Case Medical Center, Case Western Reserve University Cleveland, Ohio, USA
- *Corresponding Author:
- John B. Ammori
Department of Surgery
University Hospitals 11100 Euclid Avenue
Cleveland, OH 44106, USA
Tel: 216-844-1777
Fax: 216-286-3294
E-mail: mailto:john.ammori@UHhospitals.org
Received date: September 09, 2014; Accepted date: October 10, 2014; Published date: October 15, 2014
Citation: Choong KC and Ammori JB (2014) Hemosuccus Pancreaticus with Superior Mesenteric Artery Branch Pseudoaneurysm. J Gastroint Dig Syst 4:229. doi:10.4172/2161-069X.1000229
Copyright: © 2014 Choong KC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Introduction: Hemosuccus pancreaticus is a rare cause of gastrointestinal bleeding due to hemorrhage into the pancreatic duct, most commonly from pseudoaneurysms. Due to its rarity as well as the intermittent nature of the bleeding, diagnosis is commonly delayed. We report an interesting case of hemosuccus pancreaticus and the associated management issues. Case Report: We report a 32 year old man with 3 weeks of progressive melena found to have hemosuccus pancreaticus from an superior mesenteric artery branch pseudoaneurysm as a sequela of pancreatitis. The diagnosis was made with a combination of upper endoscopy, CT angiography. Ultimately this proved to be a management challenge as it required multiple angiographic embolizations to achieve hemostasis. Discussion: Hemosuccus pancreaticus was first coined by Sandblom in 1970. As it presents as gastrointestinal hemorrhage, initial workup is the same, with upper/lower endoscopy and CT angiographies as first line methods. Visceral angiography remains the gold standard for diagnosis of aneurysmal causes. Interventional angiography is the first line treatment of hemosuccus pancreaticus. However if this fails, operative intervention with vessel ligation or formal resection may be required for hemostasis.
Abstract
Introduction: Hemosuccus pancreaticus is a rare cause of gastrointestinal bleeding due to hemorrhage into the pancreatic duct, most commonly from pseudoaneurysms. Due to its rarity as well as the intermittent nature of the bleeding, diagnosis is commonly delayed. We report an interesting case of hemosuccus pancreaticus and the associated management issues.
Case Report: We report a 32 year old man with 3 weeks of progressive melena found to have hemosuccus pancreaticus from an superior mesenteric artery branch pseudoaneurysm as a sequela of pancreatitis. The diagnosis was made with a combination of upper endoscopy, CT angiography. Ultimately this proved to be a management challenge as it required multiple angiographic embolizations to achieve hemostasis.
Discussion: Hemosuccus pancreaticus was first coined by Sandblom in 1970. As it presents as gastrointestinal hemorrhage, initial workup is the same, with upper/lower endoscopy and CT angiographies as first line methods. Visceral angiography remains the gold standard for diagnosis of aneurysmal causes. Interventional angiography is the first line treatment of hemosuccus pancreaticus. However if this fails, operative intervention with vessel ligation or formal resection may be required for hemostasis.
Keywords
Hemosuccus pancreaticus; Pancreatitis; Pseudoaneurysm
Introduction
Hemosuccus pancreaticus, defined as hemorrhage into the gastrointestinal tract caused by a bleeding source in the pancreas, pancreatic duct, or adjacent structures that bleed into the pancreatic duct, is a rare cause of upper gastrointestinal bleeding. It is most commonly caused by rupture of a pseudoaneurysm into the main pancreatic duct and is associated with acute or chronic pancreatitis [1]. Other less common etiologies are iatrogenic, traumatic, pancreatic tumors, and arteriovenous malfomations. Due to its rarity as well as the intermittent bleeding that is associated, diagnosis is commonly delayed.
We report a case of hemosuccus pancreaticus and the associated management issues.
Case Report
A 32 year old man was taken to the emergency department with altered mental status after a syncopal episode. On further questioning, it was found that the patient had three weeks of melena and progressive weakness over the last two weeks. He denied any hematochezia, vomiting or hematemesis, but had been nauseated for the past two days. He denied any abdominal pain, prior trauma, or NSAID use. He has never had a prior gastrointestinal endoscopic examination. Importantly, the patient endorsed drinking 12 beers per day for the past 15 years.
Initial laboratory values revealed a hemoglobin and hematocrit of 4.1 g/dL and 12.3%, respectively, and a lactate of 5.8 mmol/L. He was admitted to the intensive care unit and transfused six units of packed red blood cells with appropriate response.
Diagnostic evaluation with a CT scan of the abdomen and pelvis with contrast revealed multiple cystic lesions in the pancreas, the largest of which was located in the left upper quadrant measuring 13.5 x 9.5 x 26 cm. There was no evidence of a pseudoaneurysm or contrast extravasation to suggest active bleeding. An esophagogastroduodenoscopy (EGD) was positive for candida esophagitis, for which he was started on fluconazole, as well as a small arteriovenous malformation in the stomach which was cauterized. Colonoscopy was negative for any stigmata of bleeding. A tagged RBC scan was performed which did not show any areas of active bleeding.
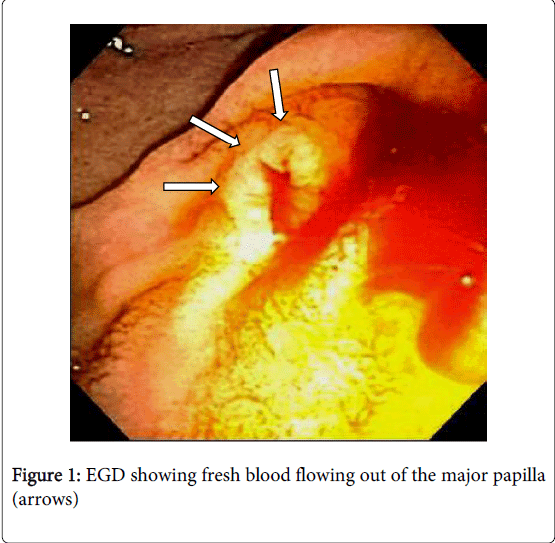
Due to continued gastrointestinal bleeding, the patient was transferred to our institution three days following his initial presentation for further evaluation and treatment. At transfer, he was hemodynamically stable, with a hemoglobin and hematocrit of 10 g/dL and 32%, respectively. Early the next day, the patient had another episode of hematochezia, prompting repeat EGD, which showed a normal esophagus and stomach, but with a new finding of fresh blood flowing out of the major papilla, consistent with a diagnosis of hemosuccus pancreaticus (Figure 1). This was followed up with a visceral angiogram which was negative for active hemorrhage or pseudoaneurysm formation from the celiac branches or the gastroduodenal artery. At this point, surgical consultation was initiated. CT angiography (CTA) was performed which demonstrated a large hemorrhagic pancreatic pseudocyst with intense inflammatory change, but without evidence of pseudoaneurysm or active extravasation. The patient continued to have a benign physical exam, with no signs of pseudoaneurysm or active extravasation that would be amenable to angiographic intervention and the decision was made to continue close clinical monitoring.
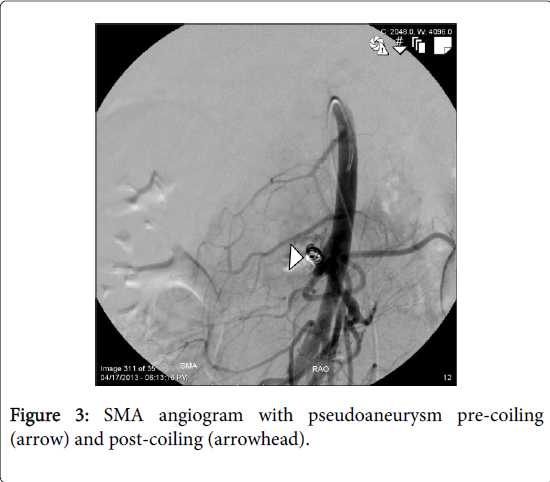
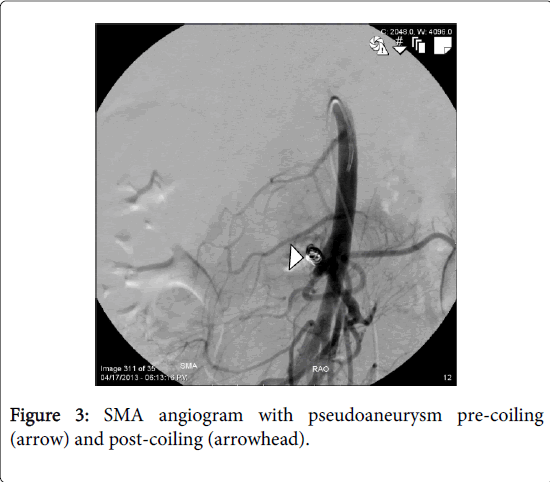
The patient continue to have a slowly down trending hematocrit over the next 10 days until a sudden drop accompanied by hematochezia. A CTA was repeated which revealed a pseudoaneurysm of a branch of the superior mesenteric artery (SMA) (Figure 2). A SMA angiogram was performed which confirmed an aneurysm of the second branch, which was successfully coil embolized (Figure 3).
Two days after angioembolization, the patient had another episode of GI bleeding. Repeat EGD showed a small amount of blood mixed with bile flowing from the papillary orifice. However, repeat angiogram showed no evidence of active hemorrhage or pseudoaneurysm. An empiric GDA embolization was performed at this point in an attempt to control the hemorrhage. The next evening, the patient had an additional episode of melena as well as hematemesis prompting a repeat CTA which showed no active extravasation, but did show a distended gallbladder containing hematoma. At this point, the decision was made to proceed with an open cholecystectomy given the CT findings of a gallbladder distended with hematoma and continued GI bleeding without other obvious source, as there was the possibility of direct hemorrhage into the gallbladder. The operation was uneventful and the gallbladder was found to be filled with blood clots. The patient did well post-operatively and was discharge on post-operative day number four to home in stable condition without additional hemorrhage after cholecystectomy.
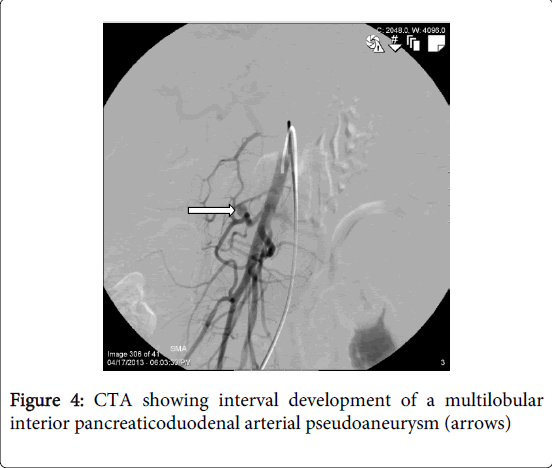
He returned to the emergency department on post-operative day number nine with hematemesis and upper abdominal pain with progressive malaise. He was tachycardic and found again to be profoundly anemic to a hemoglobin and hematocrit of 6 g/dL and 17.4%, respectively. A CTA showed an increase in the size of the previously coiled SMA branch pseudoaneurysm now measuring 3.6 x 2.5 cm (Figure 4).
Discussion
Bleeding from the pancreatic duct was first described by Lower and Farrell in 1931 [2]. However the term hemosuccus pancreaticus was coined by Sandblom in 1970 [3]. In 80% of cases, hemosuccus pancreaticus is a complication of pancreatitis, typically from a bleeding pseudoaneurysms into a pancreatic pseudocyst which communicates with the main pancreatic duct [4]. Hemorrhage in the setting of pancreatitis varies from 5-10%, but increases to 15-20% when a pseudoaneurysm is present. Mechanistically, this is thought to occur from pressure necrosis from a large pancreatic pseudocyst and/or auto-digestion of the vessel wall by pancreatic enzymes. The most common location of pseudoaneurysm formation with subsequent rupture is the splenic artery, less commonly the gastroduodenal, hepatic, or other small peri-pancreatic arteries [1,5]. SMA pseudoaneurysms as a cause of hemosuccus pancreaticus are rare, but have been reported to be present in 5% of cases of hemosuccus pancreaticus in one case series. Pseudoaneurysms of SMA branches are not specifically addressed in the same case series, although the incidence of pseudoaneurysm of the pancreaticoduodenal arteries was 27% [6].
SMA angiography confirmed a pseudoaneurysm of the inferior pancreaticoduodenal branches which was successfully coil embolized. He was observed for five days with no further evidence of gastrointestinal bleeding. He was discharged to home, has quit alcohol consumption following this episode, and has had no further bleeding episodes.
Initial workup for hemosuccus pancreaticus is no different from workup of any other gastrointestinal bleeding. Upper and lower GI endoscopy should be performed to assess for any signs of bleeding. In the case of hemosuccus pancreaticus, one would hopefully see bleed coming from the ampulla of Vater. However, bleeding is often intermittent, making diagnosis that much more difficult. Bleeding from the ampulla is only seen in 30% of cases [7]. CT angiography can be used to examine vasculature for aneurysms and pseudoaneurysms with sensitivity and specificity >90% [8]. This can be followed up with visceral angiography which is considered to be the gold standard in aneurysmal evaluation. However if there are no abnormal findings on angiography or if control of hemorrhage cannot be achieved with angiography, the next step would be surgical intervention. In the setting of pancreatitis, intra-operative determination of the site of hemorrhage and the appropriate site for resection can be difficult and the use of intra-operative ultrasound has been advocated [9].
Interventional angiography is first line for the treatment of hemosuccus pancreaticus. In this case there was a SMA pseudoaneurysm requiring three separate angiographic interventions. Rates of recurrent bleeding vary from 17-37% with further management with repeat embolization or with surgical intervention [5]. Several techniques for the operative management have been described, including: formal resection, intra-cystic ligation of the bleeding vessel, and vessel ligation with a separate drainage procedure [10]. Ultimately, good surgical judgment is critical in determining optimal treatment strategy.
In summary, we present an interesting case of hemosuccus pancreaticus with a SMA branch pseudoaneurysm requiring multiple angioembolizations to control the hemorrhage.
References
- Cahow CE, Gusberg RJ, Gottlieb LJ (1983) Gastrointestinal hemorrhage from pseudoaneurysms in pancreatic pseudocysts. Am J Surg 145: 534-541.
- Lower W, Farrell J (1931). Aneurism of the splenic artery. Report of a case and review of literature. Arch Surg 23:182-190.
- Sandblom P (1970) Gastrointestinal hemorrhage through the pancreatic duct. Ann Surg 171: 61-66.
- Ray S, Das K, Ray S, Khamrui S, Ahammed M, et al. (2011) Hemosuccuspancreaticus associated with severe acute pancreatitis and pseudoaneurysms: a report of two cases. JOP 12: 469-472.
- Boudghène F, L'Herminé C, Bigot JM (1993) Arterial complications of pancreatitis: diagnostic and therapeutic aspects in 104 cases. J VascIntervRadiol 4: 551-558.
- Bergert H, Hinterseher I, Kersting S, Leonhardt J, Bloomenthal A, et al. (2005) Management and outcome of hemorrhage due to arterial pseudoaneurysms in pancreatitis. Surgery 137: 323-328.
- Péroux JL, Arput JP, Saint-Paul MC, Dumas R, Hastier P, et al. (1994) [Wirsungorrhagia complicating chronic pancreatitis associated with a neuroendocrine tumor of the pancreas]. GastroenterolClinBiol 18: 1142-1145.
- Hyare H, Desigan S, Nicholl H, Guiney MJ, Brookes JA, et al. Multi-section CT angiography compared with digital subtraction angiography in diagnosing major arterial hemorrhage in inflammatory pancreatic disease. Eur J Radiol 2006;59: 295-300.
- Toyoki Y, Hakamada K, Narumi S, Nara M, Ishido K, et al. (2008) Hemosuccuspancreaticus: problems and pitfalls in diagnosis and treatment. World J Gastroenterol 14: 2776-2779.
- Bender JS, Bouwman DL, Levison MA, Weaver DW (1995) Pseudocysts and pseudoaneurysms: surgical strategy. Pancreas 10: 143-147.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15522
- [From(publication date):
October-2014 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 10921
- PDF downloads : 4601