Review Article Open Access
Health Coaches: An Innovative and Effective Approach for Identifying and Addressing the Health Needs of Justice Involved Youth
Dembo R1*, DiClemente RJ2, Brown R3, Faber J3, Cristiano J3 and Terminello A3
1Department of Criminology, University of South Florida, USA
2Rollins School of Public Health, Emery University, USA
3Agency for Community Treatment Services, Inc., Tampa, USA
- *Corresponding Author:
- Richard Dembo, Ph.D
Department of Criminology
University of South Florida
4202 East Fowler Avenue
Tampa, FL, 33620, USA
Tel: 813-974-2846
Fax: 813-974-5762
E-mail: rdembo@usf.edu
Received date: December 13, 2016; Accepted date: December 21, 2016; Published date: December 29, 2016
Citation: Dembo R, DiClemente RJ, Brown R, Faber J, Cristiano J, et al. (2016) Health Coaches: An Innovative and Effective Approach for Identifying and Addressing the Health Needs of Justice Involved Youth. J Community Med Health Educ 6:490. doi: 10.4172/2161-0711.1000490
Copyright: © 2016 Dembo R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
We present the background, formulation, and implementation of an innovative health service at the front end of the juvenile justice system serving the serious, growing public health needs of justice involved youth-who bear a high burden of STD/HIV and other health problems. Involving multi-agency collaboration, the Health Coach Service seeks to address the youth health needs through health risk assessment and biological testing-with indicated followup testing, prevention, and neighborhood based treatment services. Through continuous monitoring of the Health Coach Service, we will be equipped to assess its feasibility, efficacy, and its real-world effectiveness and utility as a health-risk detection, prevention, and treatment paradigm.
Keywords
Health coach services; Juvenile justice
Introduction
The need for health services at the front end of the juvenile justice system
Juvenile justice involved youth remains an understudied and underserved population at markedly elevated risk for sexually transmitted infections, including HIV. While the juvenile justice system focuses on public safety, and seeks to identify and address risk factors that affect youth offense behavior [1-4], the system does not routinely direct attention to health issues, particularly sexually transmitted diseases, by identifying and treating infected youth [5] and providing evidence-based interventions designed to reduce the risk of STD/HIV acquisition and transmission [6].
In many jurisdictions, following arrest, youth are seen by probation officers, who can dismiss the case, handle the case informally (e.g., issue a warning), or move the case forward to juvenile court proceedings. A number of jurisdictions have developed centralized intake facilities, such as juvenile assessment centers, which conduct legal functions (such as booking), screening for substance use and mental health issues, and, with state attorney and/or comparable agency approval, place the youth in detention, on home arrest, or in a community diversion program [4]. Although, in principal, youths who are under the custody of juvenile authorities receive medical evaluation and needed care, these services vary widely in their availability, quality and range of coverage [5,7,8]. This is particularly the case for community-based services to which justice involved youth may be referred.
Providing sexual disease and related health screening as youth enter the front door of the juvenile justice system is urgently needed for several reasons. First, sexually transmitted diseases, such as Chlamydia and gonorrhea, are asymptomatic, and if left untreated, can have profound adverse medical consequences. Second, most youth following arrest, are released back the community and not placed in secure detention facilities. Statistics indicate approximately 80% of arrested youth are not detained [9]. Arrested youth whose sexual disease infections are not identified are at-risk of becoming “core transmitters” of STDs upon their return to the community [10]. Third, it is costeffective to provide medical treatment to infected youth at the early stages of disease rather than after the diseases have developed into more serious medical conditions.
To address these health concerns, we discuss an innovative, comprehensive health service approach to identify a range of health issues among youth soon after their arrest. These health issues include drug use, STDs, HIV, HCV, and depression. This new service links youth with effective treatment provided by a collaborating health department, local community-based family medical centers, and community-based behavioral health services. Referrals, treatment engagement, retention in care, and outcomes are monitored and tracked; and routine, six month follow-up interviews are administered. Among the unique features of this new service is its use, wherever possible, of biological data, using recent advances in microbiological testing, for diagnosis, assessment and treatment.
Although this is not an epidemiological report, we begin by reviewing important information on the prevalence and correlates of sexual risk behavior and sexually transmitted diseases among youth. This body of work informed the development and structure of the health service we discuss.
Key sexual risk behavior/sexually transmitted disease risk factors among youth substance use
Alcohol and marijuana remain the most frequently used drugs among American youth. Monitoring the Future (MTF) surveys on the prevalence and frequency of drug use indicates alcohol and marijuana Alcohol and marijuana remain the most frequently used drugs among American youth. Monitoring the Future (MTF) surveys on the prevalence and frequency of drug use indicates alcohol and marijuana continue to be the most prevalent substances used among adolescents in the U.S. [11]. Although use of alcohol has declined in recent years, prevalence rates remain high among the 8th grade, 10th grade, and 12th grade students, with 9.0% of 8th graders, 23.5% of 10th graders, and 37.4% of 12th graders reporting past 30 day use of alcohol.
According to the MTF survey, marijuana has been the most widely used illicit drug. Marijuana prevalence peaked in the late 1970’s at 51%, dropped markedly during the 1980’s, peaked again to around 40% in late 1990’s, declined slightly during the early 2000’s, and recently increased slightly in the 2010’s [11]. MTF survey data indicate 30 day prevalence rates of 6.5%, 16.6%, and 21.2% among 8th graders, 10th graders, and 12th graders, respectively; annual prevalence rates of 11.7% for 8th graders, 27.3% for 10th graders, and 35.1% for 12th graders were also found. Although data from the 2015 MTF survey indicate a leveling out in the annual prevalence of marijuana use, the percent of students perceiving regular use as “carrying a great risk of harm” continued to decline. Since perceived risk of harm has been found to be a deterrent to use, these results indicate adolescent marijuana use remains a key concern [12].
There is a substantial empirical database linking alcohol use to sexual risk behavior and sexually transmitted diseases [13-15], with binge drinking strongly associated with these adverse health outcomes [16]. Not surprisingly, alcohol use has been found to be related to HIV acquisition, with alcohol abusers being at markedly elevated risk of HIV infection [17].
Marijuana use is also associated with risky sexual behaviors, such as sex with partners of unknown HIV status, early initiation of sex, transactional sex (exchanging sex for money, drugs, food), and a high prevalence of condom-less sex. For example, Huang et al. identified, in a nationally representative sample of youths, five distinct trajectories of sexual risk; marijuana use was significantly and positively correlated with sexual risk at each age (wave of data) and increased sexual risktaking over time. Further, marijuana use is positively associated with STD and HIV acquisition.
The use of drugs such as cocaine and opiates is also related to sexual risk behavior and contracting STDs and HIV [18,19]. This is especially the case for IV drug users. Chronic drug users are particularly vulnerable to infectious diseases and are considered “core transmitters” [10].
Depression
Sexual risk behaviors and STD infection are associated with depressive symptoms among adolescents. For example, in a study using data from the National Longitudinal Study of Adolescent Health, Hallifors et al. used cluster analysis to identify sixteen subgroups of youth based on substance use and sexual risk behavior, and assessed differences in depression and suicidal ideation across these subgroups. Results indicated involvement in sexual activity heightened the risk of reporting major depression symptoms. Although girls were less likely to be involved in risk behavior, those who were involved had greater depression. Research involving justice-involved youth has found similar relationships between depression and sexual risk behavior [3]. Studies have not been consistent, as some studies have failed to identify an association between depression and sexual risks.
Thus, the direction of the association between sexual risk behaviors and depressive symptoms remains unclear. For instance, subsequent analyses using National Longitudinal Study of Adolescent Health data by Hallifors et al. indicated that engaging in sexual risk behavior and drug use increased the likelihood of future depression among adolescents, especially girls, but depression did not predict risky sexual and drug behaviors. In contrast, there is evidence to indicate that higher levels of depressive symptoms are a significant, longitudinal predictor of STD acquisition. More research is needed to clarify the association between sexual risk behavior and depression, and the mechanisms, including cognitive processes, underlying any identified relationships among depression, sexual risk behavior, and sexual disease status [20]. At the same time, however, screening for depression, sexual risk behavior, and their consequences remain critical public health needs.
Groups at higher risk of sexually transmitted diseases and their effects
Age: As noted earlier, adolescents and young adults constitute a disproportionately high number of persons with STDs, compared to adults, with persons 15-19 and 20-24 being most vulnerable [21]. In 2014, reported cases of Chlamydia and gonorrhea increased for the first time since 2006, with these STDs continuing to affect young people most seriously [22]. In addition, the CDC estimates that the rates of undiagnosed HIV cases is greatest among youth in the 13 to 24 year age range [23], with some 10,000 persons 13-24 being diagnosed with HIV in 2013 [22]. Routine HIV testing is recommended for all adolescents aged 13 and over.
Gender: Studies indicate girls are at greater risk of acquiring a sexually transmitted disease, and to experience its consequences [22,24-26], than boys-although increasing rates of STDs among boys also contributed to the overall STD increase in 2014. The CDC [27] observed a 40% prevalence of STDs among girls admitting to having sex. Young African American women, particularly those in the 15-24 age range, are disproportionately affected by HIV, accounting for 46% of all U.S. females with this disease [28,29]. Although African American adolescents are at heightened risk for HIV/AIDS, less than one-third report having an HIV test [30].
Race/Ethnicity: Although African Americans account for only 12% of the U.S. population, they were represented in over 46% of all HIV diagnoses in 2011 [28]. Higher rates of sexually transmitted diseases among African Americans are a co-factor facilitating acquisition and transmission of HIV. Many factors appear related to STD and HIV infection among African Americans, including having sex within their ethnic group, poverty (e.g., residential segregation, limited opportunities for advancement), stigma and discrimination, lack of access to healthcare, and high rates of imprisonment among African American males (with 36% of prison inmates in 2013 being African American [21,28]. In particular, multiple studies have documented the high prevalence rates of STDs and HIV among incarcerated youth [31,32].
Description of the Health Coach Service
The Health Coach Service is housed at a centralized intake facility located in a southeastern U.S. city, where all arrested youth are brought for justice system processing, psychosocial screening, and determination of release status (e.g., secure detention, home arrest, recommended for placement in a diversion program). As described elsewhere, the Juvenile Assessment Center (JAC) meets statutory requirements, as well as identifies and responds to the results of psychosocial screening indicating a need for follow-up evaluation and services.
Goals and focus of the Health Coach Service
There are four major goals for the Health Coach Service:
• Offer HIV evidence-based risk reduction information and education to youth using a gender- and developmentallyappropriate online curriculum.
• Provide rapid testing for HIV and other STDs, including Hepatitis C when indicated.
• Follow-up with youth and provide prompt, appropriate linkage to treatment for those who are drug involved, test positive for HIV and other STDs, or screen high depression inventory.
• Health Coaches will refer youth who report they do not have a “medical home” to a collaborating family health center, and monitor and track adolescents’ engagement and retention in care.
The Health Coach Service began on October 15th, 2015. Given the disproportionate risk of STD and HIV among girls [24,26], the Health Coach Services initially focused on girls processed at the JAC. All male youth wishing to be tested for STDs continued to receive such testing, and any indicated department of health follow-up care.
On February 4th, 2016 Health Coach Services were expanded to male youth. Since Florida public health statutes do not require youth 12 years of age or older to obtain informed consent for STD testing, we focused on this age range for girls, and 15-17 year old male youth. Few youth are excluded due to being under 12 years of age (<1%). Available data indicate most girls and boys processed at JAC are between 15 and 17 years of age (75%). Youth participating in Health Coach Services are asked to sign a consent form. Based on JAC booking data collected by the County Sheriff’s Office unit at the JAC, which operates the JAC secure wing, we estimate about 400 male and female youth per month will be processed at the JAC, and that approximately 80% will agree to receive Health Coach Services.
Health Coach Service process
Since August 2007, and in collaboration with the state health department, all JAC processed youth 12 years of age or older receive voluntary, free STD testing for Chlamydia and gonorrhea and indicated treatment follow-up. The new Health Coach Service is an add-on to this existing STD service.
Health Coaches are Department of Health trained, undergraduate degree holders working under the direction of a project manager. Health Coaches are selected based on their ability to interact with youth and to non-judgmentally discuss sexual behavior issues. They are on duty 11 AM to Midnight, Monday to Friday, during which period most youth enter the JAC.
The Health Coaches also share on-call responsibilities for weekends and holidays from 11 AM to Midnight. Although fewer youth are presented during these times, this gives the Health Coaches an opportunity to serve the majority of boys and girls entering the JAC.
County Sheriff Office detention deputies operate the secure wing at the JAC. In addition to providing for facility security, deputies complete a booking process for each youth that occurs immediately after youth enter the JAC secure wing, which includes the collection of basic demographic and contact information (e.g., address), electronic fingerprints, and a photograph. After this required process, each youth is approached by a Health Coach and invited to participate in the new service. Each youth is informed the Health Coach Service will involve the following:
• Collection of sociodemographic information (e.g., age, living arrangement)
• Information on alcohol and other substance use, including collecting a urine specimen for substance use analysis
• Split testing of the urine specimen for STDs (i.e., Chlamydia and gonorrhea), with free, confidential follow-up treatment, if indicated
• Screening for HIV, with follow-up, confirmatory testing and treatment
• Completion of a screen to identify a need for Hepatitis C testing; treatment of all positive youth is available
• Information on sexual behavior
• Information on depression [33]
• Linking youth with a primary health care physician, if they do not have one, at a local family health care center
• Referral to other follow-up health related services, if needed
• Completion of an online sexually transmitted disease riskreduction intervention following release from the JAC
• Randomly selected youth will receive a six month follow-up assessment. (A random sample of youth declining to receive Health Coach Services is also selected for follow-up.)
• Those randomly selected for follow-up assessment will receive a telephone interview to monitor their health status and health risk behavior
Each youth is informed that he/she will be eligible for one of five $100 gift cards to be determined in June of each year.
Youth interested in receiving Health Coach Services complete a consent form and receive Health Coach pre-counseling. The Florida Department of Health has trained the Health Coaches to administer health department standard pre- and post-counseling to youth, as well as follow other department protocols, such as post-JAC contact procedures.
The horizons intervention
Based on social cognitive theory and the theory of gender and power, Horizons is a CDC evidenced-based intervention designed to reduce sexually transmitted diseases (STDs), increase condom use, increase communication with male partners about safer sex and STDs, and increase male partners accessing STD services [34]. The curriculum seeks to foster a sense of cultural and gender pride and emphasize diverse factors contributing to girls’ STD/HIV risk, including individual factors (STD/HIV risk-reduction knowledge, perceived peer norms supportive of condom use, and condom use skills), relational factors (persuasive communication techniques to enhance male partner responsibility for condom use), sociocultural factors (encouragement to reduce douching), and structural factors (male partners’ access to services). Horizonswas initially developed for heterosexually active African American adolescent girls, and involved group sessions and follow-up phone contacts conducted by African American women health educators. It has since been produced in an online, multimedia, digital format.
For the Health Coach Service, horizons has been adapted for use among diverse cultural groups of male and female youth. Participating youth are asked to access a full online curriculum following their release from the JAC. Youth not having access to internet accessible PCs may also access Horizons at several community locations that provide internet-capable computers. They can also access horizons via smartphone.
Health Coach Service follow-up activities
The collected urine specimens are picked up by a courier each morning and transported to a department of health laboratory where the specimen is divided in half. One half of the specimen is tested by an on-site community agency for seven drugs (marijuana, cocaine, amphetamines, opiates, benzodiazepines, alcohol and spice). The drug test results are used to inform substance abuse treatment recommendations for the youth. The results are not used to place additional charges. The other half of the urine specimen is tested by the department of health for Chlamydia and gonorrhea. STD testing uses the FDA-approved nucleic acid amplification test (Aptima Combo 2, Gen-Probe) [35]. If a sample tests positive, results are shared with a department of health, community-based Disease Intervention Specialist, who in accordance with department policy, initiates contact tracing protocols to identify the youth, provide risk-reduction counseling, assess sexual contacts, and promptly engage the youth in treatment at the health department using standard-of-care therapeutic regimens.
Youth testing positive in a Health Coach administered OraSure HIV-1 Advanced Quick Test (oral swab) have their results shared confidentially with the health department. Department outreach workers seek out the youth for western blot test confirmation of the initial HIV test results, implement risk-reduction counseling, standard of care contact tracing protocols, and promptly engage youth in treatment. Youth determined to be at risk for Hepatitis C based on screening assessment, following department of health protocol, are referred to a collaborating family health center for HCV testing and, if positive, prompt treatment and risk-reduction counseling.
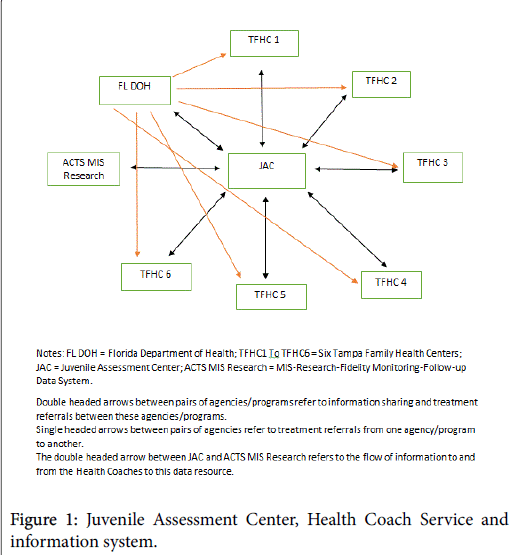
Collaborating community-based family health centers are key partners in this new service system. As Figure 1 shows, the Tampa Family Health Centers receive referrals from the department of health and JAC-based Health Coaches. Health Coach referrals are made to a designated family health center staff member, who contacts the youth and assigns him/her to a health center near his/her home. (The Tampa Family Health Centers are federally recognized and funded to provide services to low income families.)
Further referral, treatment engagement, retention, and service outcome (e.g., treatment received) information is shared with the Health Coaches for inclusion in a comprehensive medical, researchbased information system (RMIS) established for this new service. With the routine collection of individual data (e.g., drug use, STD and HIV status) and community-level data (e.g., increases in medical services delivered to youth in family health centers located in zip codes where JAC processed health coach youth are heavily concentrated), the RMIS permits the study of multi-level outcomes. It is important to emphasize that the sharing of health and related information among the department of health, family health centers, and Health Coaches is vital to successful identification and treatment of the health needs of youth. In this regard, ongoing data quality assessment of the RMIS is needed. It is performed by the Health Coach manager conducting daily checks on the quality of interaction between the Health Coaches and youth; and, among other responsibilities, daily review of the data entered by Health Coach staff-with prompt resolution of data entry anomalies.
JAC entry service follow-up information
In addition to the information collected by the Health Coaches on youth served at the JAC, post-JAC follow-up information (e.g., number of HIV+ or STD+ youth linked to treatment, number of youth completing the Horizons intervention program) is also obtained. With the collection of six month follow-up information discussed in the next section, a rich data system will be available to conduct studies providing timely data for diverse audiences.
Six month follow-up assessment with youth
Six months following the JAC entry date of each youth, a 10% random sample of youth participating in the Health Coach Service that month, as well as a 10% random sample of youth who did not participate, is selected for follow-up assessment by trained JAC Health Coach staff. Telephone interviews are completed within 30 days of the six month anniversary date of each youth’s processing at the JAC, and address the following topic areas: (a) alcohol/other drug use, (b) substance abuse treatment, (c) testing for STDs, (d) testing for HIV, (e) assignment to a primary care physician at a collaborating communitybased family health center, (f) receipt of health services, (g) completion of the online Horizons intervention program. In addition, for each youth, staff records the number of arrests during the six month followup period. With routine health service data that will be provided to the Health Coaches by the department of health and other collaborating family health centers, we shall be able to complete comprehensive outcome analyses of this service at the individual and community levels.
Health Coach Service advisory board
An Advisory Board has been established to provide ongoing advice and support to the Health Coach Service. Members include representatives from the Department of Health, Tampa Family Health Centers, and the detention center. These meetings are invaluable in addressing and improving service linkage, collaboration, and information sharing procedures.
Informing the field, stakeholders, and the community
Numerous research studies are planned (e.g. psychometric studies of the depression measure; multi-level [involving the youths’ zip codes] analyses of the STD and HIV test results, and GIS analyses of the prevalence of drug use, depression, STD and HIV). A multi-group study of depression among Health Coach served youth has already been completed [36]. In addition, plans are in place to prepare and periodically disseminate anonymized drug and STD/HIV test result summary reports to a range of community stakeholders, including the department of juvenile justice, the courts, behavioral health care providers, school officials, and law enforcement. The purposes of these reports include informing the community about health issues presented by justice involved youth, identifying new health issues requiring service response (e.g. identifying new drugs of abuse), and documenting the need for new or expanded services to address any increased incidence or prevalence of specific health issues. The comprehensive information system will inform the work of various constituencies and interest groups in their efforts to improve the community service delivery system.
Evidence of need for Health Coach Services
A report on girls receiving health coach services from October 19, 2015 through May 31, 2016, and boys receiving these services from February 4th, 2016 through May 31, 2016, highlights the serious need for them. The current, brief summary reports information relating to 777 first admission male (n=399) and female (n=378) youth 12 years of age or above during the period of time noted above, who voluntarily enrolled in the JAC Health Coach Service at the Hillsborough JAC. The youth served represent a high, 76.7%, participation rate (777 of 1013 first admissions during this time period), and reflects their perceived value of this service. For this report, we have included first admission information only on youth admitted two or more times (8% of the youth).
The results we report are arrayed across JAC release status categories (secure detention, home detention, outright release), which reflect youth risk status based on completion of a Detention Risk Assessment Instrument (DRAI). Although this report focuses on individual youth demographic and public health characteristics, it is planned for future reports to include follow-up service information on youth referred to various community agencies (e.g., the Department of Health, Tampa Family Health Centers), as well as our on-site therapist.
Demographics: Approximately equal numbers of male (n=399) and female (n=378) youth are represented in the data used for this report. 63% of male youth were placed in secure detention or placed on home detention, compared to 38% of female youth-who were more often released outright.
The youth averaged nearly 16 years of age in each JAC release category. Nearly 70% of youth released to secure detention or home detention were African American, compared to 46% of youth who were released outright. Outright release youth contained a larger percent of Hispanic and Caucasian youth.
Depression: The youths’ responses to our evidence-based measure of depression indicate an elevated level of depression exists among some 20% of youth placed in secure detention, 14% of youth placed on home detention, and 22% of youth given outright release. Depression is a major concern as a mental health issue, but also in its high association with drug use and sexual risk behaviors [36,37].
Drug use: The evidence based, Texas Christian University (TCU) self-report drug use instrument [38] we use indicated the vast majority of youth (85% or more) in each JAC release status category reported no symptoms of drug dependence, with approximately 10% of youth in each release category being in the mild or moderate drug dependence groups. Relatively few youth reported symptoms of severe drug dependence.
Stressing the value of urine testing, the self-report drug use results appear somewhat inconsistent with the youth’s UA test results, and indicate 62% of youth placed in secure detention, 53% of youth placed on home detention, and 45% of youth released outright were UA positive for marijuana. Small percentages of youth were found to be UA positive for the other drugs we tested for. Consistent with other studies of justice involved youth, it is likely the self-report drug use data underestimate the youths’ drug involvement, which appears substantial.
STD and HIV test results: High rates of STDs were found among the 657 youth who agreed to STD testing, with 14% of youth placed in secure detention, 12% of youth placed on home detention, and 7% of youth released outright testing positive for Chlamydia, gonorrhea, or both diseases. The prevalence rates are much higher among youth entering the justice system, (i.e. placed in secure detention or on home detention), than youth released outright to the community. Untreated STD positive youth are at risk of becoming transmitters of STDs to others, especially given the asymptomatic nature of these diseases. Further, these rates are significantly higher than the prevalence rates for these diseases among similar aged youth in the general Hillsborough County adolescent population. The STD positive rates we found are disturbingly high, not only in themselves, but because they reflect an elevated risk of acquiring HIV/AIDS.
No initial positive HIV results were found among youth consenting to HIV Quick Testing (via mouth swab).
These data highlight: (1) Significant drug use, STD prevalence and depression issues among youth receiving Health Coach Services, and (2) Document the continuing need for this valuable health resource for our youth, who often lack the resources to access health care.
Vision for the Future
Based on the results of department of health STD testing among JAC processed youth, with identification of high rates of Chlamydia and gonorrhea among boys and, especially, girls, we anticipate continued identification of elevated levels of STDs. Testing for HIV and Hepatitis C is expected to identify: (1) Additional sexually transmitted diseases that require prompt treatment and risk-reduction counseling, and (2) Associations among depression, drug use and these sexually transmitted diseases. Among the exciting aspects of the Health Coach Service are the expanded collaboration with the department of health, linking youth needing follow-up medical services with community-based, family health centers in close proximity to where youth reside, and the exposure of Health Coach served youth to an evidence-based STD/HIV intervention program.
We anticipated the results of this pilot effort will lead to the expansion of this service to other JACs. This expansion did occur at the Polk County JAC in May 2016. Expansion of Health Coach Services to Polk County, FL will improve the public health of that community.
There has been an increase in community pre-arrest diversion programs for youth encountering a law enforcement officer for engaging in minor misdemeanor offenses, most often petty theft. Such youth, who represent another high risk group in the community, are assigned to a program located in the county courthouse, where they receive substance use and mental health screening and referral to community-based treatment programs for follow-up services. They do not receive a comprehensive, biologically-based screening and health assessment, together with indicated risk-reduction counseling, treatment and medical service follow-up, provided to JAC Health Coach Service recipients. Expansion of Health Coach Services to this important at-risk group would further improve the public health of our community.
As noted earlier, major concerns of Health Coach Services are prevention and early intervention, with quick linkage to needed medical, public health and behavioral health care. These concerns converge well with key emphases in the recently released U.S. Surgeon General’s report on Facing Addiction in America [39].
We plan to continue current efforts to serve as a public health monitoring station. These efforts include: (1) collaboration with the University of Maryland, Community Drug Early Warning System project to identify new drugs of abuse, and include testing for new metabolites in our UA testing protocol—as we have done for the synthetic spice metabolite UR-144 [40], and (2) collaborate with other scientists to identify, test, and evaluate the efficacy and feasibility of collecting microbiological markers to assess depression.
We are hoping the service model we have developed and are implementing will be extended to all youth entering the justice system throughout our state and elsewhere. Should this opportunity occur, we plan to provide training and implementation support to requesting jurisdictions in other locations, so they can better identify and address the public health needs of justice involved youth at the front door of their justice systems.
Conclusions
The Health Coach Service represents an innovative approach that responds to a growing and urgent public health need for vulnerable juvenile justice involved youth who are disproportionately impacted by STD/HIV and other health problems. Through continuous monitoring of the Health Coach Service, we will be equipped to assess its feasibility, efficacy, and its real-world effectiveness and utility as a health-risk detection, prevention, and treatment paradigm.
References
- Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA (2002) Psychiatric disorders in youth in juvenile detention. Arch Gen Psychiatry 59: 1133-1143.
- Teplin LA, Abram KM, McClelland GM, Mericle AA, Dulcan MK, et al. (2006) Psychiatric disorders of youth in detention. Juvenile Justice Bulletin, Washington DC, USA.
- Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, et al. (2005) Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. PsychiatrServ 56: 823-828.
- Dembo R, Walters W (2012) Juvenile assessment centers: Early intervention with youth involved in drug use. Civic Research Institute, Kingston, USA, pp: 15-28.
- Belenko S, Dembo R, Rollie M, Childs K, Salvatore C (2009) Detecting, preventing, and treating sexually transmitted diseases among adolescent arrestees: An unmet public health need. Am J Public Health 99: 1032-1041.
- Golzari M, Hunt SJ, Anoshiravani A (2006) The health status of youth in juvenile detention facilities. J Adolesc Health 38: 776-782.
- Newacheck PW, Hung YY, Park MJ, Brindis CD, Irwin CE (2003) Disparities in adolescent health and health care: does socioeconomic status matter? Health Serv Res 38: 1235-1252.
- Elster A, Jarosik J, vanGeest J, Fleming M (2005) Racial and ethnic disparities in health care for adolescents: a systematic review of the literature (2005). Arch PediatrAdolesc Med 157: 867-874.
- Snyder HN, Sickmund M (2006) Juvenile offenders and victims: 2006 national report. Office of Juvenile Justice and Delinquency Prevention, Washington DC, USA.
- Office of National Drug Control Policy (1999) America’s drug use profile: Consequences of illegal drug use.
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Miech RA (2015) Monitoring the Future national survey results on drug use: 1975-2014: Overview, key findings on adolescent drug use. Institute for Social Research, University of Michigan, Ann Arbor, USA.
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Miech RA (2016) Monitoring the Future national survey results on adolescent drug use: Overview of key findings, 2015. Institute for Social Research, University of Michigan, Ann Arbor, USA.
- Windle M (1999) Alcohol use among adolescents. Sage, USA.
- Santelli JS, Robin L, Brener ND, Lowry R (2001) Timing of alcohol and other drug use and sexual risk behavior among unmarried adolescents and young adults. FamPlannPerspect 33: 200-205.
- Seth P, Sales JM, DiClemente RJ, Wingood GM, Rose E, et al. (2011) Longitudinal examination of alcohol use: A predictor of risky sexual behavior among African-American female adolescents. Sex Transm Dis 38: 96-101.
- Hutton HE, McCaul ME, Santora PB, Erbelding EJ (2008) The relationships between recent alcohol use and sexual behavior. Alcohol ClinExp Res 32: 2008-2015.
- National Institute on Alcohol and Alcohol Abuse (2012) Alcohol alert.
- DeHovitz JA, Kelly P, Feldman J, Sierra MF, Clarke L, et al. (1994) Sexually transmitted diseases, sexual behavior, and cocaine use in inner-city women. Am J Epidemiol 140: 1125-1134.
- Hser Y, Chou C, Hoffman V, Anglin MD (1999) Cocaine use and high-risk sexual behavior among STD clinic patients. Sex Transm Dis 26: 82-86.
- Shrier LA (2009) Depression and sexual risk behavior in adolescents. Jossey-Bass, USA, pp. 359-374.
- Salazar LF, Santelli J, Crosby S, DiClemente RJ (2009) Sexually transmitted disease transmission and pregnancy among adolescents. Jossey-Bass, USA, pp: 275-302.
- Centers for Disease Control and Prevention (2015) Sexual risk behavior: HIV, STD, & teen pregnancy prevention.
- Centers for Disease Control and Prevention (2012) Teens and the HIV/AIDS epidemic.
- Centers for Disease Control and Prevention (2013) STDs in adolescents and young adults.
- Centers for Disease Control and Prevention (2014) Sexually transmitted disease surveillance.
- Dembo R, Belenko S, Childs K, Wareham J (2009) Drug use and sexually transmitted diseases among female and male arrested youths. J Behav Med 32: 129-141.
- Centers for Disease Control and Prevention (2008) 2008 STD prevention conference- press release march 11, 2008.
- AVERT (2014) HIV & AIDS among africanamericans.
- Dellar RC, Dlamini S, Karim QA (2015) Adolescent girls and young women: Key populations for HIV epidemic control. J Int AIDS Soc 18: 19408.
- Swenson RR, Rizzo CJ, Brown LK, Payne N, DiClemente RJ, et al. (2009) Prevalence and correlates of HIV testing among sexually active African American adolescents in 4 U.S. cities. Sex Transm Dis 36: 584-591.
- Freudenberg, N, (2009). Incarcerated and delinquent youth. Jossey-Bass, USA, pp: 339-358.
- Centers for Disease Control and Prevention (2010) STDs in persons entering corrections facilities.
- Melchior LA, Huba GJ, Brown VB, Reback CJ (1993) A short depression index for women. Educational and Psychological Measurement 53: 1117-1125.
- DiClemente RJ, Wingood GM, Rose ES, Sales JM, Lang DL, et al. (2009) Efficacy of STD/HIV sexual risk-reduction intervention for African American adolescent females seeking sexual health services: A randomized controlled trial. Arch PediatrAdolesc Med 163:1112-1121.
- Gen-Probe, Inc. Aptima for CT and GC.
- Dembo R, Faber J, Cristiano J, DiClemente RJ, Terminello A (2016) Multi-group study of depression among youth entering the juvenile justice system. Foundations of Behavioral Health. Springer, New York.
- Dembo R, Krupa J, Wareham J, Schmeidler J, DiClemente RJ (2016) A multi-group, longitudinal study of truant youth marijuana use, depression, and STD–associated sexual risk behavior. J Child Adol Sub Abuse.
- Texas Christian University, Institute of Behavioral Research (2014) TCUDS V- TCU drug screen v. Institute of Behavioral Research, Fort Worth, Texas, USA.
- U.S. Department of Health and Human Services (2016) Facing addiction in america: the surgeon general’s report on alcohol, drugs, and health. US Department of HHS, Washington DC, USA.
- Wish ED, Billing AS, Artigiani EE (2015) Community drug early warning system: The cdewsâ?2 replication study office of national drug control Policy. Executive Office of the President, Washington DC, USA.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 3741
- [From(publication date):
December-2016 - Nov 23, 2024] - Breakdown by view type
- HTML page views : 3036
- PDF downloads : 705